A rare case of Amyand’s hernia presenting as an appendicular mucocele, extending into retroperitoneum: a case report
Highlight box
Key findings
• The case reveals an unusual presentation of Amyand’s hernia as an extensive appendicular mucocele in a 74-year-old male. Surgical intervention involved complete dissection, excision of the lesion, and mesh hernioplasty, resulting in a successful recovery without complications.
What is known and what is new?
• Inguinal hernias are common, with Amyand’s hernia being a rare variant where the appendix is within the hernial sac. Diagnostic modalities like multidetector computed tomography scans, with multiplanar reformatted images play a crucial role in diagnosing Amyand’s hernia and its extent.
• The presented case introduces an atypical manifestation, with an extensive appendicular mucocele reaching into the retroperitoneum and involving the psoas muscle. This unique presentation has not been documented in reported cases, emphasizing the need for increased awareness of diverse Amyand’s hernia presentations.
What is the implication, and what should change now?
• The case underscores the importance of surgical expertise and timely imaging in managing complex hernia cases, particularly those involving appendicular mucocele. Clinicians should be vigilant for atypical presentations, and further research is warranted to explore the spectrum of Amyand’s hernia manifestations. The findings contribute to a deeper understanding of this rare condition, prompting heightened awareness and consideration during diagnosis and surgical interventions.
Introduction
Background
Inguinal hernias are the most common type of hernia, with sacs primarily comprising the small intestine or omentum. Amyand’s hernia is a rare type of inguinal hernia that manifests as an appendix herniating the inguinal canal (1). The incidence of such presentation is seen in about 1% of inguinal hernias.
Rationale and knowledge gap
The surgical treatment depends on the severity of the inflammation of the herniated appendix. Certain instances manifest as an appendiceal mucocele, characterised by formation of a cystic mass due to accumulation of mucus within the lumen of the appendix, with an incidence rate ranging from 0.2–0.7% (2). If this mucocele ruptures, it can result in pseudomyxoma peritonei, which is associated with a higher mortality rate. Treatment requires an immediate laparotomy or appendectomy to prevent the possibility of rupture.
Objective
The objective of this study is to contribute to the understanding of atypical presentation of Amyand’s hernia. We present a rare case involving an extensive appendicular mucocele and explore the surgical management and outcomes associated with this unique manifestation. Through this case report, our goal is to provide valuable insights that can enhance the existing knowledge on Amyand’s hernia, ultimately guiding and informing future interventions in similar cases. We present this article in accordance with the CARE reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-43/rc).
Case description
A 74-year-old male patient presented to our department with intermittent pain in the right groin for 15 years, which has gradually aggravated for the last 3 months. The patient has swelling in the right inguinal region that is non-reducible and non-tender on palpation (Figure 1). The pain aggravated on coughing or engaging in strenuous activities but relieved when laying supine. The patient exhibited no co-morbidities including no history of diabetes mellitus, hypertension, tuberculosis, bronchial asthma or epilepsy, and reported no significant medical or surgical history.

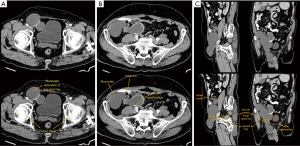
Initial investigations showed a total leukocyte count (TLC) of 10,600/microliters, haemoglobin level of 9.9 gm/dL, and an elevated erythrocyte sedimentation rate (ESR) of 88.6 mm/h. Liver and renal function tests were within normal limits. Screening for human immunodeficiency virus (HIV), hepatitis B surface antigen (HBsAg), and hepatitis C virus (HCV) was non-reactive. A computed tomography (CT) scan revealed a well-defined tubular cystic lesion originating from the base of the cecum in the right iliac fossa, measuring 4.4 cm in diameter and extending craniocaudally for 8.3 cm. Additionally, a 6.4-mm defect within this cystic lesion communicated with another tubular cystic structure. This structure extended inferiorly through the superficial inguinal ring into the scrotal sac, reaching up to the upper pole of the testis, with a maximum transverse diameter of 8.3 cm and a craniocaudal extent of 22.4 cm. Posteriorly, it abutting the right psoas muscle, and superiorly, it was adjacent to the base of the cecum. An ultrasound revealed heteroechoic contents within this cystic lesion (Figure 2A-2C).
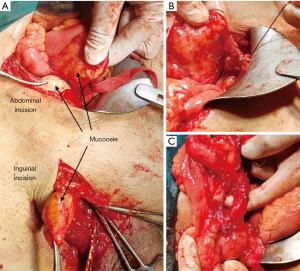
Surgery was planned based on these findings in July, 2023. Under general anaesthesia, after positioning the patient supine and proper draping and painting, a right lower inguinal incision was given. Intraoperative antibiotic prophylaxis was administered. After opening the skin and subcutaneous fascia, the external oblique aponeurosis was incised, and gentle exploration of the inguinal canal was done. A cystic pouch was identified and dissected, taking care of the vas deferens and the gonadal vessels (Figure 3A,3B).
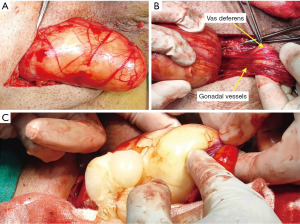
The cystic pouch was coming out of the deep inguinal ring and extending up to the scrotum through the superficial inguinal ring (measuring approximately 12 cm). To ease the dissection and to avoid underlying vasculature injury at the deep inguinal ring, thick paste-like mucus (approximately 200 mL) was evacuated from the pouch, and another horizontal incision at McBurney’s point was given to evaluate the intraabdominal extension of the pouch (Figures 3C,4A-4C).
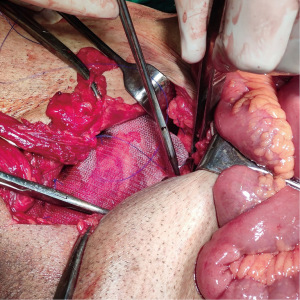
Intraabdominally, the body of the cystic pouch was so extensive that a part of it extended medially abutting the sigmoid colon and extended up to the inguinal ring (measuring approximately 10 cm), and the other part extended retroperitoneally up to the level of the psoas muscle (measuring approximately 13 cm), which was dissected (Figure 5A-5D).
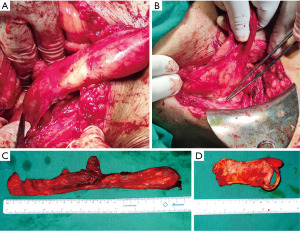
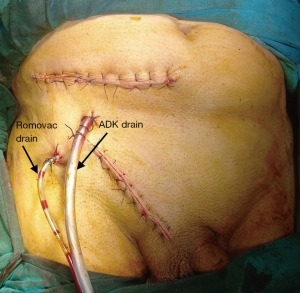
The entire cystic mass was meticulously dissected and excised using the abdominal approach along with the inguinal approach. The procedure concluded with mesh hernioplasty using Prolene 2-0, and the closure was done layer-wise after placing drains in the pelvis and the inguinal region (Figures 6,7).
Postoperative care entailed the continuous infusion of intravenous antibiotics and analgesics for optimal management of the patient. A one-day admission to the intensive care unit (ICU) was undertaken, and no postoperative fever was observed. The patient remained nil per oral (NPO) until the resumption of bowel sounds. Subsequent postoperative blood analyses revealed mild leukocytosis. Flatus and stool passage occurred on the second postoperative day. Diligent adherence to aseptic protocols was maintained during regular wound dressing, preventing any observed wound infections throughout the hospital stay. The patient commenced a fluid diet on the second day and transitioned to a solid diet on the third day.
The postoperative recovery was uneventful and the patient was discharged after 5 days of hospital stay for follow-up. The histopathological examination of the excised cystic soft tissue revealed a specimen measuring 3 cm × 0.5 cm × 0.3 cm, with a thickened wall and a prominent 1.5 cm × 1 cm × 1 cm hard calcified area within the cyst. Microscopic evaluation unveiled a predominant composition of fibro-collagenous tissue, accompanied by regions displaying chronic inflammatory infiltrates, congested blood vessels, and multiple areas of calcification. Notably, no atypia was observed suggestive of benign pathology. No notable complications or concerns were observed during the subsequent follow-up period.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Key findings
“Amyand’s hernia” was first described by Claudius Amyand in 1735, who successfully performed the first reported appendectomy for an inflamed appendix encountered during herniotomy on an 11-year-old boy (3). It is characterized by an incarcerated hernia that contains the appendix, which may manifest as either a normal or inflamed appendix.
The incidence of Amyand’s hernia in the medical literature is about 0.19% to 1.7% of all documented hernia cases (4). Of which the incidence of appendicular mucocele is only around 0.2–0.7% (2). The occurrence of a perforated appendix becoming incarcerated within an inguinal hernia is exceptionally rare, constituting merely 0.1% of all reported cases (5).
Amyand’s hernia typically arises because of extraluminal obstruction, primarily due to pressure exerted on the hernia neck, rather than intraluminal obstruction of the appendix (6,7). The contraction of abdominal muscles and abrupt increases in intra-abdominal pressure can lead to the compression of the appendix, which, in turn, can exacerbate inflammation (6). This increased pressure may impede the blood supply to the appendix, potentially leading to inflammation and bacterial overgrowth (6,8).
Losanoff and Basson proposed a classification system to determine the surgical approach for Amyand’s hernia, depending on the appendix’s status (9). For type 1 Amyand’s hernia, where the appendix is in a normal condition, mesh hernia repair is performed without appendectomy, unless the patient is of a young age. In types 2 to 4 hernias, appendectomy is routinely carried out. In the case of type 3, in addition to primary hernia repair, a laparotomy is required for abdominal irrigation, while type 4 necessitates further investigations into associated pathologies. In line with the Losanoff and Basson classifications, Rikki proposed a modified classification. This classification incorporated incisional hernias and included three subtypes: 5a (normal appendix with incisional hernia), 5b (acute appendicitis with incisional hernia and no abdominal sepsis), and 5c (acute appendicitis within an incisional hernia) (10) (Table 1).
Table 1
| Classification | Description | Surgical management |
|---|---|---|
| Type 1 | Normal appendix within an inguinal hernia | Hernia reduction, mesh repair, appendectomy in young patients |
| Type 2 | Acute appendicitis within an inguinal hernia, no abdominal sepsis | Appendectomy through hernia, primary repair of hernia, no mesh |
| Type 3 | Acute appendicitis within an inguinal hernia, abdominal wall, or peritoneal sepsis | Laparotomy, appendicectomy, primary repair of hernia, no mesh |
| Type 4 | Acute appendicitis within an inguinal hernia, related or unrelated abdominal pathology | Manage as types 1 to 3 hernia; investigate or treat second pathology as appropriate |
| Type 5a | Normal appendix within an incisional hernia | Appendicectomy through hernia, primary repair of hernia including mesh |
| Type 5b | Acute appendicitis within an incisional hernia, no abdominal sepsis | Appendectomy through hernia, primary repair of hernia |
| Type 5c | Acute appendicitis within an incisional hernia, abdominal wall, or peritoneal sepsis or in relation to previous surgery | Manage as type 4 |
The table is adapted from Saim HA, Chik I, Jaafar FF, et al. A rare presentation of low-grade appendiceal mucinous neoplasm within an amyand’s hernia: a case report. Ann Coloproctol 2023;39:183-7. Reuse with exemptions from licenses of the journal Annals of Coloproctology under the journal’s copyright policy CC BY-NC 4.0.
Strengths and limitations
The strength of this case report lies in its presentation of a unique and atypical manifestation of Amyand’s hernia, involving an extensive appendicular mucocele reaching into the retroperitoneum and the psoas muscle. The meticulous surgical procedure carried out, including the use of advanced imaging techniques and successful postoperative care, contributes valuable insights for managing complex Amyand’s hernia cases. However, limitations include the report being based on a single case, restricting generalizability.
Comparison with similar researches
A comprehensive review of documented cases of Amyand’s hernia was done. Bhatti et al. reported a type 2 hernia case in which an initial appendectomy was followed by mesh repair (11). In contrast, Morales-Cárdenas et al. described a type 1 case that was successfully managed with mesh repair without the need for appendectomy (12).
An additional study by Gao et al. (13) highlights the effectiveness of a combined approach involving appendectomy and tension-free mesh repair for patients with appendicitis. This was accompanied by postoperative antibiotic administration and pelvic drainage, which showed a reduction in the risk of postoperative infections (13).
Moreover, there are rare instances, as documented by Singal et al. (7), in which the presence of the appendix within an incisional hernia aligns with the management approach akin to type 4 cases. Remarkably, Singal et al. (7) also presented an extraordinary and intricate case featuring the coexistence of both the ascending and transverse colon within the inguinal hernial sac, extending into the scrotal region, along with the presence of the appendix. This case serves as a compelling and unusual illustration of Amyand’s hernia in clinical practice.
The mucocele is an uncommon condition, with an incidence of 0.2–0.3% among appendectomy cases, occurring more often in women than in men (3:1), typically affecting around the age of 55 years (14).
A study by Crăciun et al. (14) shows the presence of a perforated, phlegmonous, and dilated appendix in the hernia sac, displaced from the caecum, accompanied by purulent material around the appendix and fibrin deposits in their patient.
Another case reported by Anania et al. (15) wherein mucin’s deposits were discovered throughout various abdominal regions, notably concentrated in the pelvis, along the right parieto-colic space and involving the diaphragm. The treatment included pelvic peritonectomy, hystero-adnexectomy, Douglas ectomy, right hemicolectomy, and total omentectomy. Using diathermy, all the mucin’s nodes affecting the diaphragm, liver capsule, mesentery, and bowel serosa were excised. Subsequently, an ileo-colic anastomosis was performed, and the patient underwent intra-peritoneal chemohyperthermia.
Explanation of findings
Diagnosing Amyand’s hernia can be a formidable challenge, often necessitating confirmation during surgery. It is exceedingly uncommon to detect an inflamed appendix within an obstructed inguinal hernia solely through preoperative ultrasonography (USG). The most effective diagnostic approach for this clinical condition involves utilizing advanced imaging techniques like CT scans. A recent systematic review has confirmed that CT stands as the definitive diagnostic tool for patients with preoperative diagnoses (16).
Implications and actions needed
There is no non-surgical method for the management of Amyand’s hernia, as the consequences include gangrene, intra-abdominal sepsis, and potentially fatal if not addressed through surgical intervention. Appendicectomy is typically recommended when an inflamed appendix is present, and in such cases, the use of mesh is usually avoided. Generally, it is widely accepted that using mesh in infected cases should be avoided, as prosthetic material can exacerbate the inflammatory response, potentially leading to a higher incidence of wound infections (16). The use of mesh hernioplasty remains controversial and depends on the surgeon’s discretion. In our case, mesh hernioplasty was done considering the large size of the defect after dissecting the mucocele at the deep inguinal ring.
However, our case presents an unusual manifestation of appendicular mucocele that not only extends into the inguinal canal but also reaches into the retroperitoneum, encompassing the psoas muscle. A comprehensive literature search revealed that such an atypical presentation has not been documented in any reported cases.
Conclusions
Amyand’s hernia is an uncommon form of inguinal hernia that, when chronic, may lead to the emergence of an appendicular mucocele. Consequently, it is advisable to perform imaging to precisely assess the extent of this hernia. In our case, the presentation was unusual due to the extensive size of the appendicular mucocele, which extended to the caecum, sigmoid colon, deep inguinal ring reaching up to the upper pole of the testis, and even encroached into the retroperitoneal space, extending up to the psoas muscle.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-43/prf
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-43/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-43/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Heo TG. Amyand's hernia combined with contralateral recurrent inguinal hernia: A case report. Int J Surg Case Rep 2023;102:107837. [Crossref] [PubMed]
- Sankararaman B, Gurunathan S, Arafath Natchiar M, et al. Mucocele of appendix: A rare case study and review of literature. Int J Surg Sci 2020;4:333-6. [Crossref]
- Komorowski AL, Moran Rodriguez J. Amyand's hernia. Historical perspective and current considerations. Acta Chir Belg 2009;109:563-4. [Crossref] [PubMed]
- Patoulias D, Kalogirou M, Patoulias I. Amyand's Hernia: an Up-to-Date Review of the Literature. Acta Medica (Hradec Kralove) 2017;60:131-4. [Crossref] [PubMed]
- Joda AE, Hussein N. Amyand's Hernia in a 9-Month-Old Infant: Case Report & Review of the Literature. Iraqi Postgraduate Medical Journal 2017;16:218-23.
- Solecki R, Matyja A, Milanowski W. Amyand's hernia: a report of two cases. Hernia 2003;7:50-1. [Crossref] [PubMed]
- Singal R, Mittal A, Gupta A, et al. An incarcerated appendix: report of three cases and a review of the literature. Hernia 2012;16:91-7. [Crossref] [PubMed]
- Abu-Dalu J, Urca I. Incarcerated inguinal hernia with a perforated appendix and periappendicular abscess: report of a case. Dis Colon Rectum 1972;15:464-5. [Crossref] [PubMed]
- Losanoff JE, Basson MD. Amyand hernia: a classification to improve management. Hernia 2008;12:325-6. [Crossref] [PubMed]
- Saim HA, Chik I, Jaafar FF, et al. A rare presentation of low-grade appendiceal mucinous neoplasm within an amyand's hernia: a case report. Ann Coloproctol 2023;39:183-7. [Crossref] [PubMed]
- Bhatti SI, Hashmi MU, Tariq U, et al. Amyand's Hernia: A Rare Surgical Pathology of the Appendix. Cureus 2018;10:e2827. [Crossref] [PubMed]
- Morales-Cárdenas A, Ploneda-Valencia CF, Sainz-Escárrega VH, et al. Amyand hernia: Case report and review of the literature. Ann Med Surg (Lond) 2015;4:113-5. [Crossref] [PubMed]
- Gao Y, Zhang T, Zhang M, et al. Amyand's hernia: a 10-year experience with 6 cases. BMC Surg 2021;21:315. [Crossref] [PubMed]
- Crăciun C, Mocian F, Crăciun R, et al. Perforated Appendiceal Mucocele within an Amyand's Hernia: A Case Report and a Brief Review of Literature. Chirurgia (Bucur) 2023;118:1. [Crossref] [PubMed]
- Anania G, Giaccari S, Solfrini G, et al. Appendicular mucocele: two case reports and literature review. G Chir 2015;36:276-9. [Crossref] [PubMed]
- Oremule B, Ashrafi MH. Amyand's hernia with a periappendicular abscess. BMJ Case Rep 2014;2014:bcr2013203062. [Crossref] [PubMed]
Cite this article as: Brar PS, Dhuria S, Gupta G, Goyal A, Bansal R. A rare case of Amyand’s hernia presenting as an appendicular mucocele, extending into retroperitoneum: a case report. J Vis Surg 2024;10:9.