
Intrapericardial release method of pulmonary arterial bifurcation: surgical technique to secure left pulmonary artery
Introduction
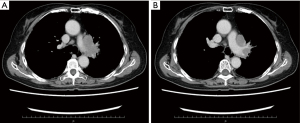
The pulmonary artery (PA) is one of the most vulnerable arteries in the body because of its thin vascular wall resulting from low blood pressure and high blood flow. Management of PA during surgery is important for thoracic surgeons because PA injury can lead to life-threatening hemorrhage. However, we sometimes experience centrally located lung cancers invading the main PA, making it difficult to access, even though the intrapericardial approach under median sternotomy (Figure 1). Transection of the arterial ligament and/or ligament of Marshall is a common technique to secure the left PA. However, if the tumor is invading close to the arterial ligament, this method may not be possible.
Herein, we report an intrapericardial release technique for PA bifurcation that enables safe access to the left main PA in such a challenging case.
Surgical techniques (Video 1)
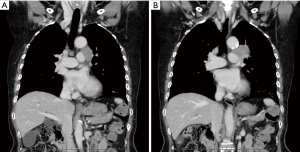
One-lung ventilation with a right-sided double-lumen endobronchial tube is recommended. Median sternotomy and left anterior thoracotomy at the second intercostal space if needed (in case when the inferior pulmonary vein can’t be exposed) were performed under the supine position. After dissecting the pre-vascular lymph nodes, we vertically cut the pericardium and exposed the ascending aorta. We taped the aorta and common PA truncus by tunneling through the transverse pericardial sinus. After vessel taping of the common PA truncus and right main PA, the PA bifurcation was dissected from the posterior pericardium by lifting the ascending aorta to the left. During traction of the ascending aorta to the right, the arterial ligament is exposed, from its proximal portion to its distal portion, and divided. To elongate the left main PA, it is necessary to disconnect the left main PA from the left atrium (ligament of Marshall) and divide the left superior pulmonary vein, then disconnect the trachea-pericardial ligament between the left main PA and main bronchus and divide the upper bronchus. We simultaneously dissected the subcarinal and paratracheal lymph nodes. Eventually, the PA bifurcation is completely free from the mediastinal structure, and the left main PA can be released and safely secured at the proximal portion, a few centimeters from the arterial ligament (Figure 2A). The left main PA was spared with arterioplasty (Figure 2B), and left upper lobectomy was successful.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s daughter for publication of this manuscript and any accompanying images and videos. A copy of the written consent is available for review by the editorial office of this journal.
Comments
Lateral thoracotomy is considered a standard approach for pulmonary resection when thoracoscopic surgery is not indicated. However, the hilar exposure is challenging under lateral thoracotomy in patients with large hilar tumors or dense hilar adhesions. Additionally, forcible traction of the lung parenchyma can easily tear the PA, resulting in life-threatening bleeding. The intrapericardial approach via median sternotomy can be an option that improves outcomes and enables easier and safer dissection of the left main PA after divisions of both the arterial ligament and ligament of Marshall. Some previous reports have indicated the advantages of the intrapericardial approach via median sternotomy in patients with hilar lung cancer invading the main PA (1,2).
Even for experienced surgeons the left main PA is difficult to secure safely in cases of hilar invasion to the proximal portion of the left main PA. The new surgical technique described in this report allows the PA bifurcation to mobilize freely from the mediastinal structure and enables safe partial clamping of the common PA truncus. With this procedure, we were able to secure a portion of the left main PA a few centimeters proximal to the arterial ligament and could spare the left main PA, leading to successful left upper lobectomy. This might be a good option not only for the case with the centrally located tumor invading the arterial ligament, but for the case receiving left completion pneumonectomy after left upper lobectomy combined with division of the arterial ligament (3).
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Peer Review File: Available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-29/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.org/article/view/10.21037/jovs-22-29/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s daughter for publication of this manuscript and any accompanying images and videos. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Igai H, Yokomise H. Intrapericardial approach via median sternotomy for hilar non-small cell lung cancer invading the main pulmonary artery. Interact Cardiovasc Thorac Surg 2010;11:385-6. [Crossref] [PubMed]
- Sanli M, Işik AF, Tunçözgür B, et al. Resection via median sternotomy in patients with lung cancer invading the main pulmonary artery. Acta Chir Belg 2009;109:484-8. [Crossref] [PubMed]
- Hattori A, Matsunaga T, Watanabe Y, et al. Repeated anatomical pulmonary resection for metachronous ipsilateral second non-small cell lung cancer. J Thorac Cardiovasc Surg 2021;162:1389-98.e2. [Crossref] [PubMed]
Cite this article as: Ozeki M, Negishi H, Endo S, Komori K, Tsubochi H. Intrapericardial release method of pulmonary arterial bifurcation: surgical technique to secure left pulmonary artery. J Vis Surg 2023;9:34.


