
Uniportal robotic-assisted thoracic surgery for mediastinal tumor resection via the lateral intercostal approach: a surgical technique and our ingenuity
Highlight box
Key findings
• Uniportal robotic-assisted thoracic surgery (URATS) for the mediastinal tumors may be safe, feasible, and less invasive than multiportal RATS (MRATS).
• URATS using the da Vinci Xi system. requires specific techniques and surgical skills.
What is known and what is new?
• RATS for the mediastinal tumors is conventionally performed via four to five incisions, but URATS has not been widely reported.
• To know the detailing the surgical technique of URATS using the da Vinci Xi system is helpful.
What is the implication, and what should change now?
• URATS using the da Vinci Xi system is safe and feasible, with perioperative outcomes.
• URATS using the da Vinci Xi system is especially useful for patients who need an intercostal approach and can be performed in hospitals that do not have the da Vinci SP system.
• Future advances in robotic technology will aid in the transition from MRATS to URATS.
Introduction
Background
In recent decades, the robotic-assisted approach has become an established alternative technique to traditional video-assisted thoracoscopic surgery (VATS) and open surgery for the treatment of many thoracic diseases (1). Robotic-assisted thoracic surgery (RATS) using a three-arm robotic approach with the aid of CO2 insufflation is effective and reliable for the resection of a posterior mediastinal tumor (2).
Rationale
The possibility of blending the uniportal approach with robotic technology would bring enormous improvements in feasibility, safety and postoperative recovery. Although there are increasing reports of uniportal RATS (URATS) using the da Vinci single-port (SP) system (3), only a few reports have detailed the surgical technique of URATS using the da Vinci Xi system.
Objective
Our objective was to report the surgical technique of URATS using the da Vinci Xi system and describe the port placement devices. This surgical technique causes minimal injury and is useful for mediastinal tumor resection in hospitals that do not have a da Vinci SP system. We present this article in accordance with the SUPER reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-30/rc).
Preoperative preparations and requirements
Under general anesthesia, the patient is intubated with a double-lumen endotracheal tube and placed in the lateral decubitus position with horizontal adjustment of the thorax and iliac crest. A skin incision of approximately 4 cm is made in the fifth, sixth, or seventh intercostal space on the midaxillary line and protected with a non-traumatic ring wound protector (Alexis Wound Retractor XS®; Applied Medical, Rancho Santa Margarita, CA, USA).
The da Vinci Xi Surgical System® (Intuitive Inc., Sunnyvale, CA, USA) is positioned at the patient’s posterior side, and the boom of the patient cart is rotated 30 degrees along the patient’s intercostal space alignment. The positioning laser is set above the upper part of the wound and adjusted in the ventral-dorsal direction. The arm farthest from the patient is canceled and the intrathoracic traditional targeting, remote center system, and CO2 insufflation are not used.
The 30-degree robotic camera is used and the operation is basically performed under a downward-looking view. However, depending on the tumor location and size, an upward-looking view may be required. The camera is placed on the tumor side of the wound, with the left-hand arm in the middle and the right-hand arm on the opposite side to avoid collision. The instruments are chosen according to the surgeon’s preference, but usually comprise Maryland bipolar forceps in the right hand and a fenestrated grasper or long bipolar forceps in the left hand. It is important to be aware that the angle between the left arm and the right arm should be 180 degrees vertically so that the arms do not interfere with each other. For example, robotic right arm is above in the monitor and left arm is under. If the arms become locked due to interference, this can be remedied by moving the camera or synchronizing both hands. The uniportal VATS instruments (long curved suction, cotton holder, and lymph node forceps) are very useful for the assistant to facilitate the development of the operative field.
Each hospital surgical team consisted of three surgeons: one main surgeon at the console, and two as bedside assistants. One surgeon from Yamagata University Hospital was always present at each surgery to share information. Our surgical team consists of a total of six skillful thoracic surgeons. Before the introduction of URATS, each surgeon performed multiportal RATS or UVATS.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). This study was approved by the Institutional Review Board of the Ethics Committee of Yamagata University (No. S-50) and Tokyo Metropolitan Bokutoh Hospital (No. 05-030). Written informed consent was obtained from the patients for publication of this manuscript, any accompanying images and videos. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
Case 1: resection of an anterior mediastinal tumor
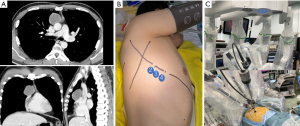
A 42-year-old man had a lesion detected in the right side of his chest in an annual health check-up and was referred to our department. Chest computed tomography (CT) revealed a homogeneous 5 cm mass in the anterior mediastinum with calcification in the wall (Figure 1A). A thymic cyst was considered, but the patient strongly desired surgery. URATS was planned and performed through a 3.5 cm wound in the fifth intercostal space at the midaxillary line (Figure 1B). The da Vinci Xi Surgical System® was positioned at the patient’s posterior side and the positioning laser was set above the upper part of the wound and adjusted in the ventral-dorsal direction. Port placement during anterior mediastinal tumor resection is shown in Figure 1C. The first arm, which was farthest from the patient, was canceled, and surgery was performed with Maryland bipolar forceps (right hand) in the second arm, long bipolar forceps (left hand) in the third arm, and a 30-degree strabismus camera in the fourth arm. The console time was 54 minutes and the blood loss volume was 1 mL. The thoracic drain was removed the day after surgery, and the patient was discharged on the second postoperative day. The intraoperative frozen section diagnosis was a thymic cyst, but the final pathological diagnosis was a cystic thymoma (Masaoka stage I and World Health Organization type AB). The patient recovered smoothly and there has been no evidence of recurrence during six months of follow-up. A video of the procedure was uploaded to YouTube by H.E., MD (Video 1) (4).
Case 2: resection of a posterior mediastinal tumor
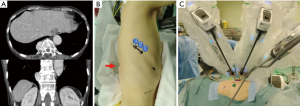
A 78-year-old woman had a posterior mediastinal mass detected on CT performed as part of her annual health check-up. Chest CT showed a 3.1 cm right paravertebral lesion at the level of Th11 (Figure 2A). She was asymptomatic and had no neurological symptoms. The preoperative diagnosis was a neurogenic tumor. She was scheduled for URATS for diagnostic and therapeutic purposes. We performed URATS through a 3.5 cm wound in the seventh intercostal space at the midaxillary line (Figure 2B). The da Vinci Xi Surgical System® was positioned at the patient’s posterior side, the positioning laser was set above the upper part of the wound and adjusted in the ventral-dorsal direction, and the boom of the patient cart was rotated dorsal-foot along the patient’s intercostal space alignment. Port placement during posterior mediastinal tumor resection is shown in Figure 2C. The fourth arm, which was farthest from the patient, was canceled, and surgery was performed with Maryland bipolar forceps (right hand) in the second arm, long bipolar forceps (left hand) in the first arm, and a 30-degree strabismus camera in the third arm. The tumor was tractioned with rounded gauze held with the fenestrated grasper’s left arm, and the pleura was incised with Maryland bipolar forceps held with the right arm. The console time was 56 minutes and the blood loss volume was 2 mL. The thoracic drain was removed the day after surgery, and the patient was discharged on the second postoperative day. The pathological diagnosis was a solitary fibrous tumor with complete resection. The patient recovered smoothly and there has been no evidence of recurrence during five months of follow-up. An intraoperative video is provided (Video 2).
Postoperative considerations and tasks
After tumor resection, hemostasis is checked and a leak test is performed to ensure that there is satisfactory lung expansion and no lung injury. A single chest drain is inserted in the thoracic cavity, and the wound is closed. The chest drain is removed four hours after surgery or the next morning, depending on the time the surgery is finished. The chest drain was placed at one end of the incision wound. Patients are allowed to drink water from two hours after surgery and start eating on the day of surgery. Analgesia is achieved by administering non-steroidal anti-inflammatory drugs three times daily starting on the day of surgery. Patients are discharged one or two days after drain removal following the confirmation of no abnormal findings on blood tests and normal lung expansion on chest radiographs.
Tips and pearls
URATS technique can be performed by following the preoperative preparations and requirements.
Docking of the da Vinci Xi can be performed quickly and easily because of less skin incision. It is important to be aware that the angle between the left arm and the right arm should be 180 degrees vertically so that the arms do not interfere with each other. For example, robotic right arm is above in the monitor and left arm is under. If the arms become locked due to interference, this can be remedied by moving the camera or synchronizing both hands. Once these new movements are mastered and the correct technique is learned, the collision never happens in experienced URATS surgeons.
There is no study on the URATS mediastinal tumor resection learning curve, but the experience in the uni-portal VATS technique is expected to shorten this period.
Discussion
Surgical highlights
VATS has been commonly used for mediastinal tumor resections for over 20 years. Several studies have demonstrated that the safety and oncological outcomes of VATS are not inferior to median sternotomy (5,6). With the development of endoscopic instruments and VATS techniques, uniportal VATS lung resection is being used for a growing number of applications (7). Suda et al. described their experience with infrasternal uniportal VATS thymectomy in 2014 (8). However, although uniportal VATS may be useful for the resection of an anterior mediastinal tumor, it would be difficult to use this technique for the resection of a middle or posterior mediastinal tumor. Therefore, uniportal VATS via an intercostal approach is now commonly used to resect posterior mediastinal tumors (9).
RATS is very useful in mediastinal tumor resections because it enables precise surgical manipulation. In particular, the number of RATS procedures for thymoma is increasing, and it has been reported that the surgery time, duration of postoperative hospitalization, and recurrence rate are almost equivalent to those of VATS (10). In 2019, Ishikawa et al. first published their experience with URATS, which comprised single-incision robotic surgery using the cross-arm technique with the da Vinci system® (11). Gonzalez-Rivas et al. performed the first URATS lobectomy without using cross-arm technology with the da Vinci Xi System® (12). The URATS technique has also been applied to advanced surgeries such as bilobectomy and sleeve lobectomy (13,14). With this surgical video demonstration, we intend to demonstrate the surgical technique and tips for URATS approaches the da Vinci Xi system for mediastinal tumors.
Strengths and limitations
This surgical technique has some limitations. First, assistants must have acquired the skills required for uniportal VATS to assist with URATS. In particular, because the three robotic arms each have an 8 mm cannula, the utility port is narrower in URATS than in uniportal VATS. Second, because robotic arms are thicker (8 mm cannula) than the uniportal VATS forceps, there can be interference between devices. If the arms are locked due to interference, this can be remedied by moving the camera or synchronizing both hands. It is important to be aware that the angle between the left arm and the right arm should be 180 degrees vertically so that the arms do not interfere with each other. Thirds, the indications for URATS are controversial. The URATS procedure requires extensive experience with RATS when manipulating a wide range of operative fields such as those required for thymectomy or for the removal of large tumors. URATS might be challenging for extended thymectomy because the left phrenic nerve cannot be identified when the right intercostal approach is used. For this reason, we think that this URATS via the lateral intercostal approach with the da Vinci Xi platform is indicated for simple mediastinal tumor resection. Finally, in our limited experience, it is unclear that a single 4 cm incision is demonstrably superior to four 1cm incisions with the robot. However, it is important to note that there were no patients converted from URATS to multiple-portal RATS or open thoracotomy, which further suggests that URATS is a safe and feasible procedure for the resection of non-invasive mediastinal tumors. Safety is the first consideration when new procedure is applied to patients. In the future, we aim to enroll more patients to validate our clinical findings.
We prefer the URATS approach for several reasons, but mainly because URATS lessens the postoperative trauma (15). Furthermore, from a surgical standpoint, the use of better visualization without the need to readjust the arms or ports translates into a safer and more time-effective procedure. We find that adapting each case to this URATS approach improves the surgical time, precision of the dissection, and postoperative recovery.
Comparison with other surgical techniques and research
In the last few years, a convergence of the uniportal approach and robotic-assisted surgery has resulted in a pure, SP robotic system: the da Vinci SP® (Intuitive Surgical; Sunnyvale, CA, USA). The da Vinci SP platform has a single 2.5 cm cannula through which an articulating three-dimensional camera and three fully articulating instruments with seven degrees of freedom can be passed. However, the da Vinci SP platform is too wide to use an approach via the intercostal space because of the 2.5 cm cannula. A few studies have reported that the subxiphoid and subcostal approaches are useful when using the da Vinci SP® (16). Given that the da Vinci Xi platform is suitable for all kinds of intrathoracic resections with excellent outcomes, the use of the da Vinci Xi system for URATS is a realistic alternative to the da Vinci SP platform. The comparison between different systems the da Vinci Xi system® and the da Vinci SP® platform are shown in Table 1.
Table 1
| Types of the da Vinci | The da Vinci SP® | The da Vinci Xi® |
|---|---|---|
| Features | Camera is equipped with an articulating function, allowing the angle and direction to be freely manipulated | It is basically designed on a platform with four arms. The camera can be connected to any of the arms |
| Advantages | Minimal interference between arms | Cannula is thin (8 mm) |
| Suitable for intercostal approach | ||
| Disadvantages | Cannula is thick (25 mm) | Interference occurs between arms |
SP, single-port.
Implications and actions recommended
Our report provides further confirmation that the URATS approach can be successfully used for the surgical resection of mediastinal tumors, as shown by the complete resection and uneventful postoperative courses achieved in these two cases.
Conclusions
The URATS approach using the da Vinci Xi system presents a promising alternative for simple mediastinal tumor resection, though challenges remain. However, the camera and forceps of the da Vinci Xi system are still relatively thick (8 mm), and interference between devices is a problem. Further advances in robotics-related technologies are eagerly awaited.
Acknowledgments
The authors would like to thank Kelly Zammit, BVSc, from Edanz (https://jp.edanz.com/) for editing a draft of this manuscript.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-30/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-30/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-30/coif). Both J.S. and H.U. serve as unpaid editorial board members of Journal of Visualized Surgery from September 2023 to August 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the Helsinki Declaration (as revised in 2013). This study was approved by the Institutional Review Board of the Ethics Committee of Yamagata University (No. S-50) and Tokyo Metropolitan Bokutoh Hospital (No. 05-030). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images and videos. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cerfolio R, Louie BE, Farivar AS, et al. Consensus statement on definitions and nomenclature for robotic thoracic surgery. J Thorac Cardiovasc Surg 2017;154:1065-69. [Crossref] [PubMed]
- Guo W, Yang S, Jin R, et al. Robot-assisted surgery for posterior superior mediastinal mass. AME Med J 2017;2:10. [Crossref]
- Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors. Part II. Tumors of the middle and posterior mediastinum. Chest 1997;112:1344-57. [Crossref] [PubMed]
- Hiroki E. Uniportal RATS for anterior mediastinal tumor. Uploaded to YouTube by Hiroki Ebana MD, PhD, on 8 Apr 2023. Available online: https://www.youtube.com/watch?v=BZfyBpQRZdk.
- Rückert JC, Walter M, Müller JM. Pulmonary function after thoracoscopic thymectomy versus median sternotomy for myasthenia gravis. Ann Thorac Surg 2000;70:1656-61. [Crossref] [PubMed]
- Shigemura N, Shiono H, Inoue M, et al. Inclusion of the transcervical approach in video-assisted thoracoscopic extended thymectomy (VATET) for myasthenia gravis: a prospective trial. Surg Endosc 2006;20:1614-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [Crossref] [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Wu CY, Heish MJ, Wu CF. Single port VATS mediastinal tumor resection: Taiwan experience. Ann Cardiothorac Surg 2016;5:107-11. [Crossref] [PubMed]
- O'Sullivan KE, Kreaden US, Hebert AE, et al. A systematic review of robotic versus open and video assisted thoracoscopic surgery (VATS) approaches for thymectomy. Ann Cardiothorac Surg 2019;8:174-93. [Crossref] [PubMed]
- Ishikawa N, Oda M, Kawachi K, et al. Robot-assisted single-port surgery for mediastinal tumors. Surg Today 2019;49:96-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bosinceanu M, Manolache V, et al. Uniportal fully robotic-assisted major pulmonary resections. Ann Cardiothorac Surg 2023;12:52-61. [Crossref] [PubMed]
- Manolache V, Motas N, Bosinceanu M, et al. Comparison of uniportal robotic-assisted thoracic surgery pulmonary anatomic resections with multiport robotic-assisted thoracic surgery: a multicenter study of the European experience. Ann Cardiothorac Surg 2023;12:102-9. [Crossref] [PubMed]
- Paradela M, Garcia-Perez A, Fernandez-Prado R, et al. Uniportal robotic versus thoracoscopic assisted surgery: a propensity score-matched analysis of the initial 100 cases. Ann Cardiothorac Surg 2023;12:23-33. [Crossref] [PubMed]
- Manolache V, Gonzalez-Rivas D, Bosinceanu M, et al. Uniportal robotic-assisted thoracic surgery for mediastinal tumors. Ann Cardiothorac Surg 2023;12:139-41. [Crossref] [PubMed]
- Park SY, Lee JH, Kim YH, et al. Multi-institutional surgical outcomes of robotic single-port surgery: a Korean experience. Ann Cardiothorac Surg 2023;12:41-5. [Crossref] [PubMed]
Cite this article as: Watanabe H, Ebana H, Suzuki J, Ujiie H, Ichiba H, Hoshijima K, Kobayashi A, Shiono S. Uniportal robotic-assisted thoracic surgery for mediastinal tumor resection via the lateral intercostal approach: a surgical technique and our ingenuity. J Vis Surg 2024;10:3.


