A tale of surviving three consecutive cardiorespiratory arrests on table during a right sided pneumonectomy
Clinical presentation
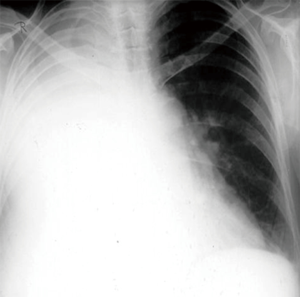
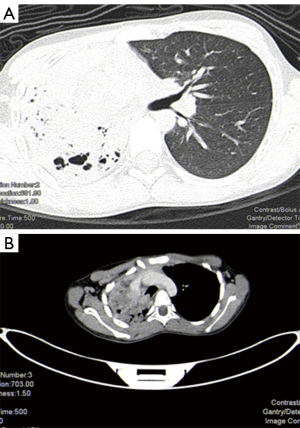
A 10-year-old male presented with history of recurrent chest infections over 2 years. He had occasional shortness of breath and asthma like symptoms. Local general practioner was treating this patient with repeated courses of antibiotics and bronchodilators. Serial chest X-ray (Figure 1) from 2 years ago to now showed evidence of progressive collapse and consolidation of right lung. CT scan of the chest shows evidence of right main bronchus tumor (Figure 2).
Bronchoscopy performed at our centre showed presence of large hard polypoidal mass in the right main bronchus extending up to the carina (Figure 3). It was not possible to navigate the bronchoscope passed the mass. It was hard rock in consistency. Multiple biopsies were taken. Histology suggested this to be a squamous papilloma. Endobronchial lasering and snaring was attempted but not well tolerated by the patient. After detailed discussion with the family, he was scheduled for a surgical resection.
Intraoperative procedure
Intraoperative plan included performing a sleeve resection if possible. Consent included the possibility of sleeve lobectomy and right pneumonectomy. Informed consent was obtained from the father of the patient as patient was a minor (<18 years). The patient was scheduled for surgery. General anesthesia was induced. A 26-French double lumen tube was passed into the left main bronchus under guidance of pediatric intubation scope. Additional monitoring was done using the radial arterial line. A left sided central line was also placed for intraoperative infusion.
The patient was placed in lateral position with right side up. Double lumen intubation was checked, endotracheal tube was fixed. The patient was found to be tolerating single lung ventilation well.
Three small ports were created and dissection was commenced by VATS, however the lung was very densely adhering to the chest wall. It was difficult to dissect the lung by VATS. Hence, right thoracotomy was performed. The right lower lobe was dissected off the diaphragm to reach the inferior pulmonary ligament. Suddenly, the patient started to desaturate. The oxygen saturation dropped progressively from 100% to 45%. The anaesthetist found that he could not ventilate the patient. The following possibilities were contemplated:
- Respiratory arrest;
- Cardiac arrest;
- Air embolism;
- Pulmonary embolism.
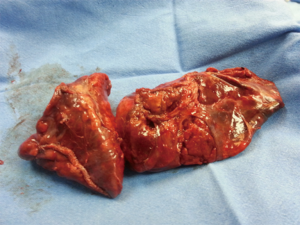
Despite repeated attempts to readjust the endotracheal tube, the anesthetist confirmed that he was unable to ventilate the patient and that the patient was apneic. The thoracotomy was draped over and the patient was urgently turned supine. The anesthetist readjusted the endotracheal tube. At this stage the patient was being re-ventilated and the saturation started to rise from 45% back to 100%. An urgent bronchoscopy could not confirm the cause of the problem. However decision was taken to continue the surgery. The patient was again turned over lateral, re-draped, lung exposed. The lung was found to be completely destroyed and not recoverable. Hence a decision was taken to perform a pneumonectomy. The lower lobe was accessed. Inferior pulmonary vein was stapled, inferior pulmonary artery was stapled using Covidien 45 Tan endostapler. As access to the hilum was still not feasible, the lower lobe bronchus was stapled, lower lobe was delivered to facilitate space for further dissection. Dissection of the hilum and upper lobe were continued. One hour into the surgery the patient again started to drop his saturation down to 45%. The anesthetist again could not ventilate the patient at all. Resuscitation was commenced. Thoracotomy was draped and patient was turned over. The endotracheal tube was re-adjusted. Urgent bronchoscopy was performed. The left lung was suctioned out. The saturation started to rise to 100% and patient stabilized. The patient was turned over lateral a third time. The chest was accessed through thoracotomy. Main pulmonary artery was exposed and stapled using Covidien 45 Tan stapler. The superior pulmonary vein was isolated and stapled. The right main bronchus was exposed using an umbilical tape. Due to the previous arrest there was no time for bronchotomy. The right main bronchus was stapled at the carina and the specimen was delivered (Figure 4). Suddenly, the patient started to desaturate again and had a cardiac arrest. The pericardium was opened. An open cardiac massage was performed. Resuscitation was continued. At this stage the stapled carina was held and the staple line was re-opened to look into the left main bronchus. That is when we realized that there was a tumor embolization into the left main bronchus. This was causing complete obstruction of the endotracheal tube on the left. Hence the patient was repeatedly becoming apneic. A Desjardin’s forceps was used to extract the tumor from the left main bronchus (Figure 5). A single lumen endotracheal tube was passed into the left main bronchus via the operative field. The patient was now ventilated, saturations climbed back to 100%.
A single lumen tube was passed through the trachea across into the left main bronchus while withdrawing the per-operative tube. The anesthetist was now able to freely ventilate left lung. The right main bronchus stump was suture with interrupted 3–0 PDS sutures. A single drain was placed in the right chest and thoracotomy was closed in layers.
Postoperative intensive care management
The patient was shifted to pediatric ICU and ventilated for 2 days. He was cooled down and ice pack was applied to the head. Intravenous Mannitol infusion was given. Forty eight hours later the patient woke up from sedation. A neurological examination confirmed good power in all four limbs. He was extubated. The ICD was removed and patient was discharged from hospital 4 days later. Follow up at 6 months confirmed that the patient was doing extremely well. He had no more chest infections. He was back to school, performing well in his activities.
Discussion
Squamous papillomas are rare benign pathologies of the tracheobronchial tree. They are usually thought to be sequelae of viral infection and can be solitary or multiple. Solitary endobronchial papillomas are the rarest kinds. Only five cases were reported in a series of 15,000 bronchoscopies by Barzó et al. (1). Surgical resection is the gold standard, but small lesions can be successfully treated endobronchial by using YAG laser or electrocautery.
In our case since the endobronchial lesion was very large and the lung distal to it was destroyed we went ahead with a surgical resection.
There are certain important lesions to take home following this case. It is important to stay cool and calm during a crisis intraoperatively. It is important to understand the root cause of the problem. It is vital that there is good communication between the anesthetist and surgeons during thoracic surgery. If there is difficulty in ventilating the patient in lateral position, it is important to turn the patient over supine to enable the anesthetist to have good access to the airway. The pericardium can be opened to facilitate intraoperative cardiac massage. Opening the bronchial stump per-operatively allows you to peep into the left main bronchus. A per-operative bronchoscopy may also give you good image. Ventilation of left lung can be done through the operative field across the bronchial stump. This manoeuvre is similar to the technique described back by Geffin et al. (2) in 1969 for anesthetic management of tracheal resection and reconstruction. Following tracheal intubation with the ETT above or sometimes through the lesion, the lungs are ventilated using IPPV. Once the trachea is transected by the surgeon, the proximal ETT is pulled back, but kept in the trachea, and a new and sterile ETT is inserted by the surgeon, through the surgical field, into the distal trachea if the tracheal lesion is high or in the left mainstem bronchus if the lesion is near the carina or at the carina itself. Sterile tubings are then attached to this distal ETT and passed to the anesthesiologist so that IPPV can be resumed.
It is important not to give up. If in trouble, it is essential to ask for help from other colleagues.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent:Written informed consent was obtained from the patient for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Barzó P, Molnár L, Minik K. Bronchial papillomas of various origins. Chest 1987;92:132-6. [Crossref] [PubMed]
- Geffin B, Bland J, Grillo HC. Anesthetic management of tracheal resection and reconstruction. Anesth Analg 1969;48:884-90. [Crossref] [PubMed]
Cite this article as: Khan AZ, Ali K, Agarwal N, Khandelwal S. A tale of surviving three consecutive cardiorespiratory arrests on table during a right sided pneumonectomy. J Vis Surg 2016;2:96.