Wide local excision of perianal Paget’s disease with gluteal flap reconstruction: an interdisciplinary approach
Introduction
Perianal Paget’s disease (PPD) is an extremely rare condition describing an intraepithelial adenocarcinoma of the anal margin (1). PPD accounts for 20% of extramammary Paget’s disease (EMPD) cases (2). EMPD typically occurs in elderly people, affecting their anogenital region (3). PPD is a type of EMPD that specifically affects the tissues surrounding the anal region (3). Rates of synchronous or metachronous malignancies in PPD range from 33% to 86% (4). In EMPD, the location of other malignancies tends to be related to the location of the EMPD itself (4). The same principal applies to PPD. Like most malignant diseases, prognosis is related to the degree of invasion (3). When no invasive component is identified, patients tend to have a good prognosis; when there is invasion into the dermis and beyond, the prognosis worsens (3).
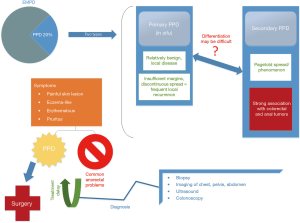
The etiology of PPD remains unclear (1,5). Paget’s cells on biopsy are a pathognomonic feature. The origin of Paget’s cells may be apocrine gland cells based on the observation that there is increased apocrine gland density within the lesions (5). There are two types of PPD: primary and secondary (1,4,5). Primary PPD is described as a relatively benign, local disease (4). However, discontinuous spread and insufficient resection margins often lead to frequent local recurrence (4). Secondary PPD, also known as Pagetoid spread or Pagetoid phenomenon, is strongly associated with colorectal and anal tumors, often from a downward spread of rectal adenocarcinoma (4,5). Although differentiation between primary and secondary PPD is not always clear-cut, such differentiation can be achieved through immunohistochemical analysis (3-5) (Figure 1).
We present a case of PPD treated with wide local excision (WLE) of the anus and perianal soft tissue followed by immediate reconstruction using gluteal advancement flaps. This case highlights surgical technique and the use of an interdisciplinary surgical team to achieve an excellent oncologic and functional outcome.
Methods
Patient selection and workup
A 61-year-old overweight female (BMI 28 kg/m2) presented with painful skin lesions in the posterior lateral perianal regions along with rectal pain and intermittent pruritus for the past two years. The patient had a history of colon polyps. Otherwise, she had no personal history of prior malignancy. Her family history was significant for a father diagnosed with colon cancer. Physical examination revealed a 6 cm × 8 cm left-sided perianal skin lesion along with a 5 cm × 6 cm right-sided perianal skin lesion. These lesions connected at the posterior aspect of the anal verge. Both lesions were erythematous and scaly in appearance and they were weeping serous fluid. Pre-operative work-up included an exam under anesthesia with biopsy, endorectal and endoanal ultrasonography, linear ultrasonography of the involved dermis, colonoscopy, and magnetic resonance imaging (MRI) of the pelvis. They failed to show invasive disease into the bowel or evidence of lymph node metastasis. While the ultrasound did reveal very minimal extension into the subcutaneous tissue underlying the diseased region, no significant sphincter involvement was found. Biopsies of the lesions were consistent with primary PPD.
Following a thorough discussion of treatment options and associated benefits and risks with the patient, we decided to proceed with a WLE of the PPD along with gluteal flap reconstruction. Risks and complications of the procedure included infection, bleeding, scarring, damage to the surrounding structures, wound dehiscence, flap failure, anal stricture, anal ectropion, neurovascular damage, chronic wound and pain, and the need for further surgeries. The patient understood these risks in addition to the need for the placement of a protective ileostomy, which we felt was necessary to aid in wound healing and decrease significant pain that the patient had already been experiencing.
A WLE with associated reconstruction of the buttocks was ideally suited for a lesion of such characteristics in lieu of other aforementioned techniques. By choosing the WLE over local excision, we were able to best avoid recurrence due to insufficient margins. An APR was avoided since earlier examinations revealed the disease did not extend into the anal canal or lower rectum. For reconstruction of the perianal defect, a V-Y advancement of bilateral gluteus maximus fasciocutaneous flaps was chosen due the technique’s simplicity, aesthetical superiority, and previous positive outcomes with WLE. These decisions were made pre-operatively and discussed with the patient. Thus, with a WLE, we increased our certainty in avoiding a histological recurrence while maximizing successful patient outcome.
Pre-operative preparation
Prior to the procedure, complete blood count, liver function test, basic metabolic panel, and carcinoembryonic antigen tests were ordered (all normal) in addition to a full physical examination and patient history. A bowel prep was also completed prior to the procedure. Antibiotics, ciprofloxacin and metronidazole, were administered in that sequence no more than 30 minutes prior to the incision. Appropriate consent was obtained from the patient per our institutional protocol.
Equipment preference card
- Fine-tip and regular-tip electrocautery;
- 3–0 and 2–0 Vicryl sutures;
- Hill-Ferguson and Pratt retractors;
- Lone Star retractor;
- Nerve stimulator/identifier;
- Anorectal tray;
- Plastic surgery tray;
- Headlight;
- Forceps and skin scalpel.
Procedure (Figure 2)

The patient was initially placed in the supine position. After general anesthesia was induced, a Foley catheter was placed. Prior to beginning the WLE of the lesion, a laparoscopic protective loop ileostomy was created. Afterwards, the patient was placed in the prone jackknife position with the buttocks taped apart. The anal canal and perianal skin were prepped with povidone-iodine solution.
A 1.5-cm margin was marked around the lesion. We then used the skin scalpel in conjunction with electrocautery. The involved area was excised with the associated dermal, subcutaneous, and adipose tissues. This dissection was continued toward the anal canal circumferentially exposing the external anal sphincter muscle and proceeding proximally to the dentate line.
Particular attention was paid to meticulous homeostasis, especially around the area of anal canal musculature where approximately 25% of the outer distal external sphincter muscle was resected in order to obtain a clear margin. The distal-most aspect of the anal canal was included with the resected specimen. The mucosal margin was divided several millimeters proximal to the dentate line.
Intraoperative frozen pathological evaluation suggested disease free margins. The retracted mucosa was stabilized with several interrupted number 3–0 Vicryl stiches to prevent proximal retraction of anoderm and potential anal stenosis in the future. This included full thickness sutures through the remaining distal canal. A small, anterior, right sided portion of anoderm in the anal mucosa was intact and not affected by PPD. That portion was approximated with 3–0 Vicryl simple interrupted sutures as well. Once that was complete, moist gauze was placed with Ioban over the anorectal region and the plastic surgery team began the gluteal reconstruction. A sterile Doppler was used to identify perforating vessels of the inferior gluteal artery and veins. Based on those perforators, left rotation and right advancement fasciocutaneous gluteal flaps were designed. The flaps were inset over two Jackson-Pratt drains and secured to the deeper fascia. Finally, the skin of the flaps was sutured to the stabilized sphincter complex. This resulted in a well-vascularized fully patent anal reconstruction. Afterwards, primary wound approximation was performed at the donor site.
Role of team members
- Colorectal team performed temporary, protective ileostomy and WLE of PPD;
- Plastic surgery team performed gluteal reconstruction.
Postoperative management
Following the procedure, the patient was admitted to the surgical floor and remained on an air mattress throughout her stay with an epidural and IV acetaminophen for pain management (7 days as per plastic surgery recommendations). She was discharged after an uneventful postoperative course. Final pathology confirmed clear surgical margins.
On 3 months follow up examination, the surgical site had healed without flap compromise. The anal lumen remained widely open. Full sphincter control was demonstrated.
Subsequently, the ileostomy was reversed and the patient regained normal function.
Results
Tips, tricks, and pitfalls
- Maintenance of meticulous hemostasis and particular care must be taken when excising around the area of anal canal musculature to preserve maximal function of sphincter;
- Creation of temporary, protective loop ileostomy should be considered prior to such a procedure in order to protect the operative wound from fecal contamination, and help with postoperative pain;
- The standard oncologic principles should be followed, especially when handling large surface specimens; no-touch technique and coverage of the exposed cancerous area is recommended;
- If partial excision of the anal canal or anoderm is performed, the proximal anoderm can be secured to the residual muscle to prevent it from retracting back into the anus (anoderm stabilization). The skin flap is then sutured also to the muscle, giving it better anchoring;
- Although not shown in the video (Figure 3), marking proper orientation of the excised tissue with various colors and lengths of sutures can prove helpful to yield correct results from pathology.

Discussion
As with EMPD cases, PPD typically presents as a painful skin lesion that is eczema-like, erythematous, and associated with pruritus (1,4,5,7) (Figure 3). Diagnosis of PPD itself tends to be considered after a lack of response to local treatments (4,5). Since symptoms of PPD are similar to those seen in common anorectal problems such as hemorrhoids, anal fissures, and pruritus ani, PPD is commonly mistaken as one or more of those conditions (5). This often causes a diagnostic and therapeutic delay, which may range from 2–8 years (4,5). Biopsy and resultant histology are typically used to obtain a PPD diagnosis, along with imaging of the chest, abdomen, and pelvis to rule out metastatic disease (1-5,7).
The preferred treatment for PPD is surgical excision of the lesion(s) (1-5,7). Surgical techniques that can be used to excise PPD include local excision and WLE. For very advanced lesions, abdominoperineal resection may be the only good option (1). The length of macroscopically clear surgical margins differentiates a local excision and WLE. Local excision aims for margins between 0.5 and 1 cm whereas WLE aims for margins over 1 cm (1). A WLE aims to avoid insufficient resection margins, a common cause of primary PPD recurrence (1). Since it is difficult to know how far the carcinoma may extend into the underlying tissues, excising beyond visible margins may reduce recurrence. On the other hand, in the study by Isik et al., each technique mentioned earlier provided comparable survival for PPD patients (1).
When performing a WLE or APR, a reconstruction of the perineum and surrounding tissues is almost always necessary (5). There have been multiple reconstructive techniques described in the literature including split thickness skin graft (STSG), S flap reconstruction, house flap, bilateral V-Y advancement flap, and simultaneous V-Y advancement flap with STSG (1,2,4). In cases of WLE, the V-Y advancement of bilateral gluteus maximus fasciocutaneous flaps was the preferred method of reconstruction due to less scarring, superior aesthetic results, lower risks of infection when compared to STSG, among other benefits (8,9).
Conclusions
We have demonstrated a case where a WLE with gluteal flap reconstruction is a feasible technique for treating PPD. An interdisciplinary surgery team was essential for the success of this approach. The colorectal team made the decision to perform a WLE after the metastatic workup revealed no lesions or cause for suspecting metastasis. The plastic surgery team performed the bilateral V-Y gluteal advancement flaps for reconstruction of the anal and perianal defect. The patient recovered uneventfully with no evidence of PPD recurrence and no flap compromise. Although the rarity of these problems make it difficult to study, further studies to evaluate this technique against less-commonly attempted primary PPD treatments such as Mohs’ surgery or non-surgical means could prove beneficial.
Acknowledgements
The authors would like to acknowledge the James R. and Helen D. Russell Institute for Research and Innovation at Advocate Lutheran General Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Isik O, Aytac E, Brainard J, et al. Perianal Paget's disease: three decades experience of a single institution. Int J Colorectal Dis 2016;31:29-34. [Crossref] [PubMed]
- Goto H, Yoshida Y, Kiyohara Y, et al. Stoma creation for treatment of primary perianal Paget's disease. Eur J Dermatol 2015;25:73-4. [PubMed]
- Ito T, Kaku Y, Nagae K, et al. Tumor thickness as a prognostic factor in extramammary Paget's disease. J Dermatol 2015;42:269-75. [Crossref] [PubMed]
- Bontinck H, Bontinck J, Rondou T, et al. Perianal Paget's disease: case report and review of the literature. Acta Chir Belg 2016.1-6. [Epub ahead of print]. [Crossref] [PubMed]
- Perez DR, Trakarnsanga A, Shia J, et al. Management and outcome of perianal Paget's disease: a 6-decade institutional experience. Dis Colon Rectum 2014;57:747-51. [Crossref] [PubMed]
- Borsuk DJ, Melich G, Marecik SJ, et al. Wide local excision (WLE) of perianal Paget’s disease (PPD) with bilateral V-Y advancement flap reconstruction of the buttocks. Asvide 2016;3:373. Available online: http://www.asvide.com/articles/1142
- Liao X, Mao W, Lin A. Perianal Paget's Disease Co-Associated with Anorectal Adenocarcinoma: Primary or Secondary Disease? Case Rep Gastroenterol 2014;8:186-92. [Crossref] [PubMed]
- Sasaki K, Nozaki M, Kikutchi Y, et al. Reconstruction of perianal skin defect using a V-Y advancement of bilateral gluteus maximus musculocutaneous flaps: reconstruction considering anal cleft and anal function. Br J Plast Surg 1999;52:471-5. [Crossref] [PubMed]
- Kwon KH, Lee DG, Koo SH, et al. Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg 2012;39:619-25. [Crossref] [PubMed]
Cite this article as: Borsuk DJ, Melich G, Sugrue J, Calata J, Seitz IA, Park JJ, Prasad LM, Marecik SJ. Wide local excision of perianal Paget’s disease with gluteal flap reconstruction: an interdisciplinary approach. J Vis Surg 2016;2:159.