Robotic-assisted first and supernumerary rib resection: case series
Highlight box
Key findings
• The robotic technique for cervical rib resection shows good safety and efficacy concerning both neurologic and vascular disorders.
What is known and what is new?
• Transthoracic robotic-assisted resection of the first rib for thoracic outlet syndrome has been adopted by many surgeons in thoracic surgery with good results.
• The approach has now been extended also to supernumerary rib resections.
What is the implication, and what should change now?
• Since robotic surgery is spreading fast throughout the world these days in thoracic surgery, the indication for rib resections at the thoracic outlet has to be taken in account for every well-trained robotic surgeon.
Introduction
When dealing with thoracic outlet syndrome (TOS), very few patients present with a cervical or supernumerary (extra) rib. It is a congenital abnormality occurring in about 0.2–1% of the population (1,2). Despite the fact that most cervical ribs are asymptomatic, patients may suffer from the same symptoms that we usually see in TOS—like venous, arterial or neurogenic features. In some rare cases even life-threatening conditions were described (1).
Cervical ribs usually originate from the seventh cervical vertebrae and can vary in length between <1 cm to those that fuse to the first rib (2). Originally, cervical ribs were first described by Gruber in 1869 (3). He described four subtypes with especially the longer two types possibly leading to vascular compromise, including arterial compression and aneurysm formation as well as venous thrombosis (Table 1). In our series, all patients showed either type 3 or 4 with or without vascular involvement.
Table 1
| Cervical rib type | Rib configuration |
|---|---|
| Type 1 | Extension to the transverse process of C7 |
| Type 2 | Extension beyond the transverse process but no connection to the first thoracic rib |
| Type 3 | Cervical rib with partial fusion to the first rib by fibrous bands or cartilage |
| Type 4 | Fusion by a bony pseudoarticulation with first rib |
Other authors found 17.4% of supernumerary ribs to cause vascular symptoms and 3.8% to show aneurysms distal to the point of compression by the cervical rib and its attachments or subclavian artery thrombosis and embolization that occurs due to the repetitive pulsatile trauma caused by a cervical rib (4,5).
When it comes to the technique of first rib resections, there are a multitude of different approaches, namely supra-/infra-clavicular, transaxillary, and transthoracic. Every technique has its pros and cons. However, there is no high-quality evidence indicating any difference in success rate among the various surgical approaches. The crucial step when treating patients with TOS is optimal visualization of the neurovascular and musculoskeletal structures at the level of the thoracic outlet as well as the ability to perform complete venolysis, arteriolysis as well as neurolysis, if needed. Thus, improved visualization naturally promotes patient safety and complete surgical decompression (6,7).
Since we prefer a completely thoracoscopic 3-port robotic approach for first rib resection in TOS, the implementation and extension to the cervical rib seemed consistent. Hereby we report a case series of 6 consecutive first and cervical rib resections. We present this case series in accordance with the PROCESS reporting checklist (available at https://jovs.amegroups.org/article/view/10.21037/jovs-23-17/rc).
Case presentation
Patients
Between January 2015 and September 2022, we performed 67 robotic first rib resections. Therefrom six patients presented with a cervical rib including all different entities of TOS (neurologic, venous and arterial) and equal symptoms to the usual TOS. Four of them were male and two were female.
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from all patients prior to inclusion in the study and the study was approved by our institutional review board (No. TS2022.09). A copy of the written consent is available for review by the editorial office of this journal.
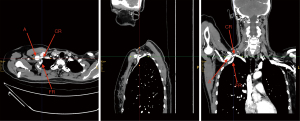
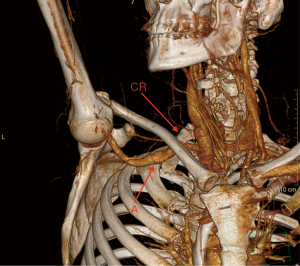
In four patients, TOS could be treated by first and cervical rib resection alone, whereas two patients required a venous or Dacron graft replacement for a subclavian/axillary aneurysm in the same procedure. The female arterial TOS patient had been referred by her family physician with recurrent episodes of pain in the forearm. Contrast enhanced computed tomography scan showed presence of a large aneurysm of the subclavian artery (Figure 1). The long cervical rib presented with a complete extension to the first rib and bony pseudoarticulation (Gruber type 4). Neurologic evaluation showed no signs of peripheral pathology in the upper limb but an acute compression of the brachial plexus by the aneurysm. The duplex sonography showed different thrombotic material in the lumen, partly floating. It was supposed that also a long-lasting Raynaud-like syndrome in the fingers reported by the patient was due to repeated embolic events. Ulnar and radial artery were partly or completely closed, so that an urgent surgical embolectomy has been immediately performed. The male arterial TOS patient was already well known at our vascular surgery department for recurrent thromboembolic events in his forearm, but he refused operative treatment for more than one year. At his last admission to our Vascular Surgery Department, he was first operated twice at the brachial artery for a surgical catheter thrombectomy and venous patch reconstruction, as he presented with acute and critical ischemia of his forearm. For this case we performed a three-dimensional (3D)-reconstruction out of the contrast enhanced computed tomography scan (Figure 2). It showed a long cervical rib with partial fusion to the first rib by fibrous bands or cartilage (Gruber type 3).
In venous TOS (vTOS) with acute thrombosis we usually treated patients first with Angio-Jet® thrombectomy before the surgical treatment. If possible, the operative procedure is scheduled 2–4 weeks after the intervention and the patient is put on oral anticoagulants or low-molecular-weight heparins.
Surgical technique
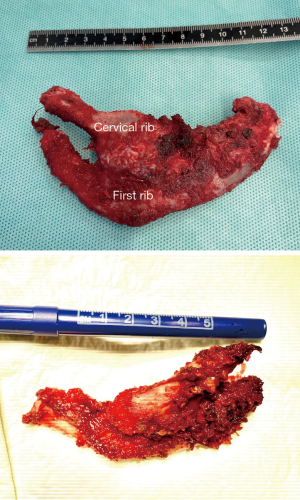
Our robotic trans-thoracic approach using the DaVinci Xi platform (Intuitive Surgical, Sunnyvale, CA) has been previously described (8,9). For the camera we use an 8-mm trocar in the fifth intercostal space midaxillary line and two 8-mm ports in the third intercostal space anterior axillary line and behind the tip of the scapula. Insufflation of carbon dioxide gas facilitates exposure. The first rib is dissected with a bipolar Maryland forceps on the right and a Cadière grasping forceps on the left. After dissection of intercostal muscles, the first rib is cut medially with a long Kerrison rongeur through the posterior 8-mm trocar. In absence of a cervical rib, this creates a trap-door mechanism so that the rib can be retracted and mobilized downward into the thoracic cavity for optimal visualization and access to all muscles and ligaments inserting there. If the supernumerary rib shows a strong partial or complete fusion with the first rib according to the Gruber subtypes 3 and 4 the bony structures cannot be moved in the same way as we found in all cases. In very slim patients it is possible to dissect the cervical rib directly up close to the transverse process of the seventh vertebra where it is cut also by the Kerrison rongeur. In larger patients the junction between the two ribs has to be cut in advance and both ribs will be dissected separately. The excellent overview allows additional venolysis and neurolysis where applicable.
We cut the posterior part of the rib also with the Kerrison rongeur (inserted through either the medial or posterior robotic trocar, whichever provides better access) lateral to the T1 nerve root only by a few millimeters. At the end, a 20-F chest tube is placed and the lung is reinflated.
For vascular replacement, an open infraclavicular approach was chosen, but thanks to prior rib resection it could be held in a minimalistic fashion through which a resection of the ribs could not have been performed. Accordingly, in one case of neurogenic affection we used an additional small supraclavicular incision for thorough neurolysis of brachial plexus.
Results
In all six patients, a complete resection of the first and cervical rib together was achieved without any intraoperative complications. Surgical time ranged between 75–365 min with a median of 170.5 min (IQR, 90–232 min). This includes also the part of vascular graft replacement in appropriate cases. One minor postoperative complication (subcutaneous hematoma in paraclavicular region) occurred in the female patient with resection of the subclavian aneurysm and neurolysis. We found no brachial plexus palsies (n=0), no phrenic nerve injury (n=0) and no chyle leak (n=0) as reported in other studies (10,11). Median hospital stay was 3 days (IQR, 3–6 days)
In pain management, visual analogue scale showed a median of 3.5 (IQR, 1–4.5) at the first postoperative day while treatment consisted of the following drugs: paracetamol, metamizole and non-steroidal anti-inflammatory drugs.
In vTOS with recent thrombosis, we start treating with oral or subcutaneous anticoagulants on the first postoperative day and continue routinely for 3 months postoperatively, depending on whether impaired venous return or residual thrombus is detected on postoperative venous duplex scan (12,13).
For arterial TOS and graft replacement acetylsalicylic acid was prescribed for at least 6 months postoperatively and for the patient with Dacron graft replacement additional oral anticoagulants have been administered for 3 months due to small vessel embolic occlusions in the preoperative phase.
We usually schedule routine follow-up visitations 3 months, 6 months, and 1 and 2 years postoperatively. All patients presented with a complete (n=4) or partial relief (n=1) where some symptoms reported by the patient already suffering from carpal tunnel syndrome on both hands and a long medical history including surgery. In everyday life, all patients attested a nevertheless substantial improvement of their medical condition. For vascular TOS patients, angiologists regularly controlled the vessels using duplex sonography for vascular patency after 3, 12 and 24 months.
Discussion
We report on our first 6 consecutive combined first and cervical rib resections as case series in two tertiary centers of thoracic surgery. Since we have developed and standardized the 3-port robotic approach for first rib resection in our country, it was a chain of reasoning that also operative treatment for cervical rib resection could be implemented as also described by Wybaillie et al. [2018] and Palivela et al. [2021] (6,11). The presence of a supernumerary rib that results in TOS is a very rare condition and subsequently only limited evidence can be found in the international literature on this topic (2,14-18). This bony anomaly accounts for about 20% of these patients which is an estimated 40 times higher prevalence than that in the general population with a 76% female rate (19). In some of them, the cervical rib is fused to the second rib lacking a real first rib. It is important to identify these really rare cases are because the anatomy is such that the second rib cannot be accessed easily, or resected via a standard approach (20,21). Such situation is ideal for a transthoracic robotic approach where you benefit most from a great overview with untroubled accessibility to all areas of dissection.
TOS will be encountered most commonly because of extrinsic neurovascular compression from a first rib or other bony abnormality or bands. It will be combined with surrounding hypertrophic muscles, which are the scalene and subclavius. Depending on which structures are compressed, patients present with symptoms of the upper extremity that can range from pain and paresthesia edema to a pale and pulseless arm (20).
Usually, the rate of neurogenic/mixed, venous and arterial TOS are 90–95%, 3–5%, 1% respectively. In the presence of bony anomalies, the compression of arterial structures rises up to 33% as we could observe in our series. Compression of arterial structures mostly results in forming of an aneurysm. Due to the compromised flow in the vessel, we found embolic complications in two patients preoperatively that required multiple interventions in peripheral arteries in one patient with transcatheter procedures as well as open surgeries. Though, vascular compromise of the very distal upper extremity should always lead to a thorough investigation of the thoracic outlet since the correct treatment can prevent patients from further episodes and chronic functional alterations (5). This might have a higher impact since most of these patients work manually and suffer from inability to work (14).
Where a supernumerary rib is associated with TOS, it should be surgically resected. There are no reports about successful conservative treatment for symptomatic supernumerary ribs. Cervical rib resection was first described by Coote in 1861 (22). For surgical decompression for TOS several reports exist about short- and long-term results. Hereby first rib resection combined with cervical rib resection when present is the recommended treatment of TOS. Even if the combination is controversial, most studies report results of combined first and supernumerary rib resection. Cervical rib resection without the first rib for TOS is rarely studied in the literature.
Nevertheless, the presence of a cervical rib is responsible for specific vascular complications like subclavian aneurysms that require appropriate treatment (23-26). As the main issue with aneurysms in this area is embolic disease with subsequent ischemic complication to the distal part of the limb treatment consists of surgical replacement of the aneurysmatic part of the vessel. Our two arterial TOS cases show good proof of these considerations. Both show good patency of the reconstructions at their 6- and 36-month follow-up. And even the case of an 8-year-old boy with a cervical rib is described in the literature suffering from a subclavian aneurysm (18).
True neurogenic TOS is rare, having a prevalence of around 1 in 1 million patients, but the presence of a supernumerary rib causes a neurogenic TOS in more than 50% of cases with a usually very delayed diagnosis (16). The delay is mainly due to the fact that the largest challenge remains the diagnosis of neurogenic TOS, because standardized diagnostic criteria are lacking. Of course, we find physical tests, electroneurography and radiological imaging as well as the aforementioned criteria for surgery but hardly any consensus on the applicability or threshold value of these examinations can be found in literature. Therefore, future studies should also focus on the diagnostic work-up of TOS (15,23,27).
For vTOS it is widely accepted that these patients will be treated in a quite standardized manner where interventional thrombolysis is thought to be the first step in a multidisciplinary treatment, followed by surgery including first and cervical rib resection when present. If still some narrowing or stenosis of the subclavian vein persists a venous stent placement is recommended. This approach has already been extensively discussed before in our work (12,13,28). After a short course of oral anticoagulants for 3–6 months the patients will remain free of medications or workout restrictions (28).
Surgical approach
Most of the discussion concerning surgical procedures is held about the best technical approach. Since several studies in the last 10 years showed a widespread adoption of robotic surgery for first rib resection, we implemented our large experience in this field for the extension to cervical rib resection (6,8,9,29-33). As a standard we use the completely thoracoscopic 3-port robotic approach with anterior and posterior transection of the rib by means of a Kerrison rongeur.
Advantages of the robotic approach are especially the good visibility of delicate structures and improved surgical morbidity that has been proven in a study by Burt et al. [2021] with less postoperative brachial plexus palsies (1% vs. 18%), phrenic nerve injury (1% vs. 6%), and chyle leak (0% vs. 4%). The latter complication occurs very rarely after cervical rib resection with a cervical approach and is reported even bilaterally by Ferris et al. [2022] (32,34). Interestingly, it resolved spontaneously by chest drains alone with no sequelae in that case. Some other authors report also Horner’s syndrome or subclavian dissection in the list of postoperative complications (9% and 3%, respectively) (14).
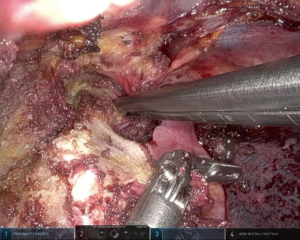
Even if the work through the posterior part of the ribs with the Kerrison rongeur in a piece-meal technique is somewhat laborious due to the narrow space, we prefer it to a drilling device since surrounding structures are protected by the smooth surface at the back of the instrument (Figure 3). Even with a very large area of fusion with the cervical rib it is feasible to remove the specimen in toto thanks to the additional degrees of freedom of the robotic instruments (Figure 4).
Though, robotic surgery has the potential to become a standard treatment for all kinds of TOS including supernumerary ribs if an appropriate system is available. The patients benefit from a minimally invasive approach with very precise dissection, resulting in extremely low morbidity.
Conclusions
In times of increasing application of robotic surgery, in all types of surgeries also procedures at the thoracic outlet show very promising results of this most minimally invasive approach so far. In cervical rib resection, the main concern is on the brachial plexus beside other well-known neurovascular structures and the presented technique offers good safety and efficacy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Robotic Thoracic Surgery: Established Procedures & Current Trends”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PROCESS reporting checklist. Available at https://jovs.amegroups.org/article/view/10.21037/jovs-23-17/rc
Peer Review File: Available at https://jovs.amegroups.org/article/view/10.21037/jovs-23-17/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.org/article/view/10.21037/jovs-23-17/coif). The series “Robotic Thoracic Surgery: Established Procedures & Current Trends” was commissioned by the editorial office without any funding or sponsorship. GJK served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Journal of Visualized Surgery from January 2023 to December 2024. WW reported teaching grant from Covidien (Metronic) and participation on the advisory board of Astra Zeneca. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Informed consent was obtained from all patients prior to inclusion in the study and the study was approved by our institutional review board (No. TS2022.09). A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wise R. Seventh cervical rib associated with subclavian artery occlusion and multiple infarcts: case report. J Neurosci Nurs 2008;40:169-72. [Crossref] [PubMed]
- Chang KZ, Likes K, Davis K, et al. The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg 2013;57:771-5. [Crossref] [PubMed]
- Gruber W. Ueber die Halsrippen des Menschen mit vergleichend-anatomischen Bemerkungen. In: No. 22. Commissionnaires de l’Académie Impériale des Sciences; 1869.
- Halsted WS. An experimental study of circumscribed dilation of an artery immediately distal to a partially occluding band, and its bearing on the dilation of the subclavian artery observed in certain cases of cervical rib. J Exp Med 1916;24:271-86. [Crossref] [PubMed]
- Lewis T, Pickering GW. Observations upon maladies in which the blood supply to digits ceases intermittently or permanently, and upon bilateral gangrene of digits; observations relevant to so-called “Raynaud’s disease.” Clin Sci 1934;1:327-66.
- Wybaillie E, Maene L, Cooreman F, et al. Robotically Assisted Transthoracic Cervical Rib Resection. Ann Thorac Surg 2018;106:e253-5. [Crossref] [PubMed]
- Abdel Ghany W, Nada MA, Toubar AF, et al. Modified Interscalene Approach for Resection of Symptomatic Cervical Rib: Anatomic Review and Clinical Study. World Neurosurg 2017;98:124-31. [Crossref] [PubMed]
- Kocher GJ, Zehnder A, Lutz JA, et al. First Rib Resection for Thoracic Outlet Syndrome: The Robotic Approach. World J Surg 2018;42:3250-5. [Crossref] [PubMed]
- Zehnder A, Dorn P, Lutz J, et al. Completely Thoracoscopic 3-Port Robotic First Rib Resection for Thoracic Outlet Syndrome. Ann Thorac Surg 2022;114:1238-44. [Crossref] [PubMed]
- Morjaria JB, Aslam I, Johnson B, et al. Bilateral chylothorax: an unusual complication of cervical rib resection. Ther Adv Chronic Dis 2015;6:29-33. [Crossref] [PubMed]
- Palivela N, Burt BM. Transthoracic Robotic First and Cervical Rib Resection for Thoracic Outlet Syndrome. Ann Surg 2021; Epub ahead of print. [Crossref] [PubMed]
- Hussain MA, Aljabri B, Al-Omran M. Vascular Thoracic Outlet Syndrome. Semin Thorac Cardiovasc Surg 2016;28:151-7. [Crossref] [PubMed]
- Madden N, Calligaro KD, Dougherty MJ, et al. Evolving strategies for the management of venous thoracic outlet syndrome. J Vasc Surg Venous Lymphat Disord 2019;7:839-44. [Crossref] [PubMed]
- Morel J, Pirvu A, Elie A, et al. Functional Results of Cervical Rib Resection for Thoracic Outlet Syndrome: Impact on Professional Activity. Ann Vasc Surg 2019;56:233-9. [Crossref] [PubMed]
- Panther EJ, Reintgen CD, Cueto RJ, et al. Thoracic outlet syndrome: a review. J Shoulder Elbow Surg 2022;31:e545-61. [Crossref] [PubMed]
- Millan G, Casal D, Sagaribay A, et al. Neurogenic thoracic outlet syndrome associated with cervical rib. Acta Reumatol Port 2013;38:98-103. [PubMed]
- Wise R. Seventh cervical rib associated with subclavian artery occlusion and multiple infarcts: case report. J Neurosci Nurs 2008;40:169-72. [Crossref] [PubMed]
- Sen S, Dişçigil B, Boga M, et al. Thoracic outlet syndrome with right subclavian artery dilatation in a child - transaxillary resection of the pediatric cervical rib. Thorac Cardiovasc Surg 2007;55:339-41. [Crossref] [PubMed]
- Weber AE, Criado E. Relevance of bone anomalies in patients with thoracic outlet syndrome. Ann Vasc Surg 2014;28:924-32. [Crossref] [PubMed]
- Hines K, Graf E, Liu D, et al. The rare case of cervical rib fusion to the second rib. Ann Vasc Surg 2014;28:742.e5-8. [Crossref] [PubMed]
- Reidler JS, Das De S, Schreiber JJ, et al. Thoracic outlet syndrome caused by synostosis of the first and second thoracic ribs: 2 case reports and review of the literature. J Hand Surg Am 2014;39:2444-7. [Crossref] [PubMed]
- Coote H. Exostosis of the left transverse process of the seventh cervical vertebra, surrounded by blood vessels and nerves; successful removal. Lancet 1861;1:19861.
- Peek J, Vos CG, Ünlü Ç, et al. Outcome of Surgical Treatment for Thoracic Outlet Syndrome: Systematic Review and Meta-Analysis. Ann Vasc Surg 2017;40:303-26. [Crossref] [PubMed]
- Gelabert HA, Rigberg DA, O'Connell JB, et al. Transaxillary decompression of thoracic outlet syndrome patients presenting with cervical ribs. J Vasc Surg 2018;68:1143-9. [Crossref] [PubMed]
- Moridzadeh RS, Gelabert MC, Rigberg DA, et al. A novel technique for transaxillary resection of fully formed cervical ribs with long-term clinical outcomes. J Vasc Surg 2021;73:572-80. [Crossref] [PubMed]
- Vemuri C, McLaughlin LN, Abuirqeba AA, et al. Clinical presentation and management of arterial thoracic outlet syndrome. J Vasc Surg 2017;65:1429-39. [Crossref] [PubMed]
- Palivela N, Lee HS, Jang HJ, et al. Improvement of Disability in Neurogenic Thoracic Outlet Syndrome by Robotic First Rib Resection. Ann Thorac Surg 2022;114:919-25. [Crossref] [PubMed]
- Zehnder A, Lutz J, Dorn P, et al. Robotic-Assisted Thoracoscopic Resection of the First Rib for Vascular Thoracic Outlet Syndrome: The New Gold Standard of Treatment? J Clin Med 2021;10:3952. [Crossref] [PubMed]
- Strother E, Margolis M. Robotic First Rib Resection. Operative Techniques in Thoracic and Cardiovascular Surgery 2015;20:176-88. [Crossref]
- Burt BM, Palivela N, Karimian A, et al. Transthoracic robotic first rib resection: Twelve steps. JTCVS Tech 2020;1:104-9. [Crossref] [PubMed]
- Gharagozloo F, Meyer M, Tempesta B, et al. Robotic transthoracic first-rib resection for Paget-Schroetter syndrome. Eur J Cardiothorac Surg 2019;55:434-9. [Crossref] [PubMed]
- Burt BM, Palivela N, Cekmecelioglu D, et al. Safety of robotic first rib resection for thoracic outlet syndrome. J Thorac Cardiovasc Surg 2021;162:1297-1305.e1. [Crossref] [PubMed]
- Gharagozloo F, Meyer M, Tempesta BJ, et al. Robotic en bloc first-rib resection for Paget-Schroetter disease, a form of thoracic outlet syndrome: technique and initial results. Innovations (Phila) 2012;7:39-44. [Crossref] [PubMed]
- Ferris S, Lonie S. Bilateral Thoracic Outlet Syndrome from Anomalous 8th Cervical Vertebrae Ribs. J Brachial Plex Peripher Nerve Inj 2022;17:e30-2. [Crossref] [PubMed]
Cite this article as: Zehnder A, Gelpke H, Weder W, Stalder P, Jung F, Kocher GJ. Robotic-assisted first and supernumerary rib resection: case series. J Vis Surg 2023;9:35.