Advantages and disadvantages of single incision VATS in major anatomical resection for lung cancer
Introduction
Different surgical approaches performed for the management of same disease may have rewards and drawbacks when they are compared to each other. These may be related to the technical features and/or surgical team’s comfort in performing the technique; yet, patient outcome measures take the priority in comparison. Any approach used in surgical oncology may become very popular for a limited period of time unless it has not been proven as safe, feasible and good for short, mid and long-term patient outcomes. Video-assisted thoracoscopic surgery (VATS) on lung resection for lung cancer was started two and a half decades ago, and for a considerably long duration, only a certain proportion of thoracic surgeons in the USA performed it. When the results of Society of Thoracic Surgeons (STS) Database in 2010 revealed that thoracotomy was an important risk factors in patients who underwent lung resection for lung cancer, the ratio of VATS approach was 36.9% (1,2). Then, surgeons shifted their operative choice from open to close in majority, and the ratio became 61.6% in the same database in 2016, 24 years after the first VATS lobectomy (3). Adapting an innovative approach into a large community takes time. Considering that the first single incision VATS (SIVATS) lobectomy was performed only 6 years ago by Gonzalez et al. (4), it is not any bad that we have a chance to discuss objectively the advantages and disadvantages of the method today.
Although ‘uniportal VATS’ is used much more commonly, there are also other descriptions used in defining the approach as single port (4) or single incision (5). As reported earlier by Migliore and co-workers, definition of the approach is yet to be clarified (6). Since lung resection is performed through the utility ‘incision’ of traditional VATS without opening the additional ‘port’ in this approach, definition of single-‘incision’ VATS was preferred over uni-‘portal’ in this article.
Technical considerations
Geometry of approaches
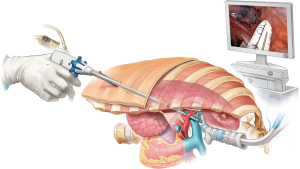
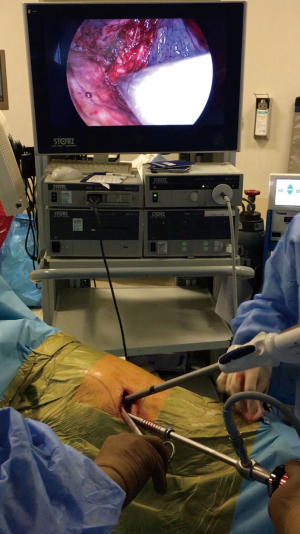
Inserting the thoracoscope and the instruments parallel to each other on the same horizontal plane makes SIVATS approach geometrically more comfortable (Figure 1). Thanks to this feature, the mental adaptation period that is needed in shifting from open surgery to multiportal VATS, where thoracoscope and other instruments approach the target area from different directions, is skipped in SIVATS. At the beginning of learning the traditional VATS everyone experiences difficulty to find the tip of the instrument on the screen. In contrast, this is not one of the concerns in learning period of SIVATS approach.
Instrument crowding
It can be thought that inserting several instruments through the same incision impedes the working of devices properly. This foresight is not totally false indeed. There are exceptional times that four different surgical instruments (i.e., thoracoscope, aspiration cannula, grasper, and a stapler) are needed at the same time inserted through the incision which is only 4 or 5 cm in length. However, in addition to the camera, the number of instruments inserted is not more than 2 in important part of operation (Figures 1,2). Difficulties have revolutionized the SIVATS surgeons to re-concur the capability of operating table in changing the position in different directions. Hence, pulling grasper is now used much less commonly once the table was turned to other side to take the lung away from the operative field. Consequently, instrument crowding which was once seen as one of the disadvantages of SIVATS is now an issue that very rarely discomfort the surgeons who perform lung resection for lung cancer thoracoscopically through a single small incision. Even so, instrument crowding can be a problem in morbid obese patients; hence, choosing the first cases of SIVATS lung resections among this group of patients could not be recommended.
Chest tube insertion site
Standardized single incision VATS lobectomy for lung cancer is performed by using fifth or fourth intercostal space in regard to the localization of the tumour (4,7-9). Rightfully, this might bring a discussion together with it whether chest tube placement through this relatively higher intercostal area weakens pleural drainage. However, no evidence has been found in the literature proving prolonged chest tube duration in the SIVATS group when compared to multiport access VATS lung resection. Meanwhile, studying the difference on residual pleural fluid collection in medium term postoperatively in SIVATS and other approaches might be a research subject.
As the preference of the author of this article, using the lower intercostal space (6th or 7th) for the incision in performing SIVATS (Figure 1) would eliminate the debate as chest tube insertion site in SIVATS might cause insufficient pleural drainage after lung resection.
Sequence of Vessel Interruption
In SIVATS lung resection for lung cancer through lower intercostal space (6th or 7th), the order of vessel stapling is the vein-first for all types of resections. However, dividing the upper lobe truncus anterior artery first in order to facilitate division of the upper lobe vein in upper lobectomies through the 4th or 5th intercostal space approach (7) may be criticized as an ‘contrast to surgical oncological principles’. Is this a rightful assumption? Indeed, the notion that manoeuvrings on the lung during resection for lung cancer may cause flaking of tumour cells into the blood stream sounds right, no clinical evidence has proven it by clinical data that it is associated with increased recurrence or shorter survival. Kurusu and associates examined whether vessel ligation sequence affects the presence of circulating cancer cells as reflected by carcinoembryonic antigen messenger ribonucleic acid (10). They assayed for the transcripts in peripheral blood taken before, during, and after operation from 36 patients with non-small-cell lung cancer who underwent a curative lobectomy. Conversion of initially negative sample to positive during the operation was more common with arterial ligation-first (85.7%) than with venous ligation-first (42.9%). However, no clinical outcome measures were reported. In contrast, two other studies reported by Rafaely and co-workers (11) and Li and co-workers (12) analysing the long-term results in comparative manner of artery-first or vein-first division of the vessels yielded no difference in recurrence or survival in patients who underwent resection for lung cancer.
Perioperative outcomes
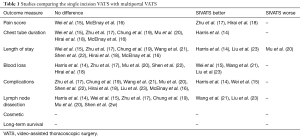
A comprehensive article reported by Sihoe in 2016 documented the comparative data of SIVATS and multi-port VATS in regard to the outcome measures in detail (13). Then, first two meta-analyses of uniportal versus multi-portal video-assisted thoracoscopic lobectomy for lung cancer reported by Harris and his co-workers in 2016 (14), and Wei and co-workers in 2017 (15) demonstrated favourable outcomes for uniportal VATS lobectomy in some of the parameters in the treatment of lung cancer when compared to the conventional multiportal approach. Conversion rate was yielded higher in SIVATS group in one of the meta-analyses (15).
Clearly, there has been no evidence proving patient safety is put at risk by SIVATS lung resection for lung cancer. In contrast, both of the meta-analyses confirmed decreased overall postoperative morbidity in SIVATS group when compared to multi-port VATS (14,15). Almost all the parameters like complications, pain, chest tube duration, length of stay (LOS) or blood loss compared between traditional VATS and SIVATS, were found similar or the SIVATS was associated with more favourable outcome in some measures observed (Table 1).
Full table
It is important to note, however, that 7 out of 8 comparative studies were performed in the centres in Asian countries like China (17,19-22), Japan (18), and Taiwan (23). There is only 1 study performed in the UK, outside of Continental Asia (16). The possibility of observing different results in different patient populations due to ethno-racial dissimilarities can mandate interpretation of these data with caution.
Pain score
Hypothetically, fewer numbers of incisions with lesser trauma to the intercostal space should be linked to the favourable pain score in the early postoperative period. Pain is not only one outcome measure of ‘postoperative comfort’. Even a minor decrease in the pain level can be critically important in patients with compromised pulmonary functions in avoiding atelectasis, pneumonia and arrhythmia.
Evidences are limited to show that SIVATS is associated with less pain score after surgery. Pain evaluation was made in three of eight papers comparing the SIVATS with traditional VATS, and two of them showed lesser pain score (17,18) in SIVATS and one showed no difference (16). Nonetheless, all the surgeons escape to increase the number of incision to avoid unnecessary injury to the intercostal nerve caused by the trocar or instrument insertion unless it is not compulsory. SIVATS has that advantageous feature already in its definition.
LOS in the hospital
In many aspects, LOS is an important parameter in evaluating the feasibility of a surgical method. Only one study in literature has shown a longer LOS in SIVATS in lung cancer resection (20) while 6 studies and one meta-analysis showed no difference (15-19,21,22). One meta-analysis, confirmed that chest tube was removed significantly earlier in SIVATS group when compared to multi-port approach (4.5±2.2 vs. 5.3±2.9 days), and patients undergoing lung resection for lung cancer by SIVATS stayed in the hospital significantly shorter (6.2±2.6 vs. 6.7±3.4 days) (14).
Cosmetic
Cosmetic results showed favourable outcome measure in SIVATS when compared to 3-port VATS for pneumothorax (24). Though, there has been no report comparing the cosmetic outcomes after lung resection for lung cancer by SIVATS or other minimal invasive approaches. Naturally, fewer numbers of incisions is expected to be associated with favourable cosmetic appearance. In addition to other advantages and disadvantages of one procedure it is not difficult to assume that cosmetic outcome could also be another factor for a patient and a surgeon in deciding which approach to be chosen. STS Database shows that the ratio of female patients is 55% among the patients who underwent lung resection for lung cancer between 2012 and 2014 in the USA (3). In an era with a trend toward to surgery performed in earlier stages aesthetic concern is not the one that to be ignored easily.
Perioperative blood loss
Considering that the SIVATS lung resections are performed generally by experienced surgeons, increased amount of blood loss in SIVATS may not be expected. Four of the six comparative studies (17,18,20,22) and one of the meta-analyses (14) showed no difference between SIVATS and multi-port lung resections for lung cancer while two studies (21,23) and one meta-analysis (15) confirmed lesser blood loss in SIVATS group than multi-port VATS group.
Oncological considerations
One of the most prominent discussions against SIVATS lung resection for lung cancer is that the approach has a limited ability to dissect the mediastinal lymph nodes in some stations (i.e., subcarinal area). Most, if not all, of the surgeons who perform SIVATS lung resections are mastered VATS surgeons who shifted their approach from multi-port to single incision in time. An experienced SIVATS surgeon has no difficulty to dissect any lymph node station, however, the feasibility of dissection remains to be documented with evidences. There has been no comparative study reporting lower yield of lymph node dissected in SIVATS lung resections. Yet, four of the six studies revealed no difference (17,19,20,22) and two studies reported higher yield of lymph node dissected in SIVATS (21,23) in comparison with standard VATS approach. The meta-analyses showed that variations of VATS approaches have no superiority to each other in this manner (14,15).
Long-term oncological consequence is the critical step for any innovative approach to be able to grow to its adulthood phase. It can be remembered that proving itself as not below, but above, to open surgery in oncological outcomes based on the evidences of meta-analyses took quite a long time for the standard VATS lung resections in lung cancer. Still, in this pre-pubertal period of SIVATS, mid and long-term oncological results wait for being completed and reported. There is no background information that could prove proclaim like “decrease the number of incision may increase survival”. Although, the contradiction has also no evidence, large series are still mandatory to prove that SIVATS is not inferior to other approaches in regard to patient survival. Proactive criticisms about the lacking of long-term oncological outcome measures of SIVATS lung resections in lung cancer have an important contribution in this regard in accelerating the studies to be published.
Conclusions
Altough, in addition to its definitive features of favourable geometrical application and more cosmetic outcome, SIVATS as one of the least invasive approach in lung resections for lung cancer has been proven by studies to have advantage over multi-port VATS in regard to chest tube duration, LOS and overall morbidity in this period of thoracic surgical evolution, there has been limited evidence proving the superiority of SIVATS over multiport VATS. It has not been shown in large comparative reports that SIVATS had disadvantage in any perioperative outcome measure and lymph node dissection in lung resection for lung malignancies. Long-term oncological results, the most important step that will shape its future practices in lung cancer, however, is yet to be reported.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Kozower BD, Sheng S, O’Brien SM, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg 2010;90:875-81. [Crossref] [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [Crossref] [PubMed]
- Fernandez FG, Kosinski AS, Burfeind W, et al. The Society of Thoracic Surgeons Lung Cancer Resection Risk Model: Higher Quality Data and Superior Outcomes. Ann Thorac Surg 2016;102:370-7. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. [Crossref] [PubMed]
- Migliore M, Halezeroglu S, Molins L, et al. Uniportal video-assisted thoracic surgery or single-incision video-assisted thoracic surgery for lung resection: clarifying definitions. Future Oncol 2016;12:5-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic lobectomy. J Thorac Dis 2013;5:S234-45. [PubMed]
- Sihoe ADL. Uniportal video-assisted thoracic (VATS) lobectomy. Ann Cardiothorac Surg 2016;5:133-44. [Crossref] [PubMed]
- Wang GS, Wang Z, Wang J, et al. Uniportal complete video-assisted thoracoscopic lobectomy with systematic lymphadenectomy. J Thorac Dis 2014;6:1011-6. [PubMed]
- Kurusu Y, Yamashita J, Hayashi N, et al. The sequence of vessel interruption affects tumor release into the circulation. J Thorac Cardiovasc Surg 1998;116:107-13. [Crossref] [PubMed]
- Refaely Y, Sadetzki S, Chetrit A, et al. The sequence of vessel interruption during lobectomy for non-small cell lung cancer: is it indeed important? J Thorac Cardiovasc Surg 2003;125:1313-20. [Crossref] [PubMed]
- Li F, Jiang G, Chen Y, et al. Curative Effects of Different Sequences of Vessel Interruption During the Completely Thoracoscopic Lobectomy on Early Stage Non-Small Cell Lung Cancer. Ann Thorac Cardiovasc Surg 2015;21:536-43. [Crossref] [PubMed]
- Sihoe AD. Reasons not to perform uniportal VATS lobectomy. J Thorac Dis 2016;8:S333-43. [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Wei S, Chen N, Liu C, et al. Does single-port video-assisted thoracic lobectomy have favorable perioperative results for non-small cell lung cancer compared with multi-port approach? A systematic review and meta-analysis. Video-assist Thorac Surg 2017;2:33. [Crossref]
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-41. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [Crossref] [PubMed]
- Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. [Crossref] [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [Crossref] [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-53. [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-72. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
Cite this article as: Halezeroğlu S. Advantages and disadvantages of single incision VATS in major anatomical resection for lung cancer. J Vis Surg 2017;3:115.