
Video-assisted thoracoscopic surgery as redo approach after prior open lobectomy: is it safely feasible?—challenges and pitfalls of a complex surgical technique
Highlight box
Surgical highlights
• This video article demonstrates how specific techniques, coupled with extensive experience in minimally invasive surgery, can make even re-interventions to be performed successfully via video-assisted thoracoscopic surgery (VATS).
What is conventional and what is novel/modified?
• There was a kind of ‘taboo’ regarding the feasibility of a redo VATS in a patient with a prior thoracotomy due to the presence of tenacious adhesions and scar tissue.
• There are pioneering reports showing that VATS is also feasible in this setting, with excellent results.
What is the implication, and what should change now?
• The increase in surgical experience, combined with the continuous development of technology now enables the performance of nearly all thoracic surgeries through VATS, even in the redo setting.
Introduction
Background
Segmentectomy/lobectomy still remains one of the gold standard treatments for the surgical management of non-small cell lung cancer (NSCLC) and other localized pulmonary diseases (1-3). The approach to major lung resections has evolved significantly over the past few decades, with minimally invasive surgery such as video-assisted thoracoscopic surgery (VATS) or robotic-assisted thoracic surgery (RATS) emerging as less invasive alternatives to traditional open thoracotomy (1-4).
While VATS/RATS offer advantages such as reduced postoperative pain, shorter recovery times, and improved cosmetic outcomes, their feasibility in patients with prior open surgery remains a subject of ongoing clinical investigation (5-9). A prior lung anatomical resection performed through thoracotomy presents, indeed, unique challenges due to the potential for pleuro-parenchymal adhesions, hilar fibrosis with altered anatomy, and scarring, which may complicate redo procedures and increase perioperative complication rates (5,7,8).
Rationale
Redo VATS segmentectomy/lobectomy following a prior thoracotomy still represents an underexplored area of thoracic surgery. However, advances in minimally invasive techniques and equipment, along with growing surgical experience, have made it possible to approach these complex cases with less morbidity than traditional open techniques (1,10). The feasibility of performing such a procedure depends on various factors, including the extent of previous surgical resection, the patient’s overall condition and the presence of pleural adhesions or hilar fibrosis limiting the operative field and increasing the risk of injury to critical structures such as the heart, diaphragm or large vessels (5-9,11).
Despite these challenges, some reports have suggested that with meticulous planning, preoperative imaging, and an experienced surgical team, redo VATS major lung resection is both technically feasible and associated with favorable outcomes in selected patients (5,8,9).
Objective
This paper addresses some technical considerations about the feasibility of performing a redo VATS segmentectomy/lobectomy in patients with a history of thoracotomy. By evaluating the risks, benefits and patient selection criteria, we seek to provide insights into how this approach can be safely and effectively utilized in the management of patients requiring anatomical lung resection after a prior thoracic surgery. We present this article in accordance with the SUPER reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-25-12/rc).
Preoperative preparations and requirements
Patients selection—anesthesiological considerations
The preoperative functional and instrumental investigations are the same as for the first operation and according to the international guidelines it encompasses an electrocardiogram (ECG), a complete spirometry with diffusing capacity of the lung for carbon monoxide (DLCO) evaluation and a routinely peripheral blood test. Values of predicted post-operative DLCO and forced expiratory volume in one second (FEV1) that are accepted from our anesthesiologic team are ≥60%, that are the same values used for standard preoperative assessment, in non-redo patients. In these cases, the patient is scheduled for surgery without further investigations. However, these patients often present with lower functional values due to previous lung resections, so the traditional supplementary examinations such as cardio-pulmonary stress test and ventilation/perfusion (V/Q) scintigraphy must be done. For borderline values, a risk stratification is carried out together with our anaesthesiologist and the decision on how to proceed is also based on the patient’s motivation.
Patients selection—surgical considerations
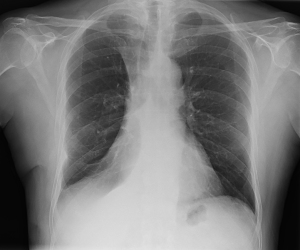
In many cases, the presence of pleuro-parenchymal adhesions or hilar scar tissue can be assessed on preoperative chest X-rays although high-resolution chest computed tomography (CT) scan remains the gold-standard technique (Figure 1). Redo surgery is by definition associated with an increased risk of intraoperative bleeding, so it is essential to carefully plan the correct timing of discontinuation of any antiplatelet/anticoagulant drugs and the request for packed red blood cells. We usually request 3 or 4 units of packed red blood cells for each of these cases. A temporary bridge to unfractionated subcutaneous heparin therapy might be discussed case-by-case to balance thrombotic and hemorrhagic risks.
In patients who underwent a previous right upper lobectomy or segmentectomy, we certainly expect a higher rate of adhesions in the hilum and in the mediastinum, that render the dissection in this delicate area more difficult, particularly in case of dissection of the main pulmonary artery. This is because in these types of resections, the hilum is deeply manipulated looking for the superior pulmonary vein and first mediastinal branch of the pulmonary artery, as opposed to middle or lower lobectomies/segmentectomies, which require fissures’ opening and a more distal manipulation of the artery.
Global preoperative assessment is fundamental in the preparation of a redo surgery, and careful pulmonary function tests, CT scan and previous pulmonary surgery evaluation is mandatory, but in our opinion the most decisive aspect is surgical expertise. The presence of a surgeon with great experience either in mini-invasive and open surgery is the most important factor for achieving a final satisfactory result.
Surgical requirements
Surgical instruments are also standard. It’s recommended to use high resolution endoscopic visualization, and it’s recommended to have open surgery instruments ready for emergency conversion. For adhesiolysis, both advanced dissection instruments such as ultrasound/radiofrequency scalpels and the Bovie can be used, while scissors-mediated dissection may be proposed by expert surgeons in case of a deep fibrous hilar consolidation. It is usually always preferred to have an epidural catheter placed in view of a possible conversion to open surgery.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki and its subsequent amendments. For this paper Ethics Committee approval was not sought because it was considered unnecessary. Written informed consent was obtained from the patient for the publication of this article, accompanying image and videos. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
Copenhagen’s triportal thoracoscopic approach is always performed in our Center (12). A 30° 10 mm 3D-optical camera is inserted through the lower access, into the same port through which, at the end of the previous procedure, the drainage was placed. With a thoracoscopic sponge-holding forceps, the surgeon carefully proceeds cranially from bottom to the top releasing all the visible adhesions to fully mobilize the lung. Adhesions are usually tenaciously and diffusely distributed alongside the chest wall, more represented at the level of the previous accesses and the areas of former dissection (Video 1). Adhesions are approached and dissected away from the lung and close to the chest wall, in order to avoid parenchymal lacerations and air losses, especially the most tenacious. This is performed to release sufficient space to open the utility port (usually 5th anterior space, 4 cm of skin incision) and the posterior access (7th or 8th space, through the scapular line, 2 cm of skin incision). Once the releasing maneuvers are completed, fissures and the hilar space are identified (Videos 1,2).
The main pulmonary artery is first identified and encircled, especially if dissection of the hilum and/or fissure is difficult due to the presence of scars. This manoeuvre allows the surgeon to approach the procedure with the confidence of having proximal control of the artery, which is particularly important in redo surgery. The maneuver is performed from the bottom upwards and in a latero-medial direction, then a surgical loop is placed around the vessel, which can be rapidly closed, if necessary, with a slack tourniquet in case of accidental vessel injury (Video 3). Securing the main pulmonary artery in the first phase of the operation and allows for the subsequent steps to proceed safely. If the presence of fibrotic tissue poses a high risk for the isolation extrapericardially, it is possible to open the pericardium to operate in a naive surgical bed, to safely perform the isolation maneuvers. As mentioned above, this option may be particularly indicated in cases where the anatomy of the pulmonary hilum has already been altered by previous surgeries on the upper lobe.
At this point, the segmentectomy/lobectomy is performed in the usual way, generally in a vein-first manner (Video 4).
At the end of surgery, two 24-Fr pleural drains are placed, one posteriorly and one anteriorly. Larger drains (28–32 Fr) can be placed if blood losses were consistent during the operation, in patients with antiplatelet therapy or preoperatory impaired blood international normalised ratio (INR) value (Video 4).
Postoperative considerations and tasks
Postoperative management of a redo case does not require any special precautions.
Postoperative management is usually carried out as a standard major lung resection despite the fact that we pay particular attention to decrease the postoperative prolonged air leaks (PALs) and postoperative bleeding as much as possible.
As concerns air leaks, to extubate the patient in the operating room in order to limit the effect of barotrauma on air leaks remains a cornerstone, especially if it is abundant after a complicated adhesiolysis. In these cases, it is advisable to maintain pleural drainage with a light suction (−8/−10 cmH2O), at least for the first postoperative day (POD), in order to minimize the damaging effect of the vacuum on the lung parenchyma. It is common to have a longer drainage time compared to resections performed in a naïve chest cavity (6). In our center, as for standard cases, pleural drain is usually removed after 24 hours in redo surgery in case of no air leaks and a fluid effusion volume lower than 500 cc per day.
In case of PALs, an autologous blood-patch (BP) with almost 200 cc of venous blood is a standard procedure in our department that is provided in 5th POD, with the possibility to be repeated further in 10th POD. Satisfying results are generally obtained after the first BP. As concerns postoperative bleedings, a routine blood count is scheduled three hours after the patient returns to the ward, in the 1 POD and in 3 POD, with the exception of any clinical or laboratory suspicion of active bleeding. In this case an urgent blood count is provided. Chest X-ray is scheduled on POD 0 and on POD 2. Other chest X-rays are planned the day after the removal of the first drain and after the removal of the second one. Postoperative respiratory and motor physical therapy starts in 1 POD with a specific plan for an early lung volume rehabilitation with a quick return to autonomous movement.
Discussion
Strengths and limitations
Redo VATS segmentectomy/lobectomy following a prior thoracotomy presents both significant strengths and notable limitations. First, the chance to perform a second surgery in the same cavity through a minimally invasive technique is a notable strength. This method reduces postoperative pain, decreases the risk of infection and accelerates the hospital discharge (1,10). VATS also offers enhanced visualization through the use of a small camera (thoracoscope), which allows for precise dissection of the lung tissue and surrounding structures (1,10,12). This can be particularly beneficial in the setting of a redo surgery, where scar tissue and adhesions from the previous thoracotomy may make the procedure technically more challenging. The magnification of the high-quality image may be an advantage (6). Furthermore, a VATS anatomical lung resection in a redo setting allows for better preservation of the chest wall that has been already injured by the previous postero-lateral thoracotomy (7,8). Traditionally, a newly thoracotomy for a second surgery can be more traumatic, especially when dealing with dense adhesions and scarring from the prior operation. VATS provides a less invasive option for resection, which may also decrease the incidence of long-term complications such as chronic neurogenic pain and post-thoracotomy syndrome (1,12). The smaller incisions used in VATS also result in better cosmetic outcomes, which can be an important consideration for patients, particularly when the prior thoracotomy incision was large or unsightly. Finally, in cases of patients which developed diabetes or peripheral vasculopathy, a smaller incision has a lower risk of wound dehiscence, which remains strictly related either to in-hospital length of stay and to postoperative infections risk (1,10,12).
However, there are several limitations to consider in a redo VATS segmentectomy/lobectomy. The most significant challenge is the presence of adhesions and distorted anatomy from the previous thoracotomy (5-9,11). These adhesions can make it more difficult to access the lung and surrounding structures, and in some cases, the conversion to an open procedure is necessary. In fact, thoracotomy remains as of today largely known by expert surgeons and routinely performed before VATS. Moreover, bleedings are generally managed more safely in an open scenario because of the small space of the utility port and the blindness induced by blood when it spreads covering the thoracoscope. These are risk factors for uncontrolled bleeding which require an emergent conversion to avoid hemorrhagic shock in the OR. However, securing the main pulmonary artery at its pericardial emergence, as described above, can be of great help in the management of massive bleeding in VATS (11). Moreover, surgeons must be prepared for potential difficulties in mobilizing the lung and performing dissection in the presence of dense scar tissue. This increases the complexity of the surgery and may lengthen the operative time (5,9).
Moreover, another limitation is the potential for compromised lung function due to the previous thoracotomy; patients who received prior lung surgery may have reduced pulmonary reserve, which could make a longer procedure riskier (13,14). Additionally, any functional limitation derived from a previous surgery, could force to perform a segmentectomy rather than a lobectomy, which certainly will be technically more complicated, particularly in a redo setting.
Additionally, the limited workspace within the thoracic cavity, especially after a previous thoracotomy, can make visualization more challenging for the surgical team, even with the use of advanced imaging technologies.
Comparison with other surgical techniques and research
The literature in recent years has also seen increasing contributions on the role of VATS for redo surgery (9). In 2020, Sun et al. demonstrated that redo VATS is feasible and safe for major lung resections by publishing a series of 14 thoracoscopic re-interventions, in which only 1 was converted to thoracotomy (7). Chen et al. compared 36 redo VATS with 28 re-thoracotomies, showing excellent results for the redo VATS group, which was characterized by fewer days of hospitalization (11.0 vs. 20.4 days) and fewer complications (16.7% vs. 39.3%) than the re-thoracotomy group (8). Fabian et al. in a case series of 41 patients undergoing redo VATS for malignancy showed good results in terms of perioperative outcomes also for those patients (6/41) with a first thoracotomy operation (5). These promising data were also confirmed in previous works from our group (6,11).
Implications and actions recommended
In light of the strengths and limitations of redo VATS lobectomy following a prior thoracotomy, several important implications and actions are recommended for clinical practice. First and foremost, patient selection is crucial. A thorough preoperative assessment, including imaging studies such as high-resolution CT scans and pulmonary function tests, is essential to evaluate the extent of adhesions, lung function, and overall tolerability. Identifying patients who may have significant comorbidities or severe pulmonary compromise can help avoid unnecessary risks, as those with poor pulmonary reserve may not be suitable candidates for a redo minimally invasive approach. For these patients, open thoracotomy may still be preferred, even if it is more invasive. On the other hand, for those with manageable scarring and good lung function, redo VATS segmentectomy/lobectomy—in properly selected patients—can offer the above-mentioned substantial benefits.
Surgeons must also be well-prepared for the challenges of redo VATS procedures, particularly the technical difficulties associated with dense adhesions and altered anatomy. Specialized training in advanced minimally invasive techniques and familiarity with anatomical variations are essential for optimal outcomes. In this regard, ongoing professional development and simulation-based training could help improve surgeon competence and confidence, reducing the risk of complications. In cases where VATS proves challenging, it is recommended that the surgical team should be prepared to convert to an open procedure if necessary. Indeed, the patient’s safety is always paramount and, especially in these cases, a conversion to open surgery, to ensure patient’s safety, should not be considered a failure of the procedure.
Furthermore, enhanced postoperative care is essential for improving outcomes. Close monitoring for complications such as PALs, wound infections and respiratory distress is crucial, particularly in redo surgeries, where these risks may be heightened. Multidisciplinary collaboration involving thoracic surgeons, anesthesiologists, respiratory therapists and nursing staff can facilitate early detection and management of any complication. Finally, long-term follow-up should include regular imaging and functional assessments to monitor for recurrence or delayed complications, as redo procedures may carry a slightly higher risk of postoperative morbidity and mortality compared to primary lobectomies.
Finally, the experience and skill of the surgical team are crucial in determining the success of a redo VATS major lung resection. Surgeons with experience in minimally invasive techniques may be able to overcome some of the technical challenges posed by adhesions and altered anatomy, but those less familiar with these procedures may face difficulties. In our centre, redo cases are usually reserved for consultants more experienced in minimally invasive surgery (more than 500 major resections), who have also gained experience with reinterventions in recent years. Consequently, the steep learning curve associated with redo VATS surgery can impact both safety and outcomes.
Conclusions
In conclusion, while redo VATS segmentectomy/lobectomy following a prior thoracotomy offers substantial advantages in terms of reduced morbidity and faster recovery, it also carries challenges related to adhesions, compromised anatomy, and patient-specific factors. The decision to pursue this approach was made on a case-by-case basis, weighing the patient’s overall performance status, challenges provided by the prior surgery and the surgeon’s expertise, which in our opinion represents the key factor for the success of the procedure. Future studies with the enrollment of larger numbers of patients for large-scale analysis of their effectiveness are required.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-25-12/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-25-12/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-25-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki and its subsequent amendments. For this paper Ethics Committee approval was not sought because it was considered unnecessary. Written informed consent was obtained from the patient for the publication of this article, accompanying image and videos. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Balderson SS, D'Amico TA. Thoracoscopic lobectomy for the management of non-small cell lung cancer. Curr Oncol Rep 2008;10:283-6. [Crossref] [PubMed]
- Nicotra S, Melan L, Pezzuto F, et al. Significance of Spread Through Air Spaces and Vascular Invasion in Early-stage Adenocarcinoma Survival: A Comprehensive Clinicopathologic Study of 427 Patients for Precision Management. Am J Surg Pathol 2024;48:605-14. [Crossref] [PubMed]
- Bonis A, Lunardi F, Pagliarini G, et al. Peripheral Circulating Blood Cells Deviation Based on Tumor Inflammatory Microenvironment Activity in Resected Upstaged Lung Adenocarcinomas. J Clin Med 2024;13:7597. [Crossref] [PubMed]
- Lim E, Harris RA, McKeon HE, et al. Impact of video-assisted thoracoscopic lobectomy versus open lobectomy for lung cancer on recovery assessed using self-reported physical function: VIOLET RCT. Health Technol Assess 2022;26:1-162. [Crossref] [PubMed]
- Fabian T, Van Backer JT, Ata A. Perioperative Outcomes of Thoracoscopic Reoperations for Clinical Recurrence of Pulmonary Malignancy. Semin Thorac Cardiovasc Surg 2021;33:230-7. [Crossref] [PubMed]
- Verzeletti V, Busetto A, Cannone G, et al. Perioperative outcomes in redo VATS for pulmonary ipsilateral malignancy: A single center experience. Eur J Surg Oncol 2023;49:107255. [Crossref] [PubMed]
- Sun W, Zhang L, Li Z, et al. Feasibility Investigation of Ipsilateral Reoperations by Thoracoscopy for Major Lung Resection. Thorac Cardiovasc Surg 2020;68:241-5. [Crossref] [PubMed]
- Chen D, Mao R, Kadeer X, et al. Video-assisted thoracic surgery is an optimal alternative to conventional thoracotomy for reoperations for ipsilateral pulmonary lesions. Thorac Cancer 2018;9:1421-8. [Crossref] [PubMed]
- Menager JB, Musso V, Issard J, et al. Feasibility of video-assisted thoracoscopic surgery as a redo chest approach for lung resection in patients with a history of surgical procedures on the same side. J Thorac Dis 2024;16:6879-87. [Crossref] [PubMed]
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Nicotra S, Verzeletti V, Cannone G, et al. Right re-redo video-assisted thoracoscopic surgery lower lobectomy with middle lobe preservation for recurrent and metachronous lung adenocarcinoma. JTCVS Tech 2023;23:120-2. [Crossref] [PubMed]
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 2011;25:1263-9. [Crossref] [PubMed]
- Lehmann M, Oehler B, Zuber J, et al. Redistribution of pulmonary ventilation after lung surgery detected with electrical impedance tomography. Acta Anaesthesiol Scand 2020;64:517-25. [Crossref] [PubMed]
- Chase CB, Mhaskar R, Fiedler C, et al. Effects of preoperative pulmonary function on perioperative outcomes after robotic-assisted pulmonary lobectomy. Am J Surg 2023;226:128-32. [Crossref] [PubMed]
Cite this article as: Nicotra S, Verzeletti V, Busetto A, Bonis A, Pellizzer E, Rebusso A, Comacchio GM, Dell’Amore A, Rea F. Video-assisted thoracoscopic surgery as redo approach after prior open lobectomy: is it safely feasible?—challenges and pitfalls of a complex surgical technique. J Vis Surg 2025;11:12.


