Learning curve and subxiphoid lung resections most common technical issues
Introduction
The subxiphoid approach has been adopted during the last decades for thoracic and cardiovascular minor procedures such as thymectomies, pulmonary metastasectomies, pneumothorax or pericardial windows (1-3).
The first subxhipoid uniportal video-assisted thoracoscopic procedure for major lung resections was described in 2014 (4,5) and clinical evidence is lacking (6).
All data were collected prospectively from patient medical notes and computerized records. Consent forms were signed by all participating patients. This new procedure was approved by the hospital’s Institutional Review Board. The subxiphoid uniportal video-assisted thoracic surgery (SVATS) program started in September 2014; approximately 450 patients underwent SVATS major lung resection in Shanghai Pulmonary Hospital, Shanghai, China. This included two different approaches: subcostal subxiphoid incision (7) and subxiphoid midline incision. We present the learning curve of the first 200 selected patients who underwent uniportal subxiphoid lobectomy or segmentectomy by subxiphoid midline incision.
With the lessons learned from this early experience in SVATS and from the experience with transthoracic uniportal VATS we sought to compile “tips and tricks” for managing the multiple intraoperative technical difficulties that can arise during the SVATS.
Length of the learning curve
The length of the learning curve has been suggested to consist of 50 VATS lobectomies for conventional and transthoracic uniportal VATS (8), but several factors influence the length of the learning curve; previous experience in VATS minor or major procedures and learning in a high volume training center.
The learning curve of the SVATS approach could be longer and more difficult in comparison with transthoracic uniportal VATS, because the view is caudal-cranial and anterior to posterior. From the subxiphoid incision to the hilum, it is in an oblique and longer distance so the instrument fighting problem during uniportal subxiphoid surgery will be challenging. For this reasons the surgeon who performs SVATS needs previous experience in uniportal VATS lobectomy and a skilled assistant.
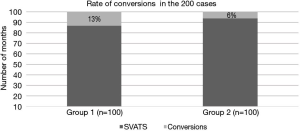
Of the 200 consecutive selected cases (72 males, 128 females) with a mean age of 57.4±9 years, underwent either uniportal subxiphoid lobectomy or segmentectomy 136 were lobectomies and 64 were segmental resections. In Figure 1, the conversion rate of the group one (first 100 cases) and group two (subsequent 100 cases) are illustrated.
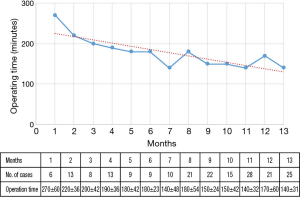
In Figure 2 the gradual reduction in the operating time with increasing experience month by month is illustrated.
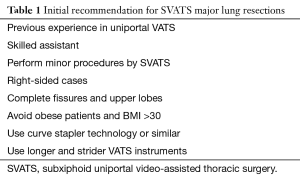
Recommendations for a SVATS lobectomy program
Before embarking in a SVATS program it is important to have previous experience in uniportal VATS lobectomy and a skilled assistant. Performing minor procedures like wedge resections and pneumothorax lung-repair is helpful as the surgeon will get familiar with the port placement, the anatomic variations and the caudal-cranial and anterior to posterior view. We recommend starting major lung resection on the right side and cases with complete fissure. The use of longer and sturdier VATS instruments makes easier to do lung grasping and sometimes curved-tip stapler technology to facilitate the passage around the structures.
Try to avoid obese patients, we consider a BMI >30 a contraindication for SVATS (Table 1).
Full table
Patient’s selection
The inclusion criteria for operating on patients by SVATS in our Thoracic Unit includes patients with benign diseases and patients with lung cancer with T status of tumour <5 cm (T1, T2) N status for tumour N0, FEV1 and DLCO >40% postoperative predicted. The exclusion criteria for operating patients with subxiphoid approach includes: chest wall involvement, central masses, previous thoracic surgery, adhesions, body mass index (BMI) >30, cardiomegaly and enlarged lymph nodes with N1 and N2 disease confirmed.
Troubleshooting guide
Patient position
The patient is put under general anesthesia with double lumen endotracheal intubation. The patient is positioned in a lateral position inclined at 60–70°. A surgeon and scrub nurse stand in front of the patient. The assistant stands at the back of the patient and the screen is placed at the head of the patient.
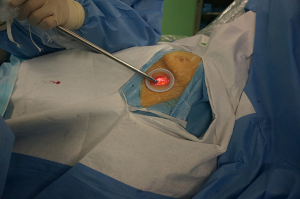
The lateral position of the patient inclined at 60–70° allows better access and view of the anterior mediastinum, thus helping the assistant with optimal camera positioning. Using a wound protector also enables effective camera and instrument insertion, without the need for a sternal lifter (Figure 3).
The operative field must be sterilized widely, to allow multiple port placements and conversion to thoracotomy in case of an emergency.
Port placement
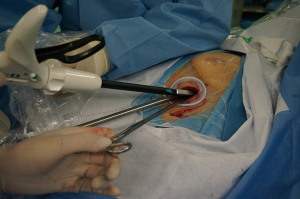
A 4 cm midline incision is made below the sterno-costal triangle, median subxiphoid incision is made if the infrasternal angle ≥70° or transverse incision is made if the infrasternal angle <70°. The rectus abdominis is divided. The xiphoid process is exposed and detached from the rectus abdominis and resected (Figure 4). The right or left pleura are opened by finger dissection via the infra-sternal angle above the level of the diaphragm and remove the pericardial fat tissue near and round the wound. One of the most common problems during dissection is the difficult passage of the staplers and longer instruments trough the incision. To avoid this is necessary to remove the surrounding pericardial adipose tissue at the beginning of the surgery (Figures 5,6).



Difficult body habitus
Obtaining Subxiphoid access can be difficult in patients with significant subcutaneous obesity or mediastinal adipose tissue. We consider a BMI >30 a contraindication to perform SVATS.
Surgeon-assistant
Is important the surgeon-assistant coordination for surgical movements to reach with the camera the desired areas. If the incision is median the camera is placed in all cases on the caudal side of the incision. If the incision is transverse, the camera is placed on the inferior side of the incision, with the assistant holding the camera at the back of the patient. The longer and strider VATS instruments are placed from the cranial side of the incision if median and the superior side if transverse (Figure 7).
Laterality
This approach is more convenient and easier to perform right-sided procedures. The subxiphoid approach from the left side chest cavity is more challenging because the cardiac pulsation is transmitted to the VATS instruments and may cause intraoperative arrhythmia in some patients due to the compression of the heart by the insertion and manipulation of the instruments. In our experience 13% of the patients had intraoperative arrhythmia that lasted till the postoperative period. In some cases a self-limited hypotension event may occur during the operation secondary to heart compression, in these cases stop the procedure for some minutes. Try to avoid patients with cardiomegaly or previous arrhythmia.
Based in our initial experience with subxiphoid uniportal approach we founded that posterior segment (S3) and superior segment (S6) in the left side and basal-posterior segment (S10) in right and left side are not feasible by this approach.
Exposure and retraction
The access for the view of the posterior mediastinum is difficult, resulting in the need for the lung requiring more traction to assess the lesions in this area. The use of longer and sturdier VATS instruments makes it easier to carry out lung grasping, and sometimes the use of curved-tip stapler technology helps to facilitate passage around the structures. One limitation of the SVATS is the impossibility to palpate the lesions. The instruments we use to perform SVATS are self-made (Figures 8,9).


Bleedings
One of the limitations of the SVATS approach is the control of major bleeding. When an emergent conversion to open surgery is necessary, an extension of the subxiphoid incision is unlikely to be useful and an additional thoracotomy must be performed. In case of a major bleeding the most important attitude is keep calm compress with sponge and a stick and decide if you can repair it adding a second trans costal port or perform an additional thoracotomy
Lymph node dissection
We recommend performing the mediastinal lymph node sampling (MLNS) or mediastinal lymph node dissection (MLND) with energy devices.
In the right-sided procedures the lymph node dissection is easier to perform. To perform right paratracheal lymph node dissection or sampling, we recommend the retraction of the superior vena cava (SVC) and pulled up the azygos using suction creating a better exposure of the area, in some cases we recommend to loop the azygos vein for better traction and exposure
In left sided procedures station four, five and six are not very challenging to expose and dissect. The subcarinal lymph node dissection in the left and right side is challenging and traction manoeuvres are needed it to reach this area. In some cases it is possible to perform nodal sampling only. With increasing experience and the development of new instruments the dissection of the subcarinal lymph nodes will be routinely dissected like in conventional VATS.
Comments
The Table 1 shows a set of recommendations for a surgeon embarking on SVATS program for major lung resections. The learning curve of the SVATS is longer and more difficult in comparison with transthoracic uniportal VATS. To our knowledge, there have been only case reports and a few recent of series of cases of the use of SVATS for major lung resections, describing benefits similar to those of transthoracic uniportal VATS in terms of duration of chest drain use, length of hospital stay, operating time, rate of conversion and complications (13-15).
There is a gradual reduction in the operating time with increasing experience. After the case number 85 the operating times becomes similar in almost all the procedures. In Figure 1 the rate of conversion is illustrated showing improvement with increasing experience in group number two.
SVATS for major lung resections is an alternative approach with a new learning curve to pass same as occur when a surgeon decide to evolve from conventional VATS to Uniportal VATS (16-18). The different view cauda-cranial and anterior to posterior, the dissection of the hilar structures and lymph node dissection makes more challenging this approach.
Although conversion to multiport VATS or thoracotomy should be always performed if required for ensuring safety or complete resection. We recommend having a clear preoperative plan and case selection. Further studies are necessary to certificate the applicability and clinical outcomes of the SVATS in order to show clear benefits from this technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Shanghai Pulmonary Hospital Institutional Review Board and written informed consent was obtained from all patients.
References
- Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. [Crossref] [PubMed]
- Liberman M, Labos C, Sampalis JS, et al. Ten-year surgical experience with nontraumatic pericardial effusions: a comparison between the subxyphoid and transthoracic approaches to pericardial window. Arch Surg 2005;140:191-5. [Crossref] [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
- Ismail NA, Elsaegh M, Dunning J. Novel Techniques in Video-assisted Thoracic Surgery (VATS) Lobectomy. Surg Technol Int 2015;26:206-9. [PubMed]
- Hernandez-Arenas LA, Lin L, Wu L, Aresu G, Jiang G, Jiang L. Subxiphoid uniportal video-assisted thoracoscopic trisegmentectomy. J Vis Surg 2016;2:90. [Crossref]
- Song N, Zhao DP, Jiang L, et al. Subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy: a report of 105 cases. J Thorac Dis 2016;8:S251-7. [PubMed]
- Yan TD, Cao C, D'Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2014;45:633-9. [Crossref] [PubMed]
- Hernandez-Arenas LA, Guido W, Jiang L. Pleura opened by finger dissection via the infra-sternal angle. The xiphoid process is exposed and detached from the rectus abdominis and resected. Asvide 2016;3:273. Available online: http://www.asvide.com/articles/1035
- Hernandez-Arenas LA, Guido W, Jiang L. Wound protector enables effective camera and instrument insertion. Asvide 2016;3:274. Available online: http://www.asvide.com/articles/1036
- Hernandez-Arenas LA, Guido W, Jiang L. Removal of the surrounding pericardial adipose tissue at the beginning of the surgery. Asvide 2016;3:275. Available online: http://www.asvide.com/articles/1037
- Hernandez-Arenas LA, Guido W, Jiang L. Dissection of left anterior segmental bronchus, with longer and strider instruments and use of curve stapler technology. Asvide 2016;3:276. Available online: http://www.asvide.com/articles/1038
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Uniportal video-assisted thoracoscopic surgery: experience with 471 cases. Interact Cardiovasc Thorac Surg 2013;17:S1-S62. [Crossref] [PubMed]
- Gonzalez-Rivas D. Evolving thoracic surgery: from open surgery to single port thoracoscopic surgery and future robotic. Chin J Cancer Res 2013;25:4-6. [PubMed]
- Ng CS. Single-port thoracic surgery: a new direction. Korean J Thorac Cardiovasc Surg 2014;47:327-32. [Crossref] [PubMed]
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5 Suppl 3:S221-5. [PubMed]
Cite this article as: Hernandez-Arenas LA, Guido W, Jiang L. Learning curve and subxiphoid lung resections most common technical issues. J Vis Surg 2016;2:117.