Uniportal subxiphoid video-assisted thoracoscopic approach for thymectomy: a case series
Introduction
Minimally invasive thoracic surgery has evolved significantly over recent years. Since the introduction and widespread acceptance of video-assisted thoracoscopic surgery (VATS) there have been attempts to further evolve the technique for example, reducing the number of incisions with uniportal VATS, and even utilisation of robotic assistance. The overall aim is to perform a safe and complete operation but with minimal post-operative pain and as short an in-patient admission as possible.
In the case of thymectomy, we have witnessed the evolution from the traditional median sternotomy approach to VATS which is now the preferred surgical option (1,2). Median sternotomy is now reserved for patients in whom complete resection is not thought possible via the VATS approach or due to intra-operative complications. The challenge with VATS thymectomy though is achieving satisfactory visualization of the entire thymus which has bilateral extension, through a unilateral approach.
Currently, a further evolution of VATS surgery is being developed—the subxiphoid-VATS approach (3). In this technique, a single vertical muscle-sparing incision is made in the subxiphoid space permitting thoracic surgery to be performed without requiring intercostal incisions.
Here we present a case series of subxiphoid-VATS thymectomies describing intra and post-operative characteristics that demonstrate the safety and feasibility of this novel surgical approach.
Methods
All procedures were performed in Shanghai Pulmonary Hospital, Shanghai, China, between October 2014 and January 2017.
Exclusion criteria for subxiphoid-VATS thymectomy included:
- thymic tumour, stage II–IV (macroscopic spread to surrounding fatty tissue or beyond, including distal metastases);
- body mass index >30;
- cardiomegaly, poor cardiac function or severe arrhythmia (because of reduced operative access to left-side of thymus and risk of cardiovascular compromise).
Surgical technique
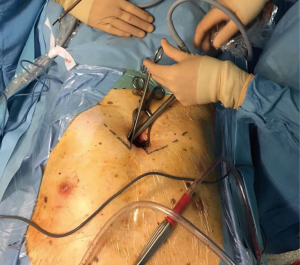
Under general anaesthesia, patients were placed in a supine position with a roll beneath the scapulae (for maximal chest extension). Selective one lung ventilation was used during the procedure. A 4-cm-long horizontal subxiphoid incision was made if the infrasternal angle was within normal limits (¡Ý70°). Alternatively, if the infrasternal angle was less than 70°, a longitudinal incision was made. The xiphoid process was then resected to provide a widened operative view. In these cases, the sternum was not elevated. Blunt finger dissection created a retrosternal tunnel between the incision and the thoracic cavity and a wound protector was placed to further optimize the view. Any obstructing anterior mediastinal adipose tissue was removed. A 10 mm 30o angle thoracoscope (Karl Storz, Tuttlingen, Germany) was used in each case (Figure 1).
The right pleural cavity was opened initially, with the left lung being selectively ventilated. Electrocautery dissection of pericardial and epiphrenic fat pads was performed and then the right lobe of the thymus was identified and dissected from the pericardium and ascending aorta. Care was taken to visualize fully the innominate vein and superior vena cava junction prior to dissection of the thymic horn from the underlying innominate vein. The thymic veins (of which there are usually 2–4) were identified prior to draining into the innominate vein and ligated using a LigaSure device.
The left pleural cavity was then opened with the right lung selectively ventilated. The left pericardial and aortopulmonary window adipose tissue was dissected prior to completing dissection of the left thymic horn. The freed thymus and any attached mediastinal fat was then removed via the subxiphoid incision (Figure 2).
A 28 Ch chest drain was placed in each pleural cavity and the subxiphoid incision closed around the drains (Figure 3). The majority of patients were extubated immediately post-operatively.
Data collection
Data was retrieved from a prospectively maintained database with additional data retrieved retrospectively from patient notes and electronic patient records. Data concerning patient demographics, intraoperative details and post-operative course were collected.
Results
Patient characteristics
Over the period of study, seventeen subxiphoid-VATS thymectomies were performed for thymic lesions. The mean age of patients was 55 years. Patient characteristics are summarised in Table 1. None of the patients had a background of myasthenia gravis preoperatively.
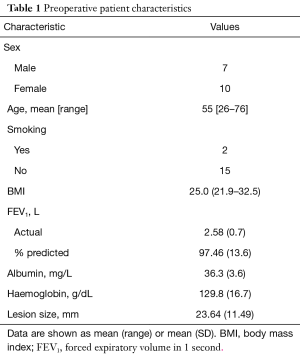
Full table
Intraoperative details
Intraoperative details are summarised in Table 2. The mean length of surgery was 2.5 hours with a range 1.5–5 hours. There was one conversion to thoracotomy because of injury to the innominate vein. There was minimal intra-operative blood loss with a mean loss 115 mL.
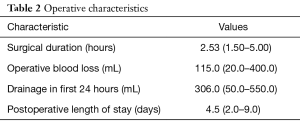
Full table
Postoperative course
One patient experienced a myasthenic crisis following surgery requiring temporary respiratory support and was discharged on day 9 post-operatively. The median length of hospital stay was 4 days. There were no instances of phrenic nerve palsy. There was no 30-day mortality in this patient series.
Post-operative pathological examination of the resected thymic lesions is summarised in Table 3. Thymic cysts were the commonest pathology observed.
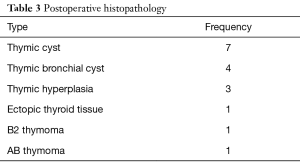
Full table
Discussion
This case series demonstrates the subxiphoid-VATS approach to be a safe and feasible approach to performing extended thymectomy in selected patients.
The VATS approach to thymectomy has been demonstrated to have several advantages compared to the traditional median sternotomy approach, without compromising the oncological outcome, including reduced intraoperative blood loss, earlier removal of chest drains, reduced requirement for blood products, reduced inflammatory cytokine response, shorter hospital stay and superior cosmesis (4,5)
The subxiphoid-VATS approach represents a further development of minimally invasive thoracic surgery which has been more recently described for a number of cardiothoracic procedures including pericardial window creation, coronary artery surgery, ablative sympathectomy, pulmonary wedge resection and even lobectomy (6-10). The potential benefits of this approach include reduced postoperative pain and the absence of chest wall paraesthesia due to preservation of the intercostal innervation and the absence of chest drains impinging on the intercostal neurovascular bundles. The main limitation of the technique is reduced instrument manoeuvrability; however, this can be overcome with specially modified instruments and an angled thoracoscope (11).
This technique is particularly suited to thymectomy as it provides excellent views of the anterior mediastinum as well as of the two pleural spaces including the phrenic nerves. This access and view provides the surgeon the opportunity to perform an oncologically radical and safe resection of the thymus with low risk of injuring the phrenic nerve or other intrathoracic structures.
To date there are only isolated case reports describing the uniportal subxiphoid-VATS technique for thymectomy (12,13). This case series adds further to the evidence that the subxiphoid-VATS uniportal approach is a safe and appropriate method for thymic resection in a selected patient group, i.e., non-obese patients with Masaoka stage 1 tumours and without significant underlying cardiorespiratory disease. We would not advocate this procedure in patients with poor respiratory function who are unable to tolerate single lung ventilation, nor in patients with significant cardiomegaly, cardiac failure or severe arrhythmia who would be likely to have poor operative access and experience cardiovascular destabilisation as a result of instrumentation of the left-hemi thorax via a subxiphoid incision.
Conclusions
The uniportal subxiphoid-VATS technique is a safe and feasible approach to performing extended thymectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Shanghai Pulmonary Hospital Ethical committee and informed consent was obtained from all patients.
References
- Tomaszek S, Wigle DA, Keshavjee S, et al. Thymomas: review of current clinical practice. Ann Thorac Surg 2009;87:1973-80. [Crossref] [PubMed]
- Regnard JF, Magdeleinat P, Dromer C, et al. Prognostic factors and long-term results after thymoma resection: a series of 307 patients. J Thorac Cardiovasc Surg 1996;112:376-84. [Crossref] [PubMed]
- Yano M, Moriyama S, Haneda H, et al. The subxiphoid approach leads to less invasive thoracoscopic thymectomy than the lateral approach. World J Surg 2017;41:763-70. [Crossref] [PubMed]
- Reddy R. The advantages of VATS: a systematic review. Thorax 2005;60:238. [Crossref]
- Raza A, Woo E. Video-assisted thoracoscopic surgery versus sternotomy in thymectomy for thymoma and myasthenia gravis. Ann Cardiothorac Surg 2016;5:33-7. [PubMed]
- Aresu G, Jiang L, Bertolaccini L. Subxiphoid video-assisted major lung resections: the Believers’speech. J Thorac Dis 2017;9:E387-9. [Crossref] [PubMed]
- Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016;50:1060-6. [Crossref] [PubMed]
- Hernandez-Arenas LA, Guido W, Jiang L. Learning curve and subxiphoid lung resections most common technical issues. J Vis Surg 2016;2:117. [Crossref]
- Aresu G, Wu L, Lin L, et al. The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies. J Vis Surg 2016;2:135. [Crossref] [PubMed]
- Aresu G, Weaver H, Wu L, et al. The Shanghai Pulmonary Hospital uniportal subxiphoid approach for lung segmentectomies. J Vis Surg 2016;2:172. [Crossref] [PubMed]
- Wu L, Lin L, Liu M, et al. Subxiphoid uniportal thoracoscopic extended thymectomy. J Thorac Dis 2015;7:1658-60. [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Karunanantham J, Fok M, Ali JM, et al. Subxiphoid SILS approach for thymectomy: a case report. J Vis Surg 2017. [Epub ahead of print]. [Crossref]
Cite this article as: Weaver H, Ali JM, Jiang L, Yang C, Wu L, Jiang G, Aresu G. Uniportal subxiphoid video-assisted thoracoscopic approach for thymectomy: a case series. J Vis Surg 2017;3:169.