Heritage of the late Professor Tsuguo Naruke
Preface
Dr. Tsuguo Naruke (Figure 1) was a great lung cancer surgeon, and a pioneer of thoracoscopic surgery in the world.
It has been already 10 years since Professor Tsuguo Naruke expired on May 20, 2006. He had been primarily a chest surgeon in National Cancer Center Hospital in Tokyo for more than 30 years. Practicing lung cancer surgery as a most prominent leader in Japan, Asia, and worldwide, he was also a pioneer of thoracoscopic surgery for lung cancer. Dr. Naruke started brand new thoracoscopic surgery when he was 58 years old, with an inspiration that thoracoscopic surgery had infinite possibilities and must be a mainstream in the future (Figure 2).
His history on video-assisted thoracoscopic surgery (VATS) is that of Japan in its early days. Dr. Naruke first started video-assisted thoracoscopic wedge resection in March 24, 1992. Then he advanced to video-assisted thoracoscopic lobectomy in June 1, 1993.
Meanwhile, due to his effort, thoracoscopic surgery was approved by Ministry of Public Health and Welfare as a high technology medicine in July 1, 1993, as well a reimbursed treatment modality under the National Health Insurance System on April 1, 1994.
Details concerning thoracoscopic surgery
On starting, he established a setting for thoracoscopic surgery (Figure 3). His system includes the most important issues for thoracoscopic surgery, and mostly still available so far. Initially, he made up two aspects of thoracoscopy. One is exploratory thoracoscopy, or VATS exploration, as a diagnostic tool and the other is therapeutic thoracoscopy as a surgical therapeutic tool.
Exploratory thoracoscopy
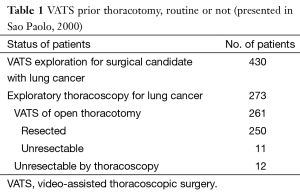
Dr. Naruke emphasized the value for VATS exploration for lung cancer.
Unique features of VATS exploration over routine staging procedures:
- The only one modality that allows complete visualization of the pleural space;
- Possible to perform various interventional procedures under VATS guidance;
- Associated with low morbidity and mortality.
VATS exploration for histologically proven or suspected lung cancer patients:
- Definitive histologic (cytologic) diagnosis for suspected lung cancer of undetermined histology;
- Definitive staging and detection of inoperable factors.
He showed effectiveness of VATS exploration (Table 1) and concluded that VATS exploration should be added to the conventional evaluation method for pretherapeutic patients with lung cancer. He also showed that thoracoscopic staging for lung cancer is a safe and effective procedure (1).
Full table
Thoracoscopic wedge resection
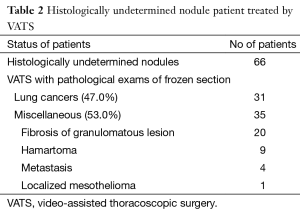
Dr. Naruke first started from video-assisted thoracoscopic wedge resection of the peripheral lung tumor in March 24, 1992. Then he experienced histologically undetermined nodule patient treated by VATS (Table 2).
Full table
Thoracoscopic lobectomy
Dr. Naruke continually developed thoracoscopic lobectomy technique and first started Video-assisted thoracoscopic lobectomy in June 1, 1993. Since then he underwent many thoracoscopic lobectomies which includes 2–3 cm Incisions, 6–7 cm “Utility or Access” thoracotomy incision, stapler of DK forceps-vein, artery, bronchus, lymph node dissection or sampling.
As an ancestor, Dr. Naruke requested below to those who practice this surgery:
- Long training;
- Wide experience;
- Skillfulness;
- Perseverance of patience;
- Good assistance.
Academic contribution
He founded a Society of Thoracoscopic Surgery of Japan, and the first annual meeting is held on October 9, 1992 in Tokyo and he continued to host the meeting until 1996.
Dr. Naruke also hosted the 11th Annual Meeting of Japan Society for Endoscopic Surgery in 1998 (Figure 4). Afterwards, he founded the Japanese Society of Thoracoscopic Surgery in 2001.
This society was taken over by Dr. Toshiaki Morikawa 1 year after his decease.
Professor Naruke, his personal issue
After finishing his final regular position in National Cancer Center Hospital of Japan as Vice-president at the age of 65, Dr. Naruke moved to Saiseikai General Hospital, a nearby base hospital, as a consultant. He still or more aggressively continued thoracoscopic surgery, and was also invited for surgery and lecture from all over the world.
Actually, Dr. Naruke was eternally the most conscientious Lung Cancer Surgeon till his decease.
Personally, the author was a resident of Chest Surgery in National Cancer Center Hospital through 1975–1978. During my residency, Dr. Naruke was my supervisor. In my memory, he was really a modest kind, respected, and shy person. He had never criticized other people.
On the other hand, he had very positive and active attitude to medical issues and no compromise in his patients. He concentrated his everything on surgery.
Especially he was a good sportsman of Judo, and a city runner. He never drunk, instead, he cooked sweets.
After finishing my residency, he made good communication with me, and let me attend many medical or government related congresses.
While establishing Japanese Society of Thoracoscopic Surgery in 2001, to my honor, I could assist his work.
More issues
By 1990’s, Professor Tsuguo Naruke had established his marks.
Lymph node mapping in the chest—“Naruke Map” (2) (Figure 5), developing complex procedure of Broncho-plasty (3), etc.

He fell down all of sudden while practicing Judo, and was ambulanced to the hospital immediately, although, could not be rescued.
Closing
His heritage is too great to evaluate.
Only what I could say is, “He was a very courageous person”.
He could do what he believed justice even if only by himself.
We can learn much by what he did, and moreover, by supposing what he would do if he were here.
May his soul rest in peace.
Acknowledgements
This manuscript is dedicated to Mrs. Tomoko Naruke, spouse of the late Professor Tsuguo Naruke, and also thanks for the permission of all figures in manuscript.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare. This content was presented in the 2nd International Conference of ATEP 2015 in Seoul National University Bundang Hospital, on 5th Dec, 2015.
References
- Naruke T, Asamura H, Kondo H, et al. Thoracoscopy for staging of lung cancer. Ann Thorac Surg 1993;56:661-3. [Crossref] [PubMed]
- Naruke T, Suemasu K, Ishikawa S. Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J Thorac Cardiovasc Surg 1978;76:832-9. [PubMed]
- Naruke T, Yoneyama T, Ogata T, et al. Bronchoplastic procedures for lung cancer. J Thorac Cardiovasc Surg 1977;73:927-35. [PubMed]
Cite this article as: Morikawa T. Heritage of the late Professor Tsuguo Naruke. J Vis Surg 2016;2:86.