An original technique for lymph node dissection along the left recurrent laryngeal nerve after stripping the residual esophagus during video-assisted thorocoscopic surgery of esophagus
Introduction
Esophageal cancer, one of the deadliest cancers in the world, is commonly found in Asia (1). Lymph node metastasis of esophageal cancer exhibits downward, upward and skip spread characteristics (2). Esophageal squamous cell carcinoma has a predilection for frequent metastasis to the recurrent laryngeal nerve (RLN) lymph node on both sides comparing with esophageal adenocarcinoma (2), which is a vital yet difficult lymph node dissection point (3). Consequently, lymphadenectomy in the upper mediastinum is an essential component of radical esophagectomy for esophageal squamous cell carcinoma (4). However, in the left upper mediastinum, the work space for dissecting the lymph node along the left RLN is limited and advanced skills in dissection are required (5-7). To overcome this obstacle, we stripped the residual esophagus (8). As a result, we could obtain a clear operative field in the upper left mediastinum with the patient in the prone position, enabling safe and straightforward lymph node dissection along the left RLN. We would like to describe our lymph node dissection method along the left RLN in this report.
Methods
Patient selection and workup (Table 1)
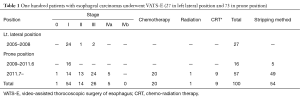
Full table
One hundred patients with esophageal carcinomas underwent video-assisted thorocoscopic surgery of esophagus (VATS-E) (27 in left lateral position and 73 in prone position). At first VATS-E in left lateral position, and then the prone position were selected for patients with superficial esophageal carcinoma from 2005. VATS-E in the prone position is indicated for all patients with resectable esophageal carcinomas with or without chemotherapy or chemoradiotherapy since 2011.
Equipment preference
Electrical devices used for VATS-E in the prone position were SonoSurg (Olympus Medical Systems, Tokyo, Japan) or LigaSure Maryland jaw sealer (Covidien, Mansfield, MA, USA). Single-port devices were ENDOPATH XCEL® Trocars (Ethicon, Cincinnati, OH, USA): three ports: 5 mm (one port long and three ports short) and one port: 12 mm (short).
Retractors: End retract mini (Covidien, Mansfield, MA, USA).
Others: 5 mm flexible laparoscope (Olympus Medical Systems, Tokyo, Japan); Endoscopic scissors and forceps.
Pre-operative preparation
General anesthesia with one lung ventilation was performed using a double lumen endotracheal tube. An epidural anesthesia tube was inserted to relieve pain in the upper abdomen. The patient was placed in a semi-prone position with a “magic bed” (or vacuum fixing bed) and a shoulder roll that was placed under the axillary.
Procedure
Position and port sites
The patient is immobilized in the semi-prone position. For an esophagectomy, the patient is rotated from the semi-prone position to the prone position. For an emergency thoracotomy, the patient is rotated from the semi-prone position to the left lateral position. Intraoperative bronchoscopy can be performed in the semi prone position.
Four ports were inserted at the 3rd, 5th, 7th and 9th intercostal spaces (ICS). One more port was added at the 7th ICS without performing a mini-thoracotomy. The chest cavity was inflated using CO2 insufflation pressure at 6 mmHg.
Intraoperative bronchoscopy can be performed with the patient in the semi-prone position, because the prone VATS-E allows for stable respiration and circulation.
Lymph nodes dissection along the lt. RLN
Stripping method to obtain the operative field of lt. upper mediastinum (Figure 1)
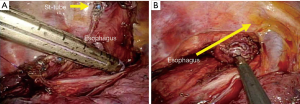
There are many advantages to the prone position, but there are also some problems, such as a narrow operative field in the upper mediastinum for lymph node dissection along the left RLN. Therefore, we considered stripping the esophagus toward the neck to remove the esophagus. The esophagus is isolated, and both the esophagus and stomach tube in the esophagus of the upper mediastinum are cut away from the tumor using iDrive™ Ultra Powered Stapling System (Covidien, Mansfield, MA, USA) or ECHELON FLEX™ Powered ENDOPATH® Stapler (Ethicon, Cincinnati, OH, USA) (Figure 1). After the stomach tube is removed through the nose, the residual esophagus is stripped in the reverse direction and retracted toward the neck. The wide operative field of left upper mediastinum is possible using this stripping technique.
Lymph nodes dissection along the lt. RLN (Figures 2,3)
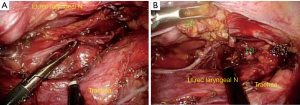

Lymph node dissection is performed after stripping the residual esophagus (10). Moreover, working space is created by compressing the right main bronchus or retracting the trachea using an Endo Mini-Retract™ 5 mm Instrument (Covidien, Mansfield, MA, USA). Lymph node and fat tissue are ablated from the left edge of the trachea, after which lymph node along the left RLN is dissected (Figures 2,3). An electrical device is used to separate the node from the nerve, and use endoscopic scissors and forceps during sharp dissection along the nerve.
Lymph nodes dissection along the rt. RLN (Figure 4)
Location of the right vagal nerve and the right inferior subclavian artery are confirmed and then the right RLN is separated from the right vagal nerve. Fat tissues, including the lymph node, are removed from the right RLN. To avoid paralysis, an electrical device is used to separate the nodes from the RLN within 2 seconds.

Role of team members
Basically, the thoracic procedures are performed by the operator in a solo surgery. But when the operator can perform incisions using an energy device under thoracoscopic vision provided by an endoscopist, greater safety can be ensured and operating time reduced if the assistant assists in providing an operative field by counter-traction during esophageal dissection. Especially during lymphadenectomy along the left RLN, the assistant can rotate or retract the trachea to ablate the lymph node and fat tissue from the left edge of the trachea while the operator uses endoscopic scissors and forceps during the sharp dissection along the left RLN.
The operator should collaborate with the assistant regarding the abdominal procedure. The operator cuts the greater and lesser omentum using an electrical device, and clips the left gastric artery and left gastro-epiploic artery with an Endo clipTM (Covidien, Mansfield, MA, USA).
The cervical procedure is performed by the operator, and the assistant expands the operative field using retractors. A left collar incision (7 cm length) is made, and the anterior cervical muscles and the sternum branch of the sternocleidomastoid muscle are divided. The cervical esophagus is then mobilized and the additional cervical lymph nodes along the left RLN are dissected. Anastomosis is performed by the operator with the assistant.
Post-operative management
The patient is placed in ICU after the operation and then extubated in the ICU on postoperative day 1. Vocalization is checked after extubation. Vocal cord evaluation and leakage check is carried out using an endoscopic examination on postoperative day 5. Food intake begins after an endoscopy and the patient is usually discharged from hospital 2–3 weeks after the operation.
Tips, tricks and pitfalls
We ablate the lymph node and fat tissue from the left edge of the trachea, after which the lymph node along the left RLN are dissected.
Fat tissue, including the left RLN and lymph node along the nerve should be separated from the upper thoracic esophagus before the upper thoracic esophagus was incised and the oral side of the esophagus stripped.
Results
This original technique of lymphadenectomy along the left RLN after stripping the residual esophagus is performed for 54 patients in the prone position VATS-E. The rate of transient RLN palsy is 17.2%, but permanent palsy is only 1.2%.
Discussion
In Japan VATS-E in left lateral position was adopted and skillful surgeons showed VATS-E is feasible for extended lymphadenectomy and reducing surgical invasiveness (12,13). However, VATS-E in left lateral position requires not only an expert operator and endoscopist but also a highly skilled first assistant.
Noshiro et al. showed the many advantage about VATS-E in prone position (14,15). The lungs are spontaneously dislocated from the operative field due to the effects of both gravity and pneumothorax without a highly skilled first assistant. An exudate accumulates in the anterior chest apart from the operative field in the prone position. The prone position provides better visualization in the subaortic arch and subcarinal and supraphrenic regions without a highly skilled first assistant. The thoracic procedures are performed by the operator in a solo surgery.
They also described prone position allows for good dissection of lymph node around the left RLN (15), but in the left upper mediastinum, the working space for dissecting the lymph nodes along the left RLN is limited and advanced skills in dissection for the operator and first assistant are required (10). Many surgeons reported about the method of lymph node dissection along the left RLN. Fujiwara et al. showed mediastinoscope assisted lymph node dissection along the RLN (8). In prone position Kang et al. and Zheng et al. dissect lymph node after suspension of the esophagus (6,7). Noshiro et al. and Oshikiri et al. performed lymphadenectomy after cutting the esophagus (5,10,15). We also dissected lymph node along the left RLN after dividing the esophagus, but our method is very easy to avoid the oral side of residual esophagus (10).
Lymph node dissection along the RLN is most important because frequent metastasis from the primary esophageal carcinoma is detected and especially difficult comparing with dissecting the other lymph node metastasis. Moreover the RLN is easily paralyzed by ablation or burn using electrical devices (16), so we use electric devices to separate the nodes from the RLN within 2 seconds timeframe for avoiding paralysis.
Conclusions
To obtain a good and wide operating field for lymph node dissection along the left RLN, only retraction or rotation of the trachea toward the right is insufficient. With our technique, the residual esophagus can easily be pulled up to the neck after sufficient ablation. In this technique, it is not necessary to retract the esophagus with more holes or to fix the esophagus. Esophageal stripping in lymph node dissection is easier and more effective than other methods.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics board of Nippon Medical School, Tama Nagayama Hospital and written informed consent was obtained from all patients.
References
- Domper Arnal MJ, Ferrández Arenas Á, Lanas Arbeloa Á. Esophageal cancer: Risk factors, screening and endoscopic treatment in Western and Eastern countries. World J Gastroenterol 2015;21:7933-43. [PubMed]
- Greenstein AJ, Pham T, Harrison VL, et al. Minimally invasive surgery for esophageal cancer. Asian J Endosc Surg 2010;3:109-14. [Crossref]
- Udagawa H, Ueno M, Shinohara H, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol 2012;106:742-7. [Crossref] [PubMed]
- Ye K, Xu JH, Sun YF, et al. Characteristics and clinical significance of lymph node metastases near the recurrent laryngeal nerve from thoracic esophageal carcinoma. Genet Mol Res 2014;13:6411-9. [Crossref] [PubMed]
- Oshikiri T, Yasuda T, Harada H, et al. A new method (the "Bascule method") for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 2015;29:2442-50. [Crossref] [PubMed]
- Kang M, Huang S, Lin J, et al. Video-assisted thoracoscopy the total mesoesophageal excision and systematic en bloc mediastinal lymph node dissection. J Vis Surg 2016;2:102. [Crossref]
- Zheng W, Zhu Y, Guo CH, et al. Esophageal suspension method in scavenging peripheral lymph nodes of the left recurrent laryngeal nerve in thoracic esophageal carcinoma through semi-prone-position thoracoscopy. J Cancer Res Ther 2014;10:985-90. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, Otsuji E. Mediastinoscope and laparoscope-assisted esophagectomy. J Vis Surg 2016;2:125. [Crossref]
- Makino H, Yoshida H, Maruyama H, et al. Lymph node dissection along the left recurrent laryngeal nerve (RLN) after esophageal stripping. Asvide 2016;3:449. Available online: http://www.asvide.com/articles/1223
- Makino H, Nomura T, Miyashita M, et al. Esophageal stripping creates a clear operative field for lymph node dissection along the left recurrent laryngeal nerve in prone video-assisted thoracoscopic surgery. J Nippon Med Sch 2011;78:199-204. [Crossref] [PubMed]
- Makino H, Yoshida H, Maruyama H, et al. Lymph node dissection along the right recurrent laryngeal nerve (RLN). Asvide 2016;3:450. Available online: http://www.asvide.com/articles/1224
- Osugi H, Takemura M, Higashino M, et al. Video-assisted thoracoscopic esophagectomy and radical lymph node dissection for esophageal cancer. A series of 75 cases. Surg Endosc 2002;16:1588-93. [Crossref] [PubMed]
- Ninomiya I, Osugi H, Fujimura T, et al. Thoracoscopic esophagectomy with extended lymph node dissection in the left lateral position: technical feasibility and oncologic outcomes. Dis Esophagus 2014;27:159-67. [Crossref] [PubMed]
- Noshiro H, Miyake S. Thoracoscopic esophagectomy using prone positioning. Ann Thorac Cardiovasc Surg 2013;19:399-408. [Crossref] [PubMed]
- Noshiro H, Iwasaki H, Kobayashi K, et al. Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc 2010;24:2965-73. [Crossref] [PubMed]
- Taniyama Y, Miyata G, Kamei T, et al. Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg 2015;20:41-6. [Crossref] [PubMed]
Cite this article as: Makino H, Yoshida H, Maruyama H, Yokoyama T, Hirakata A, Ueda J, Takada H, Matsutani T, Nomura T, Hagiwara N, Uchida E. An original technique for lymph node dissection along the left recurrent laryngeal nerve after stripping the residual esophagus during video-assisted thorocoscopic surgery of esophagus. J Vis Surg 2016;2:166.


