Uniportal video-assisted thoracoscopic major pulmonary resections
Introduction
One of the most important breakthroughs in thoracic surgery has been the development of video-assisted thoracic surgery (VATS) (1). It has revolutionized how surgeons treat thoracic diseases (2). In the early 1990s, it began to be used to perform major lung resections (3), starting an era of continuous growth in minimally invasive thoracic surgery (MITS).
The last stop in the quest for a better minimally invasive procedure is the single port approach or uniportal VATS. Rocco was the first one to describe the approach for minor thoracic procedures (4) González-Rivas and colleagues were the first team to perform an uniportal VATS lobectomy in La Coruña in 2010 (5) Since then, the technique has had an exponential widespread around the world, being performed by more and more units every year thanks to numerous workshops and training programs. (6)
Technology improvement in high definition cameras, instrumentation, staplers and energy devices has allowed that uniportal VATS can also be implemented as an approach not only for standard cases but for advance tumors and for vascular and bronchial reconstruction (7).
Uniportal VATS lobectomies can be perform safely by thoracic surgeons around the world as long as they follow the proper steps in order to learn the technique, gain experience with it and carried it out in their own units.
Patient selection and workup
When it comes to patient selection there are two scenarios, one is for the experience uniportal VATS surgeon in a high volume center and the other is for the surgeon in the learning curve or that has just surpass it.
For the experience surgeon, very complex and technically difficult cases can be done successfully, including sleeve lobectomies, vascular reconstruction or tumors invading the chest Wall (8). With exception of tumor size (tumors bigger than 8 cm are difficult to take out without rib spreading) (9), patients that are candidates for a major lung resection with an open approach should be eligible for a single port approach. And this is one of the key things to keep in mind about this technique, it does not compromise oncologic principles and basically carry out the same procedure as in open surgery but through a minimally invasive approach with VATS instruments. The complexity of the case although may be challenging, does not mean a contraindication in this scenario.
VATS surgeons that are inexperience or just surpass the learning curve should focus on early stage lung cancer lobectomies and avoid complex cases like reinterventions, sleeve resections, big tumor or cases with lots of benign lymphadenopathy around the hilum or fissure in order to avoid complications such as bleeding during the surgery.
During the work up, there are two very important aspects that will inform the surgeon of potential difficulties in a particular case. First patient previous history of tuberculosis, bronchiectasis or previous surgery should prepare the surgeon for adhesions and lymphadenopathies that will make dissection especially difficult. Second the CT image will show big lymph nodes in the probable site of dissection, big lung tumors or anatomical relations that will make the procedure especially difficult to finish without conversion (7).
Timely conversion should never be considered a complication but an appropriate step during a VATS procedure.
Pre-operative preparation
Patients that are candidates for a uniportal VATS lobectomy can undergo the same institutional protocols as other approaches lobectomies (multiport or open lobectomies) and the patient has to know that conversion to an open procedure is a possibility during the procedure as a step to avoid complications or risky situations.
It is appropriate to accompany single port MITS with fast track protocols that should began when the surgeon interview the patient in the outpatient clinic managing patient expectations and addressing their concerns. An educational program of respiratory exercises and smoke cessation will be helpful for the postoperative recovery (10).
When the surgeon is experience to do so, a pre-operative conference with the anesthesiologist discussing the possibility of a non-intubated uniportal VATS lobectomy is important for a good coordination and safe planning for the surgery.
Equipment preference
Optimal equipment can facilitate and made more comfortable the procedure for the surgeon. The ideal equipment necessary to perform a major lung resection includes:
- 30-degree lens high definition camera thoracoscope: provides a very detailed image and permits the assistant to move the angle of the camera to obtain the appropriate visualization around structures during visualization;
- Distally mounted charge couple device (CCD): it reduces the fighting between the surgeon and the assistant (11);
- Instruments with distal and proximal articulation: a complete set of instruments such as the one show in Figure 1 allows the surgeon to do the surgery without having troubles with the incision, since only the fixed part of the instrument is in contact with it during dissection (Figure 1);
- Wound retractor: it is not always necessary, although it might help to prevent camera smearing in fat patients or with inexperience assistants;
- Reticulated staplers: the angulation of the staplers makes it easy to pass the structure, avoiding tension and unnecessary risks during this step;
- Vascular clips (click a-V Grena): for vessel when the angle for vascular division is difficult, also for small segmental branches of the pulmonary artery that can be safely divided using this clips;
- Energy devices: they permit to keep the operative field clean and avoid unnecessary bleeding from small vessels in fatty tissues or around lymph nodes. During lymph node dissection can avoid lymph leaking after the surgery.

Although the equipment mentioned above is the ideal one in the present to perform and uniportal VATS lobectomy it is not mandatory, the surgery can be performed with conventional VATS instruments (6), but with more technical difficulty.
Role of team members
The surgeon and the assistant must be positioned in the same side, in order for them to share the same view and work in coordination (Figure 2). The surgeon should be position in front of the incision, with the monitor directly in front, at the level of the eyes. In this way the surgeon avoids to take uncomfortable positions during the whole surgery. The assistant has to be much focused in keeping the camera in the posterior part of the incision and avoid lens smearing. During the surgery the assistant can change position between the left and right side of the surgeon in order to get the best angle of visualization.
The nurse should be placed in the other side of the patient, taking care not to obscure the visualization of the monitor.
The anesthesiologist has to be communicating with the surgeon during the procedure, in order to avoid unexpected movement (cough) during critical dissection of vessels. When it is a non-intubated procedure, the coordination during the surgery is mandatory and requires for a very close control of the condition of the patient.
Procedure
In uniportal VATS, is important that the surgeon maintain comfortable positions during the surgery in order to avoid fatigue. The best way to achieve this is in a way remembering that the surgeon is mimicking open surgery and should reproduce this condition. For example, is better to position the monitor in front of the surgeon at the level of his eyes, instead of putting it in near the head of the patient, because that will make the surgeon keep his head turn to this side during the entire procedure. The assistant should be positioned at the same side of the surgeon so they will share the same vision and coordinate better their movements.
The patient is position in lateral decubitus, and the procedure can be done under general anesthesia with double lumen intubation or without intubation (only by expert uniportal surgeons). The surgical table can be move away or to the surgeon in order to help in the exposure of structures and lymph node stations, since by gravity the lung is pull away from the operative field.
The incision is located at the 5th intercostal space, in the anterior position of the mid axillary line, although sometimes the 4th intercostal space can be used for upper lobes. Trocar is not needed for uniportal VATS, so nerve damaged by compression is minimized and space available in the incision maximized.
The role of the camera man is very important and difficult, because in order for the surgeon to be comfortable the assistant has to sometimes take positions that are demanding and at the same time get the right view of the surgical field, which requires a learning curve also and a lot of team work to be correct.
It is also important to remember that the camera should always be in the posterior part of the port, and the instruments enter the thoracic cavity from below, in this way resembling the eye and hand configuration as open surgery.
The approach to the target lesion is very similar as the one use in the open technique, because the visualization occurs along the same axis (12) and the angles of vision require performing a safe and detailed dissection can be obtained by moving the angle of the 30-degree lens camera (5,6).
During the entire procedure the surgeon must perform bimanual instrumentation, making the exposure and dissection better and easier. The retraction has to be carried out by the assistant, allowing the surgeon to use both hands and instrument for dissection.
The technique for upper lobectomies usually begins by dividing the first branches of the pulmonary artery, creating space and avoiding obstruction for the stapler for the vein division that comes afterwards. Then the bronchus as dissected and divided and the fissure is usually complete at last. For lower lobectomies the procedure usually begins with the pulmonary ligament, the inferior pulmonary vein, then the pulmonary artery, bronchus and fissure at last.
Vessels are usually divided with stapler, but vascular clips can also be used. For bronchus and fissure division staplers are routinely the choice.
The specimen can be remove using and endo-bag or even a glove, taking care not rupture it in order to avoid spilling of the specimen that could compromise oncologic results. If a wound retractor was used for the surgery is better to removed it prior to take out the specimen in a bag, because to keep it in place could make this step more difficult since it can reduce the space or flexibility of the tissues in the wound.
At the end of the procedure the three intercostal spaces are infiltrated with bupivacaine under direct vision, usually the space of the incision and the one below and up from it.
Surgical steps for each lobe
Right lower lobectomy
The procedure usually begins with the dissection of the inferior pulmonary ligament, the lobe can be retracted upwards by the assistant and the surgeon use the sucker to put aside the diaphragm and the ligament divide with energy devices or cautery. Then posterior mediastinal pleura can be divided up until the fissure; this step will help make easier to pass the vein and to dissect the artery and separate it from lung parenchyma in fissure less technique. After the posterior pleura is dissected the vein is dissected and divided using a vascular stapler with a reticulation, a tie or the sucker can be used to help the anvil of the stapler pass the structure.
The next step is to dissect the artery that is done from anterior to posterior. It is not difficult when the fissure is complete because the surgeon just have to divide the visceral pleura from the artery, but when the fissure is incomplete it has to be perform with the fissure less technique. The dissection has to begin in the space between the inferior and medial pulmonary vein, then go upwards to encounter the bronchus, and just above it find the artery. Dissection above the artery will create the plane to put the stapler and complete the fissure (care must be taken to avoid injury to middle lobe artery). The artery can be divided after in one step if it can be pass easily or first dividing the basilar branch will allow a better exposure of sixth segment artery(can be divided using a clip). The last step of the lobectomy is dividing the bronchus in which is important a good retraction and correctly identifying the middle lobe bronchus to avoid damage to it during transection of the lower lobe bronchus.
In cases of very difficult fissures, such as bronchiectasis or thick incomplete fissures the best way is to perform a fissure less technique, starting with the ligament, then the inferior pulmonary vein, bronchus, artery and at last the fissure. Correctly identifying middle lobe structures would avoid injuries to them during transection.
Middle lobectomy
This lobectomy can be technically difficult in uniportal VATS, since the angles for division and dissection of the structures can be tricky. The lung must be retracted up and backwards by the assistant. The procedure began by identifying the middle lobe vein, dissecting it. When the major fissure is incomplete, the stapler can be put in the space between the middle and lower lobe vein, which would facilitate passing the middle lobe vein after with the stapler. If a safe angle cannot be obtain with the stapler a vascular clip (a-V Grena) can be used to divide the vein. The next step is to divide the bronchus taking care not to injure the artery that is just behind. The artery is staple next and at last the anterior portion of the minor fissure and the posterior portion of the major fissure.
Right upper lobectomy
The dissection usually begins with the artery, identifying the anterior arterial trunk and then dividing it with the stapler. This step facilitates to divide the vein after since it helps to obtain a better angle by removing the obstruction of the artery. The right upper bronchus will be expose along with the posterior ascending artery, so the surgeon can choose to divide the one that is better exposed in that moment. The posterior ascending artery can be stapled or divided using a clip and the bronchus divided using a stapler. Care must be taken when passing the bronchus to avoid damage to the azygos vein. At last the fissure can be divided using a stapler, always being sure that the stumps are not in the jaws of the stapler but in the lobe that is going to be resected. When the artery is occult because of an incomplete fissure the best way to expose it is to dissect between the middle and upper lobe vein, the bronchus will be expose and just above it the artery can be identified. It is safe to dissect above the plane between the artery and lung parenchyma, and to staple above the artery would avoid injuries to other structures and permit to complete the fissure. It is important to avoid vigorous retraction of the lobe before dividing the posterior ascending artery, because it might rupture and is not and unusual cause of bleeding and conversion when performed by inexperience surgeons.
Left lower lobectomy
The steps to complete a left lower lobectomy are very similar as those uses to complete a right lower lobectomy. The surgery begins by dissecting the pulmonary ligament and continues to dissect the posterior visceral pleura until the fissure, the plane should be close to the lung parenchyma to avoid injury to surrounding structures. The next step is to divide the lower lobe vein. When dissecting the artery care must be taken to identify the lingular artery so it will not be injure when the lower lobe artery is stapled. In case of incomplete fissure the surgeon can use the same maneuver to find the artery as in the right lower lobe. Dissect the space between the upper and lower vein, the artery will be just above the bronchus. The staple can be safely placed just above the artery to divide the lung in the fissure.
Left upper lobectomy
The left upper lobectomy should be carried out by a surgeon that has prior experience with uniportal vascular dissection, stapling, ligation and that has successfully performed other uniportal lobectomies, specially a right upper lobectomy.
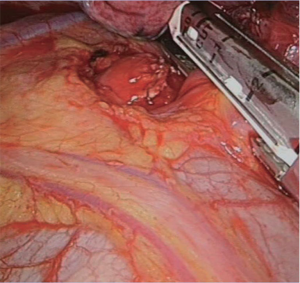
This lobectomy, along with the middle lobe lobectomy are perhaps the most difficult ones to perform in uniportal VATS, but the risk of bleeding secondary to vascular injury is more frequent an important in the left upper lobectomy. This is especially true in two steps, when dissecting the anterior trunk an injury can be done to the base of the artery by traction and when passing the stapler through the vein, without good exposure and traction the anvil can injure the pulmonary artery behind, causing a major bleeding. A tie can be used to retract the vein or the sucker pass through the space in order to facilitate the step and avoid this injury (Figure 3).
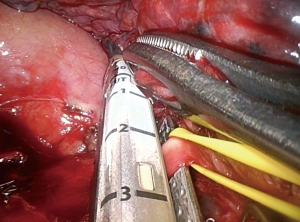
The dissection begins with the anterior trunk, a key maneuver is to expose to posterior part of the trunk before trying to pass it, because it avoids unnecessary traction to the vessel. After dividing the trunk the vein can be dissected ant then staple with a reticulated endostapler, avoiding injury to the pulmonary artery behind with the anvil of the stapler (Figure 4). To facilitate this step is important to dissect the vein as distally as possible. The next step is to dissect the fissure, which can be easy when is complete or requires identifying the artery between the upper and lower lobe vein in order to complete it. Lingular artery and the rest of the branches can be ligated, staple or divided using a vascular clip. The last step is the bronchus, which is easy if all the vascular structures are divided, but is more difficult if the lingular artery is not divided, because is just behind the bronchus. Dividing the bronchus with scissors or using a TA are maneuvers needed to complete this task. When cut the bronchus can be closed with sutures or staplers.
Lymphadenectomy
A complete lymph node dissection that follows the same oncologic principles as conventional VATS or open surgery can be performed. In block resection of the lymph nodes must be pursued and energy devices are especially helpful to maintain a clean operative field.
The surgical table can be move in order to facilitate visualization of lymph node stations. When dissecting station 7, the table can be moved anteriorly, and sponge stick can be used by the assistant to retract the lung and expose station 7. This will provide and excellent visualization and allow the surgeon to use both hands to remove the lymph nodes. In the right side care must be taken to retract away the esophagus in order to avoid injury to it.
For paratracheal lymph node dissection, the patient should be placed in anti-trendelenburg position, and the pleura below the azygos vein dissect, then remove the lymph nodes and fatty tissue in block by dissecting it away from the superior vena cava, vagus nerve. The lymph nodes then can be finally removed from remaining attachments by opening the pleura above and pulling them up.
For the aortopulmonary window, exposure is also improved in anti-trendelenburg position, dissection should avoid injury to the recurrent laryngeal nerve.
Post-operative management
Fast track protocols are important in order to maximize the benefits of a uniportal VATS approach. The patient can resume oral feeding the same day of the surgery and can initiate walking with help. The chest tube can be removed in absence of bleeding and air leak. Respiratory rehabilitation should start from the same postoperative day and incentive in spirometry must be reinforced. In case of no intubated lobectomies studies suggest patients can recover faster and resume ordinary activities sooner.
Tips and tricks
- Maintain always ergonomic positions in order to avoid fatigue;
- Keep the camera in the posterior part of the incision;
- The assistant must perform the retraction of the lobe so that the surgeon perform bimanual instrumentation;
- To optimized exposure, the surgical table can be move in some steps of the surgery, especially in lymph node dissection;
- In upper lobectomies dividing the anterior trunk first helps to facilitate the division of the vein;
- Using a tie or the sucker to facilitate the passing of the stapler when dividing the vein are key maneuvers to avoid injury to the artery in upper lobes;
- In incomplete fissures the artery can be located by dissecting upwards from the space between lobes veins, creating a safe plane top putt he staple and complete the fissure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Rocco G, Martin-Ucar A, Passera E.. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5 Suppl 3:S234-45. [PubMed]
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23.
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Sihoe AD, Chawla S, Paul S, et al. Technique for delivering large tumors in video-assisted thoracoscopic lobectomy. Asian Cardiovasc Thorac Ann 2014;22:319-28. [Crossref] [PubMed]
- Das-Neves-Pereira JC, Bagan P, Coimbra-Israel AP, et al. Fast-track rehabilitation for lung cancer lobectomy: a five-year experience. Eur J Cardiothorac Surg 2009;36:383-91; discussion 391-2. [Crossref] [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. ScientificWorldJournal 2012;2012:780842.
- Bertolaccini L, Rocco G, Viti A, Terzi A.. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
Cite this article as: Guido Guerrero W, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic major pulmonary resections. J Vis Surg 2016;2:85.