Uniportal video-assisted thoracic surgery for pneumothorax and blebs/bullae
Introduction
The last British Society of Thoracic Surgeons (BTS) guidelines of 2010 for the management of primary spontaneous pneumothorax (PSP) stated that, after the first recurrence, the treatment of PSP should be a surgical operation, like a bullectomy accompanying with a procedure for inducing pleural adhesions (1). Therefore, the surgical approach is considered the best treatment to minimise the risk of recurrence in patients who experienced a PSP. There is substantial evidence in the literature demonstrating that the minimally invasive approach should be preferred to the thoracotomic procedure since it can reduce the postoperative pain and it is associated with a faster recovery of the physical and working activity (2). The video-assisted thoracic surgery (VATS) approach has been shown to offer greater advantages about patient pain and respiratory function when compared to thoracotomic incisions. A single port or single incision or uniportal approach was developed as an alternative to the standard multi-port VATS. Uniportal technique has shown to be safe and efficient not only for pulmonary resections and biopsies but also for lobectomy. When used for PSP, the bullectomy/blebectomy and pleural abrasion/pleurectomy is performed through the single incision through which the chest drain is then inserted (3). In this perspective, evidence showed that the minimally invasive approach should be preferred, confirming the advantages in comparison with traditional techniques (4).
Here we described the theoretical aspects of the uniportal VATS approach for PSP.
Surgical technique
Uniportal VATS allows performing all the main surgical steps recommended for treating patients affected by PSP with the same clinical advantages of the traditional three-port VATS. The VATS technique achieves the exploration of the chest cavity and the lung parenchyma to find blebs/bullae, to resect the diseased areas of the lung, and to perform adequate pleurodesis procedures (e.g., mechanical parietal pleural abrasion, talc poudrage, pleurectomy, etc.) (2).
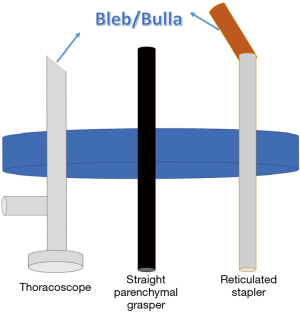
Patient decubitus is in the lateral position. Otherwise, from the standard three-port VATS approach, where the lesion represents the peak of an ideal pyramid, and the camera and instruments are placed in correspondence of the other three pinnacles, the uniportal VATS technique implies that the target, the thoracoscope, and the instruments all lie in the same sagittal plane. Although the single incision is the fulcrum where the parallel devices reach the target, arranging themselves in a craniocaudal direction (5), the surgeon should be free to move inside the chest cavity without the boundaries due to an unfavourable geometry (6). A 1.5–2 cm skin incision at the sixth intercostal space along the middle axillary line is made. We recommend the assessment of the thoracic cavity without muscular section and without rib spreading, using only a wound retractor (Alexis, Applied Medical, Rancho Santa Margarita, CA, USA), with a 30° 10 mm thoracoscope, and two parenchymal graspers. The first step, after the chest cavity exploration, is the resection of parenchymal dystrophies using an articulated stapler. The thoracoscope, the articulated stapler, and the straight parenchymal grasper could be simultaneous introduced (Figure 1). Pleurodesis is performed using several techniques: partial apical pleurectomy and pleural abrasion, electrocoagulation hook from the second through the fifth intercostal space, Vicryl mesh, talc effusion pleurodesis, etc. Finally, a single 24 Fr chest tube was introduced through the single incision under visual control. For the chest tube withdrawal there are some protocols; one, our preferred according to the current literature, is 24 hours suction at 20 mmHg suction since the end of the operation, then 24 hours without suction, and, finally, chest tube removal at postoperative day two (7).
Discussion
VATS has been developed over a period of many years and early became the surgical treatment for PSP. With advances in thoracoscopic instruments and techniques, VATS blebectomy/bullectomy remains the procedure of choice for many centres in the treatment of PSP. VATS technique has a level acceptable recurrence rate and has been shown clearly to deliver better patient satisfaction and tolerability, as well as cost implications. The most popular approach is the three port baseball diamond for VATS bullectomy and pleurodesis. The single port access enables the use of a grasping endoscopic instrument, the thoracoscope and an articulated stapler. Surgical instruments entered from different angles could create a three-dimensional working environment (8).
Subsequently, the procedure was shifted to single-port approach. Uniportal VATS technique, introduced by Marcello Migliore (9-11) was spread around the world by Gaetano Rocco (3). The uniportal VATS technique is a practical method to perform bullectomy for the treatment of PSP in association with pleural abrasion as pleurodesis with a reduction in the postoperative stay, pain and paresthesia (3). Uniportal VATS did not upsurge the risk of recurrence of PSP and allowed almost all patients to resume full working and physical activities as before the operation (2). Due to the well-known geometrical advantages, uniportal VATS allows for good exposure and adequate resection of the affected areas of the lung (12). Keys to achieving success in uniportal approach are the angled (30°) thoracoscope and roticulator staplers (9-11). With the use of these instruments, the skin incision and the compression on the intercostal nerve can be kept to a minimum (13). Many thoracic surgeons will prefer mechanical pleural abrasion or pleurectomy for benign diseases. Nevertheless, there is not any study that compares significant long-term complications of talc pleurodesis in young patients (7). Moreover, VATS permits proper pleurectomy/pleural abrasion with the diathermy scratch pad. The lower incidence of postoperative pain and paraesthesia of uniportal VATS along with current strategies like early patient mobilization are crucial steps to realize day case surgery for PSP (3). Some surgeons performed uniportal VATS without a protecting intercostal space device; nonetheless, a wound retractor should be used to protect intercostal neurovascular bundle (14).
Controversy exists in the management of first episodes of PSP. Authors suggest an immediate surgical operation by uniportal VATS in locoregional anaesthesia in the conscious patient. The absence of general anaesthesia and double-lung ventilation and the reduction of hospital costs on the other side could shift the balance in the management of PSP toward uniportal VATS. Same others suggest that this surgical procedure can even be done in an outpatient setting, minimizing the requirement for a dedicated hospital suite and beds (15).
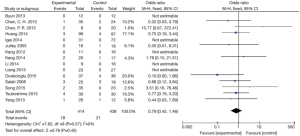
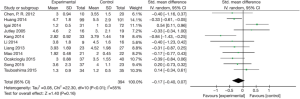
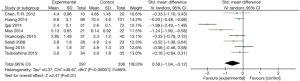
VATS is a well-known standard method in PSP because of its benefit, less postoperative pain and early recovery, compared with a thoracotomy (16). Nevertheless, authors found limitations in surgical exposure and technical feasibility of uniportal VATS, and the operation time could be longer than is necessary for three port VATS (17). Hopefully, a meta-analysis comparing uniportal with three-port VATS for PSP was recently published. Forest plots showed that the uniportal VATS approached neither increased mortality or recurrence rate (Figure 2) nor prolonged the surgical time, the length of postoperative drainage (Figure 3). Uniportal VATS showed a decreased postoperative hospital stay (Figure 4). However, uniportal VATS could reduce patients’ postoperative pain and paraesthesia, and improve patients’ satisfaction concluding that the uniportal VATS technique is a safe, feasible and effective treatment for PSP (18).
Conclusions
In patients with PSP, compared with the traditional three-port VATS, the uniportal VATS offered better results regarding the postoperative length of stay, the restore of full physical action after the operation, and the reduction of postoperative paraesthesia rate. Additionally, the uniportal VATS had surgical costs like three port VATS with lower postoperative stay costs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Salati M, Brunelli A, Xiume F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [Crossref] [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [Crossref] [PubMed]
- Salati M, Brunelli A. Uniportal VATS for pneumothorax and interstitial lung disease. J Thorac Dis 2013;5 Suppl 3:S217-20. [PubMed]
- Bertolaccini L, Viti A, Terzi A, et al. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. [Crossref] [PubMed]
- Migliore M. VATS surgery for anatomical lung resection: a different approach for every surgeon. Video-assist Thorac Surg 2016;1:31. [Crossref]
- Masmoudi H, Etienne H, Sylvestre R, et al. Three Hundred Fifty-One Patients With Pneumothorax Undergoing Uniportal (Single Port) Video-Assisted Thoracic Surgery. Ann Thorac Surg 2017;104:254-60. [Crossref] [PubMed]
- Chen CH, Lee SY, Chang H, et al. The adequacy of single-incisional thoracoscopic surgery as a first-line endoscopic approach for the management of recurrent primary spontaneous pneumothorax: a retrospective study. J Cardiothorac Surg 2012;7:99. [Crossref] [PubMed]
- Migliore M, Deodato G. A single-trocar technique for minimally invasive surgery of the chest. Surgical Endoscopy 2001;15:899-901. [Crossref] [PubMed]
- Migliore M, Giuliano R, Aziz T, et al. Four-step local anesthesia and sedation for thoracoscopic diagnosis and management of pleural diseases. Chest 2002;121:2032-5. [Crossref] [PubMed]
- Migliore M. Efficacy and safety of single-trocar technique for minimally invasive surgery of the chest in the treatment of noncomplex pleural disease. J Thorac Cardiovasc Surg 2003;126:1618-23. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Ocakcioglu I, Alpay L, Demir M, et al. Is single port enough in minimally surgery for pneumothorax? Surg Endosc 2016;30:59-64. [Crossref] [PubMed]
- Kang DK, Min HK, Jun HJ, et al. Early outcomes of single-port video-assisted thoracic surgery for primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg 2014;47:384-8. [Crossref] [PubMed]
- Rocco G, La Rocca A, Martucci N, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for spontaneous pneumothorax. J Thorac Cardiovasc Surg 2011;142:944-5. [Crossref] [PubMed]
- Jeon HW, Kim YD. Does 11.5 mm guided single port surgery has clinical advantage than multi-port thoracoscopic surgery in spontaneous pneumothorax? J Thorac Dis 2016;8:2924-30. [Crossref] [PubMed]
- Kim MS, Yang HC, Bae MK, et al. Single-Port Video-Assisted Thoracic Surgery for Secondary Spontaneous Pneumothorax: Preliminary Results. Korean J Thorac Cardiovasc Surg 2015;48:387-92. [Crossref] [PubMed]
- Qin SL, Huang JB, Yang YL, et al. Uniportal versus three-port video-assisted thoracoscopic surgery for spontaneous pneumothorax: a meta-analysis. J Thorac Dis 2015;7:2274-87. [PubMed]
Cite this article as: Bertolaccini L, Pardolesi A, Brandolini J, Solli P. Uniportal video-assisted thoracic surgery for pneumothorax and blebs/bullae. J Vis Surg 2017;3:107.


