Video-assisted thoracoscopic right upper sleeve lobectomy for fixated interlobar lymph node
Surgical resection represents the best therapeutic option Video-assisted thoracic surgery in patients with non-small cell lung cancer (1). Surgical approaches include posterolateral thoracotomy, anterolateral thoracotomy, video-assisted thoracoscopic surgery (VATS). VATS has been demonstrated to dramatically diminish pain, hasten recovery, reduce complications, and reduce postoperative complications and mortality, lead better postoperative quality of life, better preservation of pulmonary function (2-4). Sleeve lobectomy was initially accepted as an alternative to pneumonectomy for patients with low-grade, centrally located tumors and compromised cardiopulmonary reserve. Today, it has been accepted as first line intervention for centrally located lesions of all grades. We report a case of right upper sleeve lobectomy via VATS.
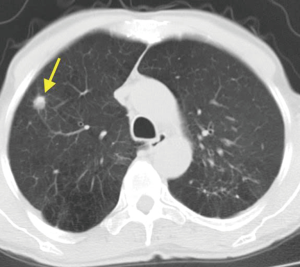
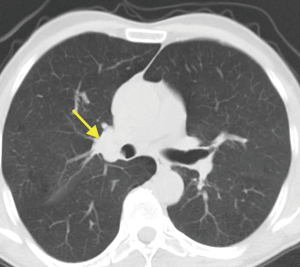
The patient was a 59-year-old male who was admitted in to our outpatient clinic due to intractable cough. He was a heavy smoker. A CT revealed a 2 cm mass located in the right upper lobe (Figure 1). Also, an interlobar lymph node adjacent to right upper lobe was seen on CT (Figure 2). A fiberoptic bronchoscopy revealed a mass obstructing right upper lobe nearly completely. An endobronchial biopsy disclosed squamous cell carcinoma. The patient’s biochemical parameters are in normal limits. Forced expiratory volume in 1 second (FEV1) was 1,910 mL (73%), forced expiratory capacity (FVC) was 3,010 mL (94%) and FEV1/FVC was 64%. Cranial MRI and a PET-CT revealed no metastasis. A mediastinoscopy was performed in order to biopsy paratracheal (#2R, #2L, #4R, #4L) and subcarinal (#7) stations. There was no N2 disease revealed by mediastinoscopy. An informed consent was obtained from the patient.
The patient received general anesthesia with double-lumen endotracheal intubation. He was positioned in the left lateral decubitus position. The 10-mm camera port was placed in the 7th intercostal space anterior axillary line. Another 10-mm port was placed posteriorly in the 6th intercostal space. Another 10 mm port was created immediately above the hilum anteriorly. This port was elongated during sleeve anastomosis and become extraction port for the specimen at the end of the operation.
Firstly, superior pulmonary vein was dissected, stapled and divided using a 45 mm endostapler. Anterior truncus branch, apical branch and a branch of posterior ascending of the right pulmonary artery were dissected, divided and stapled using endostapled after identification of interlobar artery and middle lobe arterial branches. We used a 60 mm stapler to divide major and minor fissures. Because of the fixated #11 frozen-section proven positive (for tumor) lymph node located on the right upper lobe and main bronchus junction, we decided to perform a right upper lobe sleeve resection. The main bronchus and intermediary bronchus were dissected and cut using a scalpel through the utility incision (elongated anteriorly placed port). The resected right upper lobe was then extracted with an endobag. Tumor-free margins (right main bronchus and intermediary bronchus) were confirmed by frozen-section pathological analysis. The right main bronchus was anastomosed to the right bronchus intermedius with a single running 3–0 prolene suture (Figure 3). After confirming that there was no air leak from the anastomosis, mediastinal fatty tissue was used to cover the anastomosis. A complete mediastinal lymph node dissection including lymph nodes #2R, #4R, #7, #10, #8 was then performed. There was no complication. A fiber-optic bronchoscopy performed after operation revealed no anastomotic complication. The patient was discharged after 8 days without any complication. Postoperative pathological evaluation revealed a squamous cell carcinoma of a stage T3N1M0. The patient has been doing well for 18 months. He received adjuvant chemotherapy.

Sleeve lobectomy should be performed in patients with centrally located tumors invading main or intermediary bronchus when possible. With the development of VATS, a minimally invasive method presents a better alternative approach in terms of morbidity, mortality, postoperative stay, quality of life, acute and chronic pain and cosmesis (2-4,6). The need for a sleeve resection should not preclude the minimally invasive approach. Sleeve lobectomy has been performed usually for the tumoral invasion of main bronchus or bronchus intermedius. However, a tumor-positive, bronchus invading interlobar lymph node prevents a tumor-free margin standard lobectomy since the invasion of right-upper lobe junction. For this reason, a sleeve lobectomy was necessary in our case. A complete evaluation and preoperative bronchoscopy immediately performed before operation is of utmost importance for the evaluation of the tumor and the correct operative strategy. Fixated lymph nodes are the true enemies of clear and rupture-free dissection of bronchus and arterial branches. Intranodal dissection strategies do not prevail in all patients. Sleeve and/or bronchoplastic resection may be necessary to overcome this difficulty.
We performed complete VATS approach for almost all T1a to T3 tumors. As reported previously, we believe that, VATS sleeve lobectomy should be considered in patients who need the procedure for a R0 resection (7). There is no need for specific instrument or traction sutures for VATS sleeve resection, however, a knot-pusher is a useful helper for knot-tying. A continuous 3–0 prolene has been used for anastomosis without any complication. Running sutures are proven to be safe and easier for VATS anastomoses. A postoperative bronchoscopy should be performed for the visualization of the anastomosis and secretion clearance. A supportive mediastinal tissue with a good blood support is recommended to be used to cover the anastomosis at all times.
Preoperative mediastinal staging is performed according to latest ESTS guidelines (8) at our institution. We did not perform mediastinoscopy or EBUS-TBNA if the tumor is peripheral, T1 and there was no mediastinal lymph node involvement on PET-CT. Since the tumor is located on right upper lobe, a mediastinoscopy was performed before planned surgery.
As a result, VATS sleeve lobectomy is a safe and doable operation for the patients in whom an interlobar fixated tumor-positive lymph node precluded standard lobectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- LoCicero J III. Surgical treatment of non-small cell lung cancer. In: Shields TW, LoCicero J, Reed CE, et al., editors. General Thoracic Surgery, 7th Edition. Philadelphia: Lippincott Williams & Wilkins, 2009:1387-1426.
- Li WW, Lee TW, Lam SS, et al. Quality of life following lung cancer resection: video-assisted thoracic surgery vs thoracotomy. Chest 2002;122:584-9. [Crossref] [PubMed]
- Rizk NP, Ghanie A, Hsu M, et al. A prospective trial comparing pain and quality of life measures after anatomic lung resection using thoracoscopy or thoracotomy. Ann Thorac Surg 2014;98:1160-6. [Crossref] [PubMed]
- Nomori H, Ohtsuka T, Horio H, et al. Difference in the impairment of vital capacity and 6-minute walking after a lobectomy performed by thoracoscopic surgery, an anterior limited thoracotomy, an anteroaxillary thoracotomy, and a posterolateral thoracotomy. Surg Today 2003;33:7-12. [Crossref] [PubMed]
- Turna A, Toker SA. Following dissection of right main bronchus and bronchus intermedius, tumor-free-proven tracheal rim was anastomosed to bronchus intermedius using running 3–0 prolone sutures. Asvide 2016;3:257. Available online: http://www.asvide.com/articles/1019
- Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. [Crossref] [PubMed]
- Zhang R, Xia W, Yu Z, et al. Complete video-assisted thoracic surgery right upper lobe sleeve resection. J Thorac Dis 2013;5 Suppl 3:S331-2. [PubMed]
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
Cite this article as: Turna A, Toker SA. Video-assisted thoracoscopic right upper sleeve lobectomy for fixated interlobar lymph node. J Vis Surg 2016;2:115.