How to identify the posterior boundary of No. 8a and the right side group of No. 9 lymph nodes?
Introduction
Suprapancreatic lymphadenectomy is important for gastric cancer surgery. A number of laparoscopy-assisted gastrectomy procedures have been performed in the same manner as open surgery (1-3), which makes the suprapancreatic lymphadenectomy possible and feasible. In recent years, several surgeons have developed kinds of methods for suprapancreatic lymphadenectomy. Satoh et al. (2) and his colleagues firstly introduced the method that dissecting from right to left. And Fukunaga et al. (4) developed a left-sided approach without duodenal transection. Then in 2011, Kanaya et al. (5) introduced a medial approach for suprapancreatic lymph node (LN) dissection. Last year, Huang et al. (6) and his colleagues successfully introduced another left-side approach for suprapancreatic LN dissection. All these techniques make the procedure more operable and simple. But there’s few detail description about the precise extent of the LNs, especially the posterior boundary of No. 8a and the right side group of No. 9 LNs. That still confuses many gastric surgeons. Here we discuss about this issue and focus on the posterior boundary of No. 8a and the right side group of No. 9 LNs.
Patient selection and workup
Patients for this operation should be diagnosed as distal gastric cancer, which have a pre-operative stage of cT2-4aNxM0 or cT1N+M0, with gastroscopic biopsy and contrast computed tomography (CT).
Inclusion criteria: (I) distal gastric adenocarcinoma with biopsy; (II) pre-operative stage of cT2-4aNxM0 or cT1N+M0 with contrast CT; (III) age from 20 to 70 years old.
Exclusion criteria: (I) T1N0 orT4b tumor; (II) distal metastasis detected before or during operation; (III) apparent LNs fusion; (IV) history of previous gastrectomy; (V) pre-operative neoadjuvant chemo- or radiotherapy; (VI) age beyond 70 years old; (VII) with severe systemic problems that can’t endure major operations.
Pre-operative preparation
- Careful pre-operative examinations to exclude any contraindication;
- Proactive preparation of respiratory system for 3 days;
- Proactive mental preparation of the patients before operation;
- Inserting gastric tube and urethral catheter right before operation;
- Preparation of all instruments needed for the operation.
Equipment preference card
- Laparoscopy system, including a high-definition camera, display system, and pneumoperitoneum machine;
- Irrigation and suction devices;
- Image and video storage devices;
- Ultracision;
- Biactive coagulation set;
- Intestinal endo-GIA;
- Circular staplers;
- 5–12 mm trocars;
- Intestinal forceps;
- Maryland forceps;
- Noninvasive grasping forceps;
- Scissors;
- Needle holder;
- Absorbable suture;
- Aspirator;
- Absorbable clip applier;
- Titanium clip applier;
- Vascular clamps;
- Small gauzes.
Procedure
Patient’s position
Patient position is very important for intraoperative exposure during laparoscopic gastrectomy. A reverse Trendelenburg position with the head elevated approximately 15 degrees is used.
Trocar locations
As the trocars’ position, here we make a little change. In routine procedure, the 5-port method is generally used (7). We lower the observation port to 2–3 cm below the umbilicus.
Surgeons’ locations
The surgeon stands on the patient’s left side, with the assistant on the right and the camera operator between the patient’s legs.
Procedure
Firstly, the assistant’s left-hand grasper forceps grasped the pedicle of left gastric vessels at the point close to the lesser gastric curvature and lifted up the stomach vertically, his or her right-hand grasper forceps lifted up the lymph-adipose tissue in front of common hepatic artery (CHA). The surgeon’s left-hand grasper forceps pressed the body of pancreas down and caudal ward and began the dissection of NO. 8a LNs in front of CHA with ultrasonic scalpel, to the right until the exposure of gastro-duodenal artery, to the left until the exposure of the initial segment of splenic artery (SpA). Then the assistant’s right-hand grasper forceps lifted up the lymph-adipose tissue around SpA. The surgeon continued to dissect the No. 11p LNs and the left side group of No. 9 LNs. Because the celiac artery (CA) was tilted to left, the left paries of CA would be exposed after dissection of the left side group of No. 9 LNs. The surgeon continued the dissection along the left paries of CA until exposure of the superior margin of the root of CA (point B, which was described below). The assistant lifted up the lymph-adipose tissue around the root of left gastric vessels and the surgeon denuded the vessels and divided left gastric vein first then the artery to finish the No. 7 LNs dissection. Secondly we transected the duodenum (or not). The assistant put down the stomach; the surgeon began the dissection of No. 5 LNs, denuded the right gastric vessels and divided them at the root. The assistant’s left-hand pulled the divided right gastric vessels to the left direction, the surgeon’s left-hand pulled proper hepatic artery to the right and began the dissection of No. 12a LNs along the PHA until the left paries of portal vein (PV) had been exposed. The assistant’s right-hand grasped the right segment of CHA to right and lower direction with left-hand lifted up the lymph-adipose tissue of No. 8a LNs to left and upper direction. The surgeon dissected No. 8a LNs along CHA from the right to left side until the superior margin of PV had been exposed. At last we arrived at the crossover of the superior margin of PV with CHA (point A, which was described below). Thirdly, we made an imaginary horizontal plane including point A and B as the posterior boundary of No. 9 LNs. The surgeon’s left grasper forceps pulled down the CHA and continued the dissection of No. 8a and the right side group of No. 9 LNs until the lymph-adipose tissue in front of the imaginary plane has been removed completely. Finally the lymphadenectomy of supra-pancreatic area was completed.
Role of team members
Surgeon: perform the major part of the operation.
Assistant: help to expose the visual fields of the operation and assist the surgeon to perform the operation successfully.
Camera operator: in charge of the camera system to gain a sharp and comfortable view of the operation.
Anesthetist: in charge of the patient’s anesthesia to make sure the patient is in well anesthetic state during the operation.
Nurses: in charge of the devices needed for the operation before and during operation.
Post-operative management
- Parenteral nutrition for 5–7 days after operation;
- Out-of-bed activity on day 2;
- Extract gastric tube after passage of gas by anus;
- Liquid diet the next day after extraction of gastric tube;
- Semi-liquid diet on day 7 and extract peritoneal cavity drainage tubes;
- Discharge on day 8.
Tips, tricks and pitfalls
Here we discuss about the suprapancreatic lymphadenectomy, focusing on No. 8a and the right side group of No. 9 LNs. Many gastric surgeons still get confused about the posterior boundary of No. 8a and the right side group of No. 9 LNs. It will cause insufficient lymphadenectomy if the dissection is too superficial and unnecessary injury will occur if it’s too profundus.
We think the principle thing is to identify the dissection extents of No. 8a and 9 LNs and to find out the corresponding anatomical landmarks. Our experience is that the superior margin of PV can be used as a good anatomical landmark for No. 8a and the right side group of No. 9 lymphadenectomy. And to make it simple and sensible, we also use two points (A and B) and an imaginary plane as accessory landmarks, which will be described below.
Using the superior margin of PV as anatomical landmark, two requirements should be fulfilled, reasonable in theory and feasible in technique.
Firstly, is it reasonable in theory? We retrieve the documents about the grouping of LNs for gastric carcinoma of Japanese classification of gastric carcinoma. The concept for No. 8a LNs is those along the CHA (anterosuperior group). And No. 8p LNs is those along the CHA (posterior group). From the illustration figure, we can see there are no LNs between CHA and PV, which is coincident with what we see during operation. No. 8p LNs is those in the profundus location behind the superior margin of PV, we can regard the superior margin of PV as the dividing line of No. 8a and 8p LNs. In other words, the superior margin of PV can be used as the anatomical landmark for the posterior boundary of No. 8a LNs.
Where is the posterior boundary of the right side group of No. 9 LNs? There’s no detail description about that. According to the Japanese classification of gastric carcinoma, No. 9 LNs is defined as those LNs along the CA, so we can regard the root of CA as the posterior boundary of No. 9 LNs. But actually it does be hard to expose the root of the CA, especial the right paries of the root of CA during laparoscopic surgery. Here we try to make it simple and sensible. Firstly we mark two points, A and B. We name point A as the point where the superior margin of PV meets the CHA (Figure 1) and point B as the superior margin of the root of CA (Figure 2). It’s easy to expose these two points as shown in the video (Figure 3). Then we draw a line from point A to B (Figure 4). And we make an imaginary horizontal plane with this line as the posterior boundary of the ride group of No. 9 LNs.
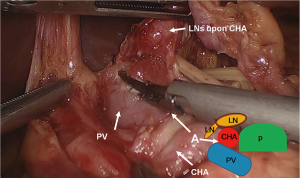
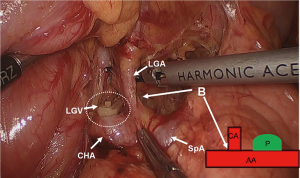
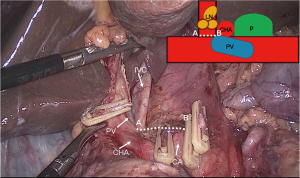
Secondly, is it technically feasible to expose the anterosuperior paries of PV in laparoscopic gastrectomy? We know that the observing direction in laparoscopic gastrectomy is different from that of open surgery. During traditional open surgery, the observing direction is from anterior to posterior, and it’s easier to expose the PV. But during laparoscopic surgery, the observing direction is from anterior-inferior to posterior-superior, and the PV is covered by the pancreas and the CHA, that brings disadvantages for exposure of PV. The following is our procedure for that (Figure 3). Firstly, we preliminarily dissect No. 8a LNs in front of CHA and expose the anterior paries of the CHA at the superior margin of the pancreas. We dissect NO. 11p LNs, the left side group of the No. 9 LNs, as we know CA is tilted to left side, the left paries of CA is easy to exposed, then we can expose the superior margin of the root of CA, which we mark it as point B. We divide left gastric vessels at the root. We transect (or not) the duodenum and dissect No. 5 LNs and divide right gastric vessels at the root. At this time, the lymph-adipose tissue of No. 12a, 8a and 9 LNs will be more isolated. Then the assistant’s left clamp pulls the lymph-adipose tissues of No. 12a, 8a LNs to the left and upper direction, and the surgeon’s left clamp pulls CHA to the right and lower direction, the surgeon begins the dissection of No. 12a and expose the left paries of PV and continue the dissection from hepatoduodenal ligament to the superior margin of CHA. Due to the natural adhesion of No. 8a lymph-adipose tissue to anterosuperior margin of PV, keeping tension during dissection, we dissect No. 8a LNs along CHA, the superior margin of PV will exposed naturally. We continue dissecting until we arrive at point A where the superior margin of PV counters CHA; we draw a line from point A to point B and make an imaginary horizontal plane with the line as the posterior boundary of right side group of No. 9 LNs. Through this method No. 8a and the right side group of No. 9 LNs can be removed completely. According to our experience, keep suitable tissue tension during dissection is very important. Insufficient tissue tension will cause difficulty for exposure of PV, but redundant tissue tension will cause abruption of the tissues.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Noshiro H, Nagai E, Shimizu S, et al. Laparoscopically assisted distal gastrectomy with standard radical lymph node dissection for gastric cancer. Surg Endosc 2005;19:1592-6. [Crossref] [PubMed]
- Satoh S, Okabe H, Kondo K, et al. Video. A novel laparoscopic approach for safe and simplified suprapancreatic lymph node dissection of gastric cancer. Surg Endosc 2009;23:436-7. [Crossref] [PubMed]
- Katai H, Sasako M, Fukuda H, et al. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703). Gastric Cancer 2010;13:238-44. [Crossref] [PubMed]
- Fukunaga T, Hiki N, Tokunaga M, et al. Left-sided approach for suprapancreatic lymph node dissection in laparoscopy-assisted distal gastrectomy without duodenal transection. Gastric Cancer 2009;12:106-12. [Crossref] [PubMed]
- Kanaya S, Haruta S, Kawamura Y, et al. Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Endosc 2011;25:3928-9. [Crossref] [PubMed]
- Huang CM, Chen QY, Lin JX, et al. Laparoscopic Suprapancreatic Lymph Node Dissection for Advanced Gastric Cancer Using a Left-Sided Approach. Ann Surg Oncol 2015;22:2351. [Crossref] [PubMed]
- Huang CM, Zheng CH. Preoperative Notes of Laparoscopic Lymph Node Dissection for Gastric Cancer. In: Huang CM, Zheng CH. editors. Laparoscopic Gastrectomy for Gastric Cancer. Berlin: Springer Netherlands, 2015:13-24.
- You J, Hong QQ, Luo Q, et al. Demonstration of the dissection of No. 8a and the right side group of No. 9 LNs with a 3D animation and laparoscopic operation. Asvide 2016;3:344. Available online: http://www.asvide.com/articles/1113
Cite this article as: You J, Hong QQ, Huang ZJ, Li YW, Lou LT, Luo Q. How to identify the posterior boundary of No. 8a and the right side group of No. 9 lymph nodes? J Vis Surg 2016;2:143.


