Single-port video-assisted thoracoscopic surgery (VATS) right pneumonectomy: a case report
Introduction
Modern principles of surgical treatment of NSCLC dictate that every possible effort has to be made to avoid pneumonectomy, its debilitating consequences and a higher rate of complications (1). In marginal cases where VATS sleeve or double sleeve lobectomy cannot be performed a conversion to open sleeve lobectomy is always preferred over a VATS pneumonectomy (1-3). Since indications for a VATS pneumonectomy are very limited, only a few reports of single-port VATS pneumonectomy exist (4,5).
Case presentation
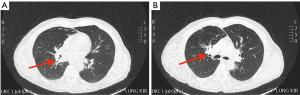
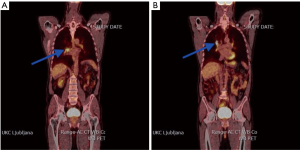
We present a case of a 64-year-old male patient with the history of persistent cough and sweating. Chest computed tomography revealed two centrally located endobronchial masses in the upper and lower lobe of the right lung with enlarged mediastinal lymph nodes on the ipsilateral side (Figure 1). Positron emission tomography/computed tomography revealed metastases in the hilar nodes on the ipsilateral side—N1 disease. Subsequently flexible bronchoscopy with transbronchial needle aspiration of the hilar nodes showed no sign of metastases—N0 disease (Figure 2).
A 5 cm single incision was made in the right 5th intercostal space in the anterior axillary line and an Alexis type wound protector was placed to provide maximal exposure.
The lung was retracted posteriorly and caudally to obtain a good visualization of the hilar structures and azygos vein. Initially the anterior mediastinal pleura of the hilum was dissected using a harmonic scalpel.
As the first step, the truncus anterior of the right pulmonary artery (PA) was carefully dissected, freed from the pericardium and then ligated and divided with an endoscopic stapler. Posteriorly to it, right main stem bronchus was visualized. Having gained more space to maneuver, the bronchus was dissected and divided with an endoscopic stapler. Due to the angle provided by the approach through the newly created incision, we have stapled the bronchus in the medial to lateral direction. Thereafter we proceeded with the dissection and exposure of the right PA, access to which has been facilitated following the division of truncus anterior of the right PA and the right main stem bronchus. Having completed the vital part of the procedure, the lung was repositioned and retracted posteriorly and cranially. Both right inferior and superior pulmonary veins were dissected, freed from the surrounding structures and divided with an endoscopic stapler. The lung was extracted using an endobag.
Finally, azygos vein was dissected from the posterior wall between the point where the right superior intercostal vein drains into it and where it drains into the superior vena cava. A paratracheal lymph node superiorly to it was excised from the fatty tissue. Two 2/0 braided nylon sutures were used to pull the azygos vein over the bronchial stump to cover and reinforce it.
A 20 Fr chest tube was inserted through a separate incision in the 8th intercostal space in the posterior axillary line. Total duration of the procedure (skin to skin) was 102 minutes.
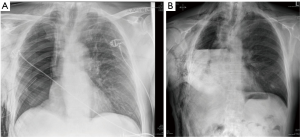
Postoperative recovery was satisfactory, with subcutaneous emphysema appearing on the postoperative day (POD) 1. Chest tube was removed on the POD 2. A chest radiograph was performed on the POD 5 and it showed a slowly diminishing subcutaneous emphysema and a pleural effusion up to the level of the 3rd rib anteriorly (Figure 3). The patient was discharged on the same day. Pathology report revealed both tumors to be squamous cell carcinoma (Figure 4).

Discussion
The indications for single-port VATS pneumonectomy are limited. The procedure should be reserved for centrally located tumors, synchronous tumors in the same lung or smaller tumors involving central structures (7). When possible, a sleeve lobectomy should be performed (8). In the reported case the mentioned criteria have been met. The location of malignant lesions was found to be central, in the same lung and with endobronchial invasion. Sleeve lobectomy was not a feasible option.
The main difficulty to a single-port VATS resection presented the anatomy of the right PA and its relationship to the right main stem bronchus. To obtain an optimal angle for thoracoscopic resection, we approached the hilum through an incision in the 5th intercostal space in the anterior axillary line. This provided a direct visualization of the right PA after the dissection of the mediastinal pleura. Due to its very proximal origin, the anterior truncus of the right PA was dissected first, then ligated and divided with an endoscopic stapler. The right main stem bronchus was located posterio-cranially to the right PA, therefore we decided to dissect and divide it first and then, after gaining more room to maneuver, we proceeded with the dissection and division of the right PA. Due to the thoracoscopic angle, the conventional method of cartilage to membranous portion stapling could not be performed, instead we have stapled the bronchus by compressing it in the medial to lateral direction, which could pose a problem and arguably increase the chances of bronchopleural fistula (BPF) occurrence as opposed to the conventional method of cartilage to membranous portion folding (9). To minimize the chances of the latter, azygos vein flap was pulled and sutured over the bronchial stump (10).
Chest tube was inserted through another incision in the 8th intercostal space to obtain a better position for chest drainage.
Conclusions
Single-port VATS pneumonectomy can be a safe and feasible procedure when performed by an experienced surgeon in a centre with previous VATS experience. However, when possible, VATS sleeve or double sleeve lobectomy or even conversion to open sleeve lobectomy should be performed instead of VATS pneumonectomy in order to avoid its debilitating consequences and a higher rate of complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ludwig C, Stoelben E, Olschewski M, et al. Comparison of morbidity, 30-day mortality, and long-term survival after pneumonectomy and sleeve lobectomy for non-small cell lung carcinoma. Ann Thorac Surg 2005;79:968-73. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Annals of Cardiothoracic Surgery 2014;3:E2. [PubMed]
- Stallard J, Loberg A, Dunning J, et al. Is a sleeve lobectomy significantly better than a pneumonectomy? Interact Cardiovasc Thorac Surg 2010;11:660-6. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Video: Single-incision video-assisted thoracoscopic right pneumonectomy. Surg Endosc 2012;26:2078-9. [Crossref] [PubMed]
- Domjan M, Mavko A, Štupnik T. Single-port video-assisted thoracoscopic surgery (VATS) right pneumonectomy. Asvide 2017;4:400. Available online: http://www.asvide.com/articles/1714
- Conlan AA, Sandor A. Total thoracoscopic pneumonectomy: indications and technical considerations. J Thorac Cardiovasc Surg 2003;126:2083-5. [Crossref] [PubMed]
- Berthet JP, Paradela M, Jimenez MJ, et al. Extended sleeve lobectomy: one more step toward avoiding pneumonectomy in centrally located lung cancer. Ann Thorac Surg 2013;96:1988-97. [Crossref] [PubMed]
- Aoki T, Ozeki Y, Watanabe M, et al. Cartilage folding method for main bronchial stapling. Ann Thorac Surg 1998;65:1800-1. [Crossref] [PubMed]
- Al-Mufarrej F, Margolis M, Strother E, et al. Bronchial stump reinforcement with an azygous vein flap. J Cardiothorac Surg 2009;4:22. [Crossref] [PubMed]
Cite this article as: Domjan M, Mavko A, Štupnik T. Single-port video-assisted thoracoscopic surgery (VATS) right pneumonectomy: a case report. J Vis Surg 2017;3:130.