Single-incision video-assisted thoracoscopic surgery left-lower lobe anterior segmentectomy (S8)
Introduction
Anatomical segmentectomies are lung preserving procedures that are indicated for benign lesions, lung metastasis, low-grade malignancies and even early stage adenocarcinomas of less than 2 cm without nodal involvement. Their performance needs a comprehensive knowledge of the intralobar anatomy and the potential anatomical variants, but also a careful dissection specially focused on the venous segmental drainage and the bronchial anatomy to avoid complications.
We present a left lower lobe (LLL) single-incision video-assisted thoracoscopic surgery (SI-VATS) S8 anatomical segmentectomy in a 32-year-old woman with a benign pneumocytoma.
Case presentation
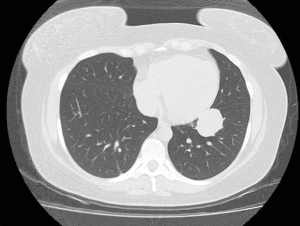
A 32-year-old woman without smoking history was incidentally diagnosed a LLL mass while consulting for several weeks of epigastralgia. A chest CT-scan showed a well-defined 3.5 cm mass in the anterior segment of the LLL, suggesting a carcinoid tumor (Figure 1). PET-CT scan evidenced pathological uptake (SUVmax 4.4) in the mass without nodal involvement, and there were no endobronchial lesions. A transthoracic core-needle biopsy was performed and reported as benign pneumocytoma. Pulmonary function tests were normal (FEV1 98%, DLCO 75%).
After initial suggestion of left-lower lobectomy due to the central location, a SI-VATS anatomical anterior segmentectomy (S8) was offered to the patient in order to preserve the majority of the lobe and the benign nature of the lesion.
Under general anesthesia, double-lumen orotracheal intubation and a 4-cm unique incision in the 5th intercostal space, intercostal block was performed at the beginning of the procedure with 0.5% Bupivacaine. First we dissected the pulmonary artery (PA) in the fissure, and identified two anterior branches for the S8 segment, so we divided them with a vascular stapler (Figure 2A). Just below the arterial stump, we dissected the bronchus. After initial dissection of both the S8 and the S9+10 segmental bronchus, we individualized the S8 bronchus and, as usual, we made an intraoperative fiberbronchoscopy for guidance and, clamping the segmental bronchus, we checked the bronchoscope light through the bronchial wall proximal to the clamp (Figure 2B). After careful identification of the segmental vein V8, we divided the fissure between S8 and S9+10 with thick load staplers. Then we checked that the segmental vein V6 and V9+10 were preserved and we divided the V8 by using a vascular stapler (Figure 2C). Last step to complete the segmentectomy requires division of the parenchyma between S8 and the surrounding segments (S6 and S9+10), and needs a thorough revision for avoiding unnoticed division of V9+10 or V6 with the parenchyma staplers. Total operating time was 140 minutes (Figure 3).

After 24 hours in the Intermediate Care Unit, chest tube was removed without air leak and normal lung reexpansion, and the patient was discharged home on the 5th postoperative day mainly due to patient’s frighten to be discharged sooner after a pulmonary resection. Visual analogue scale (VAS) scores were 3/10 and 3/10 on POD 1 and 2.
Final pathological exam showed a 3 cm sclerosant pneumocytoma without mitosis. Chest X-ray one month after the surgery showed an uneventful LLL reexpansion.
Discussion
For many years, anatomical lobectomies and more extensive procedures (bilobectomies and pneumonectomies) were the most common anatomical resections due to better oncologic outcomes for lung cancer surgery (2). Thus, for benign lesions or metastasis, wedge non-anatomical resections were first attempted as they were more simple procedures. Recent advances in the knowledge of lung cancer surgery showed that anatomical segmentectomies have its role in lung cancer treatment because of its comparable outcomes in terms of recurrence and survival, which are similar to lobectomy for early stage adenocarcinoma without nodal involvement (3,4). Asian surgeons face more often these pattern of lung adenocarcinoma with slow growth so in those countries anatomical segmentectomies have developed interestingly, improving the knowledge and comprehension about intralobar anatomy and technical aspects of sublobar procedures such as segmentectomies and subsegmentectomies (5).
Combining these lung-sparing resections with minimally invasive approaches such as uniportal conventional or subxiphoid VATS is feasible and safe (6). Some of the sublobar resections are more commonly performed worldwide such as lingulectomy, lower lobe upper segmentectomies (S6) and left upper apical trisegmentectomies, but individual upper lobe segmentectomies and even more, lower lobe segmentectomies need more experience as dissection has to be carried inside the lobe for precise division of segmental vessels and bronchus.
Lower lobe anterior segmentectomy (S8) is not common but lesions that accomplish the aforementioned criteria located in the segment can be attempted. First tip can be identifying the segmental artery, which is the most anterior division of the PA in the fissure, although sometimes there are two small divisions as in our case. Just behind the arterial stump, surgeon can dissect the lower lobe bronchus, and again the anterior division of it should be divided. It is important to highlight that B8 should not be mistaken with B8 + B9-10 bronchus, so one trick is that when the segmental bronchus is identified, an intraoperative bronchoscopy is performed to endoscopically identify the bronchus, and surgeon can even switch off the thoracoscope light so the transbronchial fiberoptic light can be visualized. One alternative consists in clamping the segmental bronchus and ventilate the lung so the preserved parenchyma can be identified and distinguished from the atelectasis of the S8. Lower vein can be dissected from below after dividing the pulmonary ligament, and V6, V9+10 and V8 must be identified. The segmental vein can be divided now, but an alternative is to divide the fissure between S8 and S9+10 before dividing the vein, running the stapler towards the division of V8 and V9+10. Finally, division of the intersegmental fissure between S8 and S6 in the fissure can be continued from the stapling line.
When indicated, anatomical segmentectomies have the advantage of preserving more lung parenchyma. In these cases, performing a S8 resection instead of a left lower lobectomy preserves three segments. These procedures can be safely performed through SI-VATS approach in experienced hands, but it is very important to carefully identify the segmental bronchi and preserve the venous drainage for the remaining segments to avoid major complications. Future work should focus in acquiring more consistent evidence for sublobar resections and define its indications, advantages and technical details.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Galvez C, Lirio F, Sesma J, et al. The technical aspects of Single-incision VATS left-lower lobe anterior segmentectomy (S8), highlighting the tricks for bronchial isolation and for preserving venous drainage for the remaining segments of the left-lower lobe. Asvide 2017;4:348. Available online: http://www.asvide.com/articles/1660
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Martin-Ucar AE, Delgado Roel M. Indication for VATS sublobar resections in early lung cancer. J Thorac Dis 2013;5 Suppl 3:S194-9. [PubMed]
- Altorki NK, Kamel MK, Narula N, et al. Anatomical segmentectomy and wedge resections are associated with comparable outcomes for patients with small cT1N0 non-small cell lung cancer. J Thorac Oncol 2016;11:1984-92. [Crossref] [PubMed]
- Yoshimoto K, Nomori H, Mori T, et al. Postoperative change in pulmonary function of the ipsilateral preserved lung after segmentectomy versus lobectomy. Eur J Cardiothorac Surg 2010;37:36-9. [Crossref] [PubMed]
- Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016;50:1060-6. [Crossref] [PubMed]
Cite this article as: Galvez C, Lirio F, Sesma J, Baschwitz B, Bolufer S. Single-incision video-assisted thoracoscopic surgery left-lower lobe anterior segmentectomy (S8). J Vis Surg 2017;3:114.


