Is there a role for video-assisted thoracic surgery in chest wall surgery?
Video-assisted thoracic surgery (VATS) lobectomy has been used in the treatment of lung cancer since the early 1990s. This approach was both popularized and perfected by Robert McKenna and has revolutionized the field of thoracic surgery. With the evolution of thoracoscopic surgery for lung cancer and its use for increasingly complex problems and difficult situations, the indications to convert to an open operation are continually decreasing. Moreover, thoracoscopic approaches can enhance your ability to perform an operation. In this article we will discuss the role of VATS in lobectomy with en bloc chest wall resection, in first rib resection for thoracic outlet syndrome, and rib resection for bone metastasis.
In the early stages of VATS, performing a VATS lobectomy with en bloc chest wall resection would likely require conversion to open thoracotomy. However, with increasing advancement in thoracoscopic technology, this can be done using the same VATS incisions.
We make the incisions in the same locations every time. Incision 1 is approximately 2 cm long and placed in the intercostal space just below the inframammary crease. This is angled as anteriorly and inferiorly as possible to ensure that the instruments are directed towards the fissure. Incision 2 is used for the trocar and thoracoscope and placed in the eighth intercostal space in the posterior axillary line. Incision 3 is a utility incision and where the dissection is performed. This is placed at the location of the superior pulmonary vein for upper lobectomies and 1 rib space below for lower lobectomies. Incision 4 is placed in the auscultatory triangle (Figure 1) (1). A 5 mm, 30-degree angle is preferred to minimize torque on the intercostal nerves.
After the lobectomy dissection is completed and lobe of interest is completely divided from the hilum, the chest wall resection can begin. The area of planned resection is scored with electrocautery to ensure adequate margins. First we use a periosteal elevator to separate the rib from the underlying neurovascular bundle. Electrocautery and ultrasonic shear can help in locations that are difficult for the periosteal elevator to reach. We use either endoscopic bone shears or high speed drill burrs to divide the bone. These instruments are placed through the port that will provide the most perpendicular angle to the rib, which is typically in incision 1 or 4. If the rib of interest is near the utility incision, then standard bone shears can be used. Once the bone is divided, we then use ultrasonic shears to divide the chest wall tissues and intercostal bundle. After the ribs, chest wall tissues, and intercostal bundle are divided on one side, we then transect the other side. This allows the rib block to be more mobile and facilitates division of the contralateral side of the resection. The entire specimen is placed into a large specimen bag and removed from the utility incision or incision 3 (2).
If chest wall reconstruction is necessary, the VATS approach can still be utilized. We first measure a polytetrafluoroethylene (PTFE) patch to cover the defect with an onlay on the remaining rib along the resection bed. To do this, you may need to create space between the rib and chest wall tissues. Holes are pre-cut at the edges of the PTFE to tack to the chest wall. To anchor the PTFE to the chest wall, we use a device typically used to close laparoscopic port sites (Carter-Thomason Close-Sure System; CooperSurgical, Inc., Trumbull, Conn). The device can be passed twice through a small stab incision and a suture can be passed both through the PTFE and around a rib for fixation. The knot is tied extra corporeally and hidden under the skin. This is done circumferentially securing the mesh to the chest wall.
VATS approach to first rib resections for thoracic outlet syndrome provide great exposure and minimally invasive way to do chest wall surgery. First a 5 mm trocar is inserted and a 30° thoracoscope is placed in the fifth or sixth intercostal space in the midaxillary line. A second incision is made as approximately 2 cm in size over the third rib in the midaxillary line. The first rib is identified where the vessels can be seen above the first rib. We dissect the parietal pleura and intercostal muscles from the costal edge of the first rib using the Harmonic scalpel (Ethicon endo-surgery, Cincinnati, Ohio). We then bluntly dissect the surface of the ribs and then move caudally to the first rib. The first rib IS identified by feeling the flat unique orientation of the rib. The subclavian artery can be seen on superior aspect of the rib. This confirms identification the first rib visually with the thoracoscope. A periosteal elevator is used both laterally and superiorly on the first rib to separate it from surrounding tissue and muscle. During this time of the index finger was used to protect the neurovascular bundle and the brachial plexus. Removal of a 1 cm piece of the first rib in the midaxillary line allows the surgeon to push the rib caudally and complete mobilization to the sternum anteriorly and the vertebral bodies posteriorly. The rib is then cut with a rib cutter. After transection of the rib, the anterior scalene and middle scalene muscle are divided under direct visualization.
Bone metastases are classified as either osteolytic or osteoblastic (see Table 1). Osteolytic bone metastases are characterized by destruction of normal bone while osteoblastic metastases are characterized by the deposition of new bone based predominantly on radiographic appearance. Osteolytic bone metastasis (e.g., renal cell carcinoma, melanoma, etc.) can be more difficult to identify intraoperatively with the naked eye if the damage is mostly intermedullary and not affecting the periosteum. In this case when bone metastases do not protrude into the pleural space, we typically use interventional radiology guidance with wire localization to assist with identifying the metastatic lesion in the rib. We typically have IR place a wire into the lesion and it is left extending out from the skin to identify to the surgeon where to make the incision. This both ensures the correct rib is removed and the lesion is removed.
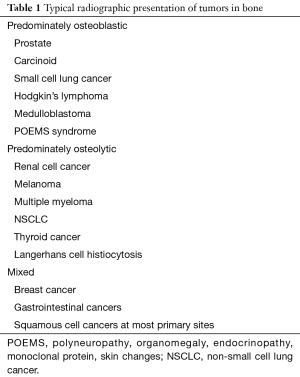
Full table
In the situation where there are osteoblastic bone metastases (e.g., prostate cancer, carcinoid, etc.) and there is protrusion into the pleural space from disruption of the periosteum, a thoracoscope can be used to localize the lesion and guide location of the incision. We typically place the incision for the thoracoscope in the anticipated location of the chest tube. Once the lesion is identified, we then plan the incision for the rib resection.
VATS has typically been used in pulmonary or intra-thoracic operations. Its use for chest wall operations is more complex and is not commonly performed. However, with the improvement in VATS instruments and technology, there is increasing indications for use VATS for chest wall surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- McKenna RJ Jr, Mahtabifard A, Swanson SJ. Atlas of Minimally Invasive Thoracic Surgery (VATS): Expert Consult. Elsevier Health Sciences, 2010.
- Demmy TL, Yendamuri S, Hennon MW, et al. Thoracoscopic maneuvers for chest wall resection and reconstruction. J Thorac Cardiovasc Surg 2012;144:S52-7. [Crossref] [PubMed]
Cite this article as: Onugha O. Is there a role for video-assisted thoracic surgery in chest wall surgery? J Vis Surg 2017;3:89.



