How to demarcate intersegmental plane with resected-segments inflation method using the slip knot technique in thoracoscopic anatomic segmentectomy
Introduction
Thoracoscopic anatomic segmentectomy is challenging because intersegmental demarcation line on the surface of the visceral pleura could not be found at thoracoscopic findings. Furthermore, in the case of pulmonary malignancies, it should be needed to gain a sufficient surgical margin from the tumor. To identify the intersegmental demarcation line is a vital point to perform thoracoscopic segmentectomy.
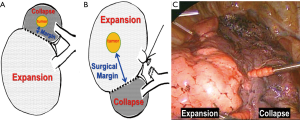
The conventional ventilation recruitment method for identifying the intersegmental plane involves inducing collapse of the resected segment and inflation of the reserved segment (1-3). The problem of this method is that the inflated segments become an obstacle to perform thoracoscopic surgery in narrow intrathoracic space. Additionally, because of the presence of three types of collateral ventilation (or collateral air drifts) taking place via the pores of Kohn, the canals of Lambert, and direct airway anastomosis (4), when the reserved segment inflation method is applied, the intersegmental plane is occasionally unclear. The resected segments inflation (RSI) method is reported to have benefits in terms of obtaining a sufficient working space and surgical margin from the tumor (Figure 1) (5,6).
RSI method
Air is sent to the objective segmental bronchus located at the center of the basic pulmonary structure. The affected segment is inflated and reserved segments are collapsed and an intersegmental plane could be identified. If this is visualized well, resection of intersegmental plane could be easily performed with the inflation-deflation line and the intersegmental pulmonary vein. The lung parenchyma that is undergoing dissection of the intersegmental plane shows changes of the color by containing the air, which serves as a landmark during dissection. This method is advantageous in that inflated segments enable identify the surgical margin from the tumor to the intersegmental plane in an air-filled condition (6).
Several methods for sending air to the resected segments have been reported. They include the jet ventilation method (7,8), and the butterfly needle method (9,10). The butterfly needle method involves the risk of an air embolism due to possible entry of air into the vein neighboring the bronchus (11,12). In this paper, we demonstrated that a new slip knot technique to make intersegmental demarcation line during segentectomy.
Slip knot technique
We have been using the RSI method to identify the intersegmental plane. In the past, bronchoscopy was used to send air to the objective bronchus. However, this technique is skillful and the inflated segments become an obstacle to perform a thoracoscopic procedure in narrow intrathoracic space. To resolve the problems, we developed the slip knot technique, and use this technique to perform thoracoscopic anatomic segmentectomy.
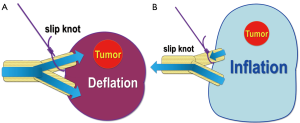
The modified Roeder knot is a method of ligation that is employed for the slip knot technique (13). A 3-0 or 4-0 polypropylene monofilament suture is passed through the segmental bronchus planned for resection, and a slip knot is formed outside the thorax. The knot is formed in the following way. A single knot is made and held by the middle finger. Wrap the end three or four times around the limbs of the loop of the suture being passed through the bronchus. The end of this suture is passed through the circle formed by the initially formed knot. The end of this suture is held and the proximal side of the knot is pulled to complete the slip knot. So that the slip knot can smoothly reach the bronchus when pulled, it is advisable to avoid excessive pulling, that is, to keep it slightly tightened.
Several types of slip knot are available, however our slip knot can be easily advanced to the bronchus just by pulling and ligate it. A characteristic of this technique is that because the knot can be advanced easily to the bronchus just by pulling, there is no excessive traction force applied to the target organ, and ligation of the bronchus is possible even if poor operative visibility. Making slip knot is presented in Figure 2.

Thoracoscopic segmentectomy using the slip knot technique
Before surgery, three-dimensional computed tomography images are established (15). The simulation images are used to identify: (I) the segmental arterial branches; (II) the intersegmental veins to be preserved; and (III) the venous branches in the affected segment to be divided. These data are used to perform the surgical procedure while comparing and contrasting the simulation with the real-time conditions in the surgical field by rotating and resizing the 3-D images.
Surgery is performed under general anesthesia and one lung ventilation. The steps for anatomic segmentectomy are as follows: firstly, the pulmonary vein and artery of the segment planned for resection are dissected from the hilum in order to isolate the segmental bronchus located behind the pulmonary artery. The veins were detached from the hilum toward the peripheral side after deciding which intersegmental pulmonary veins were to be preserved and which were to be dissected on the basis of the simulation. Then we ligated and dissected the segmental artery and detached the segmental bronchus.
Secondly, a monofilament non-absorbable suture is passed through the segmental bronchus, and a slip-knot is made outside the thorax. The suture used to form the slip knot is pulled to advance the knot, but not tightening of the bronchus. At this stage, the bronchus has not yet been ligated, and thus ventilation is possible (Figure 3A). Thirdly, bilateral lung ventilation with pure oxygen is conducted. When the affected segment has been inflated sufficiently, the slip knot suture is pulled and the segmental bronchus is ligated (Figure 3B). Then, the lung is collapsed again, the affected segment is kept inflated and collapse is induced in the segments to be reserved, allowing visualization of the inflation-deflation line. The bronchus ligated with the slip knot is dissected by stapler, suture, or ligation, depending on the caliber and nature of the bronchus (16).
In some cases, although it takes a time to get a lung collapse in the reserved segments, visualization can be completed during manipulation of the hilum. Fourthly, as inflation of the affected segment and collapse of the reserved segments could be found, resection of intersegmental plane could be easily performed with the inflation-deflation line and the intersegmental pulmonary vein.
In the resection of the lung parenchyma, we use electrocautery, an energy device, or stapler depend on the condition of emphysematous change of the lung. When dissection of about 1/3 from the hilum and the visceral pleura has been achieved along the inflation-deflation line and the intersegmental pulmonary vein serving as the landmark, respectively, a stapler is used to complete segmentectomy. The right apical (S1) segmentectomy is presented in Figure 4.

Regarding with slip knot technique, it will take 1–2 minutes (bilateral ventilation with pure oxygen) plus about 7–10 minutes (to visualize the intersegmental plane). In the case of pulmonary emphysema and the secretion of air-way, it will take a much more to obtain intersegmental plane.
Segmentectomy with the slip knot technique is applicable to the small caliber bronchi. For this reason, it is also applicable to multiple segmentectomies and segmentectomy accompanied by subsegmentectomy. Guiding the bronchoscope into the 4th or 5th generated branched bronchus is sometimes difficult, but this can be done with the use of the slip knot technique. In practice, visualization of the inter-subsegmental plane of subsegments is easier after introduction of the slip knot technique, and subsegmentectomy has been performed more frequently than it was before we adopted this technique (18).
Pure oxygen is used for inflating again with the slip knot technique. This is because inflation of lung with pure oxygen leads to a nitrogen-free state in which oxygen is absorbed in the reserved segments supplied with the pulmonary artery and collapse is easier to induce (19). Pure oxygen is inhaled for about 1–2 minutes, until the expired oxygen concentration in the respirator begins to increase.
Comments
When pulmonary segmentectomy was performed with the slip knot technique, visualization of the inflation-deflation line was possible in most cases. However depiction of the inflation-deflation line was insufficient in some cases, such as emphysema and chronic bronchitis. In the latter cases, depiction of the inflation-deflation line is difficult when air is poorly sent from the segmental bronchus planned for resection. Problems encountered in cases of emphysema include: (I) inaccurate border due to communication with the resected segments arising from peripheral lung destruction; and (II) difficulty in inducing collapse due to air trapping.
Aside from the air-sending method for visualizing the intersegmental plane, other methods are available, including a method involving injection of indocyanine green (ICG) into the segmental bronchus planned for resection (20,21) and a method in which the intersegmental line is observed under an infrared thoracoscope after intravenous injection of ICG following pulmonary artery blocking (22,23). The method involving ICG injection into the bronchus involves the risk for failure to achieve uniform dispersion of the dye in subsegments. Intravascular injection of ICG might be promising, however it involves problems of its cost and duration of visualization as it becomes invisible in a quite short time.
Segmentectomy with the slip knot technique is applicable if the segmental bronchus planned for resection can be exposed. The demarcation line does not disappear once it becomes visible. Its greatest advantage is that it does not require a jet ventilation facility or an anesthesiology unit equipped with individuals with sufficient bronchoscopy skills or bronchoscopists, allowing depiction of the intersegmental plane only by the surgeon’s manipulation within the surgical field. Use of the slip knot technique is expected to allow segmentectomy to be performed anywhere and anytime needed, with no costs required for new equipment.
Acknowledgements
The research reported in this publication was not supported by any external funding or grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Blades B. Conservation of lung tissue by partial lobectomy. Ann Surg 1943;118:353-65. [Crossref] [PubMed]
- Overholt RH, Woods FM, Betts RH. An improved method of resection of pulmonary segments: report of a technique applied in 70 operations. J Thorac Surg 1948;17:464-79. [PubMed]
- Rubenstein LH, O'Neill TJ, Glover RP. A technique for pulmonary segmental delineation. J Thorac Surg 1949;18:75-81. [PubMed]
- Spencer H, Philip SH. Spencer's pathology of the lung 5th ed. New York: McGraw-Hill; 1996:33-4.
- Tsubota N, Ayabe K, Doi O, et al. Ongoing prospective study of segmentectomy for small lung tumors. Ann Thorac Surg 1998;66:1787-90. [Crossref] [PubMed]
- Tsubota N. An improved method for distinguishing the intersegmental plane of the lung. Surg Today 2000;30:963-4. [Crossref] [PubMed]
- Matsuoka H, Nishio W, Sakamoto T, et al. Selective segmental jet injection to distinguish the intersegmental plane using jet ventilation. Jpn J Thorac Cardiovasc Surg 2003;51:400-1. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Kamiyoshihara M, Kakegawa S, Morishita Y. Convenient and improved method to distinguish the intersegmental plane in pulmonary segmentectomy using a butterfly needle. Ann Thorac Surg 2007;83:1913-4. [Crossref] [PubMed]
- Kamiyoshihara M, Kakegawa S, Ibe T, et al. Butterfly-needle video-assisted thoracoscopic segmentectomy: a retrospective review and technique in detail. Innovations (Phila) 2009;4:326-30. [Crossref] [PubMed]
- Kiribayashi M, Nakasone M, Moriyama N, et al. Multiple cerebral infarction by air embolism associated with remarkable low BIS value during lung segmentectomy with video assisted thoracic surgery (VATS) technique: a case report. Masui 2010;59:480-3. [PubMed]
- Otsuka T, Nakamura Y, Harada A, et al. Extremely rare but potential complication of diffuse brain edema due to air embolism during lung segmentectomy with selected segmental inflation technique by syringe needle during video-assisted thoracoscopic surgery. J Thorac Cardiovasc Surg 2011;142:e151-2. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. How to make the slip knot. Asvide 2016;4:328. Available online: http://www.asvide.com/articles/1640
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Management of bronchial stumps in anatomic lung segmentectomy. Ann Thorac Surg 2016;101:2120-4. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. Video-assisted thoracic surgery (VATS) right S1 (apical) segmentectomy using slip knot technique. Asvide 2016;4:329. Available online: http://www.asvide.com/articles/1641
- Kato H, Oizumi H, Inoue T, et al. Port-access thoracoscopic anatomical lung subsegmentectomy. Interact Cardiovasc Thorac Surg 2013;16:824-9. [Crossref] [PubMed]
- Iwata H, Shiraishi K, Mizuno Y, et al. Surgical technique of lung segmental resection with two intersegmental planes. Interact Cardiovasc Thorac Surg 2013;16:423-25. [Crossref] [PubMed]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. [Crossref] [PubMed]
- Oh S, Suzuki K, Miyasaka Y, et al. New technique for lung segmentectomy using indocyanine green injection. Ann Thorac Surg 2013;95:2188-90. [Crossref] [PubMed]
- Misaki N, Chang SS, Igai H, et al. New clinically applicable method for visualizing adjacent lung segments using an infrared thoracoscopy system. J Thorac Cardiovasc Surg 2010;140:752-6. [Crossref] [PubMed]
- Pardolesi A, Veronesi G, Solli P, et al. Use of indocyanine green to facilitate intersegmental plane identification during robotic anatomic segmentectomy. J Thorac Cardiovasc Surg 2014;148:737-8. [Crossref] [PubMed]
Cite this article as: Endoh M, Oizumi H, Kato H, Suzuki J, Watarai H, Hamada A, Suzuki K, Shiono S. How to demarcate intersegmental plane with resected-segments inflation method using the slip knot technique in thoracoscopic anatomic segmentectomy. J Vis Surg 2017;3:100.


