Type C1 radical hysterectomy and anatomical reconstruction of pelvic structures to enhance pelvic floor function in early-stage cervical cancer: surgical technique
Highlight box
Surgical highlights
• Building upon the foundational principles of type C1 surgery, strengthening the support of the uterine-vaginal stump and reconstructing the vesicocervical ligament to reduce the occurrence of postoperative pelvic dysfunction.
What is conventional and what is novel/modified?
• Conventional surgical technique: type C1 consists of the resection of the uterosacral and vesicouterine ligaments at the rectum and bladder levels, respectively. The ureter is mobilised completely, and 15–20 mm of the vagina from the tumour or cervix is resected, whereas a nerve-sparing approach, remains above the deep uterine vein.
• Modifications or innovations of surgical technique: Strengthen the support of the uterine-vaginal stump and reconstruct the vesicocervical ligament.
What is the implication, and what should change now?
• Cervical cancer patients, especially young women, should undergo pelvic floor reconstruction based on C1 surgery to reduce the damage to the pelvic floor structure after surgery.
Introduction
Background
Radical hysterectomy with pelvic lymphadenectomy is the first choice for treating early cervical cancer [International Federation of Gynaecology and Obstetrics (FIGO) stage IA1–IIA2] (1). This radical surgery has severe late complications, especially bladder dysfunction, potentially lasting >1 year after surgery (2,3). Therefore, nerve-sparing radical hysterectomy (type C1) is gradually replacing traditional surgery, intending the reduction of postoperative complications.
Rationale
Some studies have confirmed that type C1 surgery is beneficial for the recovery of bladder and anorectal function and the reduction of vaginal bleeding (4-6). However, the destruction of pelvic floor structure by radical cervical cancer surgery still exists. Concerning young patients of reproductive age, there is a potential late risk of vaginal apical prolapse after paracervical tissue resection. Additionally, upper vaginal resection and ureteral separation weaken the back of the vesical triangle and lack support. In addition, it changes the ureter course, which has a late risk of complications for the long-term prognosis of young patients.
Our improved surgical techniques include type C1 radical hysterectomy and an anatomical reconstruction of pelvic structures to enhance pelvic floor function.
Objective
Through surgical modification, the stump of the uterus and vagina stump was reinforced and the vesicocervical ligament was reconstructed, enabling the contracted bladder triangle to stretch to an extent that restores the original anatomy of the ureter and bladder angle, it is also reduces the potential risk of long-term postoperative complications in young patients. Herein, we introduce an improved surgical technique to reduce the damage of female pelvic floor function and improve the prognosis of patients with early cervical cancer. We present this article in accordance with the SUPER reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-45/rc).
Preoperative preparations and requirements
The procedure requires four gynecologists (at least two chief physicians), a travelling nurse, a device nurse and an anesthesiologist. The procedure must be performed in an operating theatre with the patient lying flat on the operating bed. No special surgical equipment, supplies, drugs or software are used.
Our team has conducted and completed >2,000 cases of cervical cancer surgery (including laparotomy and minimally invasive surgery), with the lead surgeon and the first assistant cooperating with >600 cases of gynecological surgery.
All procedures performed in this study were based on the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (revised in 2013). Written informed consent was obtained from the patient (41 years old) for the publication of this manuscript and the accompanying images and video. A copy of the written consent is available for review if requested.
Step-by-step description
Here we present the type C1 radical hysterectomy with anatomical reconstruction of pelvic structures for early-stage cervical cancer with a video (Video 1).
- Based on the foundational principles of type C1 surgery, after sufficiently isolating Okabayashi space, and the space between the fascia propria rectum and the sacral ligament, suture the sacral ligament near the sacrum with non-absorbable thread and leave the thread in reserve.
- Lift the sacral ligament and excise the sacral ligament structure with an ultrasonic knife at the lateral level of the rectum.
- After processing the peripheral structures of the uterus, cut the vaginal wall 2–3 cm below the fornix and suture the vaginal stump routinely. The supporting structures at the top of the vagina (e.g., pericervical ring and sacral ligament) are completely destroyed.
- Suturing the site where the sacral ligaments at the stump of the vagina were originally attached and attaching it to the remnant part of the sacral ligament, notably, full-thickness suturing of these sites should be avoided. The opposite side should be handled the same way. After suture and traction, the uterovaginal stump was supported to a certain extent.
- With 3-0 non-absorbable thread, the remaining parts of the original vesicocervical ligament between the vagina and the bladder are carefully sutured to reconstruct the vesicocervical ligament, enabling the contracture of the bladder triangle to have partial recovery.
- The vesicocervical ligaments and vaginal stump were sutured above the lateral side of the vesical triangle to restore the original anatomy of the ureter and bladder horn.
Tips and pearls
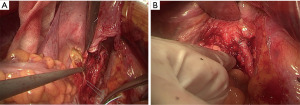
- In type C1 surgery, further vaginal contracture may occur due to lack of apex support. The operator should fully understand the anatomical structure of the sacral ligament and can clearly distinguish and retain the upper 1/3 of the sacral ligament. In this way, the operator can suture the site where the sacral ligaments at the stump of the vagina were originally attached and attaching it to the remnant part of the sacral ligament, so that the uterovaginal stump was supported to a certain extent (Figure 1A).
- The destruction of the triangular structure of the bladder can affect the function of the bladder. The operative should also fully understand the anatomical morphology of the vesical triangle and the vesical cervical ligament, so that the vesicocervical ligament can be reconstructed and the original anatomy of the ureter and bladder horn can be restored (Figure 1B).
Discussion
Surgical highlights
Based on type C1 surgery for early cervical cancer, referring to the surgical methods of prostate cancer, we strengthened the support of the top of the vagina and reconstructed the vesicocervical ligament according to the female pelvic structure.
Strengths and limitations
The anatomical structure of the pelvic cavity can be reconstructed to reduce the incidence of postoperative urinary or reproductive complications after cervical cancer surgery. For young patients, it may benefit the recovery of their urinary system and improve their quality of life after surgery. However, the increase in operation time increased the risk of surgery to some extent.
Comparison with other surgical techniques and researches
At this case in the video, the entire operation took 4 hours, approximately 0.5 hours longer, and the intraoperative bleeding was approximately 150 mL. We performed a urodynamic examination pre- and post-surgery to examine the bladder function recovery. Reportedly, the length of the vagina stump increased significantly post-surgery and postoperative recovery was not significantly different from that of the conventional surgery. The patient had no obvious special discomfort and was satisfied.
Additionally, patients and their families will be followed up with questionnaires 3 and 12 months post-surgery, including the recovery of urinary system function and sexual life. Considering the economy and living habits of patients, magnetic resonance imaging was used to examine the recovery of the pelvic floor structure 1 year post-surgery. We are continuously monitoring the related data of our patients.
Implications and actions recommended
Because younger patients are more concerned about restoring pelvic floor function (urinary system and sexual life), we recommend this way of operation more for younger patients with early cervical cancer.
Conclusions
The different surgical approaches for early-stage cervical cancer are controversial (laparotomic or minimally invasive). Although most studies have shown that there is no significant difference in the 5-year disease-free and overall survivals between different approaches (7,8), several studies show that patients with minimally invasive radical hysterectomy have a higher recurrence rate than those with laparotomy (9). Therefore, based on the age and prognostic expectation of our patient, we adopted laparotomy in this case in May 2023. So far, the patient’s recovery of the pelvic floor function after surgery has been satisfactory for urinary function recovery and sexual life. Our improved cervical cancer radical surgery, when combined with pelvic structure reconstruction, improves the prognosis and quality of life of patients with early cervical cancer.
Acknowledgments
We thank the patient and her family, who agreed to allow us to publish the video. The authors are also grateful for all colleagues working at the department. All of them attributed to taking care of this patient and performing the operation.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-45/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-45/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-23-45/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and the accompanying images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Koh WJ, Abu-Rustum NR, Bean S, et al. Cervical Cancer, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2019;17:64-84. [Crossref] [PubMed]
- Manchana T, Prasartsakulchai C, Santingamkun A. Long-term lower urinary tract dysfunction after radical hysterectomy in patients with early postoperative voiding dysfunction. Int Urogynecol J 2010;21:95-101. [Crossref] [PubMed]
- Cai L, Wu Y, Xu X, et al. Pelvic floor dysfunction in gynecologic cancer survivors. Eur J Obstet Gynecol Reprod Biol 2023;288:108-13. [Crossref] [PubMed]
- Kim HS, Kim TH, Suh DH, et al. Success Factors of Laparoscopic Nerve-sparing Radical Hysterectomy for Preserving Bladder Function in Patients with Cervical Cancer: A Protocol-Based Prospective Cohort Study. Ann Surg Oncol 2015;22:1987-95. [Crossref] [PubMed]
- Zhao D, Li B, Wang Y, et al. Clinical Outcomes in Early Cervical Cancer Patients Treated with Nerve Plane-sparing Laparoscopic Radical Hysterectomy. J Minim Invasive Gynecol 2020;27:687-96. [Crossref] [PubMed]
- Pieterse QD, Ter Kuile MM, Deruiter MC, et al. Vaginal blood flow after radical hysterectomy with and without nerve sparing. A preliminary report. Int J Gynecol Cancer 2008;18:576-83. [Crossref] [PubMed]
- Pecorino B, D'Agate MG, Scibilia G, et al. Evaluation of Surgical Outcomes of Abdominal Radical Hysterectomy and Total Laparoscopic Radical Hysterectomy for Cervical Cancer: A Retrospective Analysis of Data Collected before the LACC Trial. Int J Environ Res Public Health 2022;19:13176. [Crossref] [PubMed]
- Corrado G, Anchora LP, Bruni S, et al. Patterns of recurrence in FIGO stage IB1-IB2 cervical cancer: Comparison between minimally invasive and abdominal radical hysterectomy. Eur J Surg Oncol 2023;49:107047. [Crossref] [PubMed]
- Melamed A, Ramirez PT. Changing treatment landscape for early cervical cancer: outcomes reported with minimally invasive surgery compared with an open approach. Curr Opin Obstet Gynecol 2020;32:22-7. [Crossref] [PubMed]
Cite this article as: Huang J, Zuo X, Li M, Li D. Type C1 radical hysterectomy and anatomical reconstruction of pelvic structures to enhance pelvic floor function in early-stage cervical cancer: surgical technique. J Vis Surg 2024;10:10.