Video assisted right mini-thoracotomy for aortic valve replacement
Introduction
Minimally invasive aortic valve replacement (mini-AVR) refers to an aortic valve replacement that is not performed through a traditional median sternotomy. The predominant surgical approaches for mini-AVR are upper hemi-sternotomy and right anterior mini-thoracotomy (RAM) (1). Mini-AVR has been associated with a decrease in blood transfusions, hospital and intensive care unit length of stay, ventilation time, and improved cosmesis when compared to conventional sternotomy (1-6). Furthermore, mini-AVR performed through a mini-thoracotomy approach potentially has improved outcomes compared to those performed through a hemi-sternotomy (7). Despite its potential advantages, this technique has not been widely adopted due to technical challenges, which include visualization and difficulty placing the annular sutures (8,9). In this report we describe in step-by-step fashion our surgical approach for isolated aortic valve replacement through a RAM.
Patient selection and workup
All patients are considered for RAM-AVR with the exception of patients with porcelain aorta. Severe atherosclerosis of the aorta is a relative contraindication. This approach can be done as a redo operation in experienced hands. Patients with endocarditis may be a contraindication for this approach. Patients must not have an absolute contraindication to transesophageal echo (TEE), but those with relative contraindications to TEE based on the American Society of Echocardiography guidelines are considered on a case by case basis (10).
Pre-operative preparation
We obtain an electrocardiogram, echocardiogram, cardiac catheterization, and pulmonary function testing. We do not routinely obtain a computed tomography scan unless there is concern for aortic root or ascending aorta pathology.
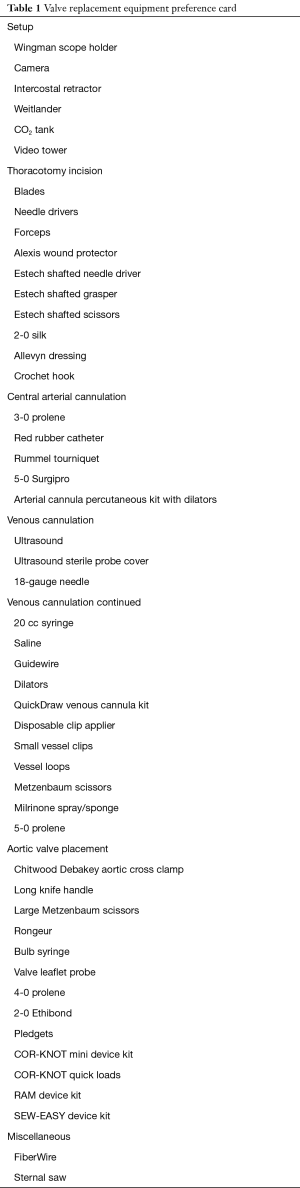
Equipment preference card
The equipment for the operating room setup and the surgical tools and instruments typically used in a RAM-AVR are listed in Table 1.
Full table
Procedure
The patient is intubated using a single lumen endotracheal tube. Systemic and pulmonary arterial catheters are placed for hemodynamic monitoring. TEE examination is initiated. The patient is prepped from above the clavicles to the knees bilaterally. We make a 5 cm incision in the second intercostal space 1 cm lateral to the sternal border (Figure 1). The pectoralis muscle is then spread to expose the intercostal muscles. The right pleural space is entered lateral to the right internal thoracic artery (RITA). The RITA is then ligated with ties and clips. A laparotomy pad is placed in the chest to compress the lung. An Alexis wound protector (Applied Medical; Rancho Santa Margarita, CA, USA) and an intercostal retractor (Miami Instruments; Miami Lakes, FL, USA) are used to expose the mediastinum. If necessary the 2nd rib can be disarticulated from the sternum for additional exposure. We place a small incision for a 5 mm camera port in the same interspace lateral to our main incision. Carbon dioxide is infused at a rate of 8 liters/min through the camera port to reduce the risk of retained intracardiac air.

After identifying the phrenic nerve, the pericardium is opened just superior to the right atrial appendage. There is usually a potential space at this point which makes pericardial entry safer. The pericardiotomy is extended superiorly toward the pericardial reflection to the aorta. Pericardial stay sutures are placed and brought out through separate 1–2 mm incisions using a surgical crochet hook. The site of aortic cannulation is 2–3 cm above the level of the right pulmonary artery. Two 3-0 polypropylene pledgeted purse-string sutures are placed at the aortic cannulation site. Liberal use of stay sutures enhances exposure. The femoral vein is cannulated using Seldinger technique and ultrasound guidance. The venous cannulation site can be pre-closed using a 4-0 Monocryl. We place an Amplatz extra stiff guidewire followed by a 25 Fr QuickDraw venous cannula (Edwards Lifesciences, Irvine, CA, USA) into the superior vena cava (SVC), both with live TEE guidance. The ascending aorta is cannulated using Seldinger technique. Positioning of the guidewire in the descending aorta is confirmed by TEE prior to placement of the arterial cannula into the aortic arch. We use an 18 Fr cannula for patients with body surface area (BSA) less than 2 and a 20 Fr cannula for patients with BSA greater than 2. Cardiopulmonary bypass (CPB) with vacuum assist is initiated and the patient is cooled down to 30 degrees Celsius.
In the setting of aortic insufficiency, we place a retrograde cardioplegia catheter whenever possible using TEE guidance. A 4-0 purse-string suture is placed in the right atrium and the cannula is advanced through the purse-string into the coronary sinus. Pulsatile venous return further confirms coronary sinus placement. If a retrograde catheter cannot be placed, direct coronary ostial perfusion is utilized. We place a 3-0 polypropylene purse-string in the right superior pulmonary vein, through which a drainage tube is advanced to vent the left ventricle. A separate 5 mm incision in the third interspace anterior to mid axillary line is used to place a Chitwood Debakey aortic clamp (Scanlan International; St. Paul, MN, USA), which is then “prepositioned” in the transverse sinus. A 2-0 silk suture is placed about 3–4 cm below the aortic cross clamp to help secure the cardioplegia cannula. The antegrade cardioplegia needle is inserted. The aorta is cross clamped and 20 mg of adenosine is administered, followed by 2 liters of histidine tryptophan ketoglutarate (HTK) cardioplegia solution to enable approximately 2 hours of cross clamp time.
After removal of the cardioplegia needle the aortotomy is made through the needle insertion site. The aortotomy is extended to the left toward the pulmonary artery and to the right towards the non-coronary sinus. The 2-0 silk sutures are used for stay sutures superiorly and laterally.
Commissural stay sutures are placed using 2-0 silk. A gauze pad is placed in the left ventricle temporarily to collect any debris. The leaflets are excised and the annulus sized. In aortic stenosis cases we debride residual calcium away from the annulus.
Annular sutures are placed using shafted instruments. Each suture can be used to facilitate the next suture placement. Each annular suture is then placed through the prosthetic valve sewing ring. When a valve is to be inserted in the supra-annular position, an automated suture delivery system (RAM® Device; LSI SOLUTIONS®, Victor, NY, USA) can be used to place pledgeted annular sutures. When the RAM® Device is used, an automated prosthetic valve suturing device (SEW-EASY® Device; LSI SOLUTIONS®) is used to place the annular sutures through the prosthetic valve sewing ring. Once seated, the valve is secured with the COR-KNOT® Device and titanium fasteners (LSI SOLUTIONS®). The aortotomy is closed using 4-0 polypropylene suture. The left ventricle is de-aired. The cross clamp is released at low flow prior to tying the running suture in order to de-air the aorta. The anesthesiologist uses TEE to meticulously evaluate for appropriate de-airing, ventricular function, and prosthetic valve function. An assessment is also made for the presence of perivalvular leak. CPB is discontinued. In aortic stenosis patients, desmopressin (0.3 mcg/kg IV) is administered after protamine. The aortic cannula is removed and the purse-string is secured with a COR-KNOT® fastener. The peripheral venous cannula is removed and the Monocryl is tied. A drain is placed through the camera port and another through the cross-clamp incision site. The second rib is then secured to the sternum with FiberWire (Arthrex; Naples, FL, USA). Intercostal nerve blocks are performed under direct visualization with bupivacaine (0.25%) with epinephrine. The wound is then closed in layers.
Role of team members
The primary surgeon is responsible for the pre-operative, intraoperative and post-operative care of the patient. In addition, surgical trainees play an integral part in the case. The trainee routinely performs the incision and initial dissection and placement of pericardial stay sutures. The camera view greatly enhances the educational experience of the junior surgical resident as they begin to appreciate the appropriate needle angles, bite depth, etc. The camera view also enables the primary surgeon to easily assess the quality of the trainee’s suturing.
The anesthesiology team places the arterial, central venous and pulmonary artery catheters and performs the endotracheal intubation. An anesthesiologist proficient in advanced perioperative TEE performs a comprehensive TEE examination at the beginning of the case and communicates findings to the surgical team. New or significant ventricular dysfunction or presence of unexpected valvular pathologies may prompt a change in surgical approach. During cannulation for CPB, cooperative TEE guidance helps to avoid intracardiac and aortic injury. Because a single lumen endotracheal tube is used, breath holding is necessary during the mediastinal dissection and placement of the pericardial stay sutures. Frequent and prompt communication between the anesthesiologists, surgeons, and perfusionists is necessary to optimally manage patient ventilation and hemodynamics.
Perfusionists need proficiency with HTK cardioplegia, vacuum assisted CPB, and ultrafiltration. They will interact frequently with the surgeon and anesthesiologist during the case. Nursing teams are actively involved in the pre, intra, and post-operative management of each patient, frequently assessing clinical status and ensuring adequate pain control to promote a quick recovery. Physical therapy plays a key role in helping the patient achieve early ambulation. Utilizing the expertise of this multidisciplinary team, patients can leave the hospital in as few as two days.
Post-operative management
Patients are transferred promptly to a cardiac intensive care unit under the care of fellowship trained critical care intensivists. Patients can be extubated in the operating room. We recommend early removal of chest tubes whenever feasible. Multimodal analgesic therapy, including intercostal nerve blocks, acetaminophen, and peri-incisional lidocaine patches, helps to reduce narcotic pain medicine requirements and promote early mobilization.
Tips, tricks and pitfalls
Communication is essential between the surgeon and anesthesiologist especially during the placement of the CPB wires/catheters. The surgeon should employ liberal use of stay sutures in order to mobilize the aorta prior to cross clamp. The bottom jaw of the clamp must be placed through the upper part of the transverse sinus to avoid pulmonary artery injury. If the aortotomy is deep into the non-coronary sinus, a running closure of the aortotomy should be started before the valve is seated; as it can be difficult to close the aorta once the valve is seated in extended aortotomies. The use of the camera greatly enhances visualization of the aortic valve and annulus. The successful clinical use of an automated suturing device for annular and prosthetic suturing was first reported by Wong et al. In this clinical study, Wong et al. reported that this automated suturing device could facilitate annular suture placement through the right mini-thoracotomy approach (12). The use of an automated suturing device may address the concerns of some surgeons who believe that annular suturing is too difficult through a mini-thoracotomy. Pacing wires can be trickier to place through this approach. It is important to have near normal left and right ventricular function when starting your minimally invasive program as the aortic cross clamp time will probably be longer initially.
Conclusions
Aortic valve replacement can be done safely through a RAM approach. The use of video and automated suturing technology can help to facilitate this approach so that more patients can benefit from having a RAM-AVR.
Acknowledgements
We would like to give special thanks to our AVR patient for agreeing to have photo and video taking during their procedure. We would also like to thank Anthony Ryan and Roger Winkler for producing and editing this video. Thanks also to Jessie Evans, Chris Miller, Richard DiPasquale, Dr. Julie Wyrobek, and Dr. Jude S. Sauer.
Footnote
Conflicts of Interest: CA Johnson Jr received funding through the Peter A. Knight, MD Fellowship Fund that is supported, in part, by LSI SOLUTIONS, Inc, Victor, NY USA.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Malaisrie SC, Barnhart GR, Farivar RS, et al. Current era minimally invasive aortic valve replacement: techniques and practice. J Thorac Cardiovasc Surg 2014;147:6-14. [Crossref] [PubMed]
- Glauber M, Miceli A, Gilmanov D, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. J Thorac Cardiovasc Surg 2013;145:1222-6. [Crossref] [PubMed]
- Gosev I, Neely RC, Leacche M, et al. The impact of a minimally invasive approach on reoperative aortic valve replacement. J Heart Valve Dis 2015;24:181-6. [PubMed]
- Murtuza B, Pepper JR, Stanbridge RD, et al. Minimal access aortic valve replacement: is it worth it? Ann Thorac Surg 2008;85:1121-31. [Crossref] [PubMed]
- Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137:670-9.e5. [Crossref] [PubMed]
- Tabata M, Umakanthan R, Cohn LH, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur J Cardiothorac Surg 2008;33:537-41. [Crossref] [PubMed]
- Miceli A, Murzi M, Gilmanov D, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. J Thorac Cardiovasc Surg 2014;148:133-7. [Crossref] [PubMed]
- Miceli A, Gilmanov D, Murzi M, et al. Minimally invasive aortic valve replacement with a sutureless valve through a right anterior mini-thoracotomy versus transcatheter aortic valve implantation in high-risk patients. Eur J Cardiothorac Surg 2016;49:960-5. [Crossref] [PubMed]
- Glauber M, Miceli A. Minimally invasive aortic valve replacement with sutureless valve is the appropriate treatment option for high-risk patients and the "real alternative" to transcatheter aortic valve implantation. J Thorac Cardiovasc Surg 2016;151:610-3. [Crossref] [PubMed]
- Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr 2013;26:921-64. [Crossref] [PubMed]
- Johnson CA Jr, Melvin AL, Lebow B, et al. Right mini-thoracotomy aortic valve replacement. Asvide 2018;5:096. Available online: http://asvidett.amegroups.com/article/view/22989
- Wong JK, Melvin AL, Siordia JA, et al. Novel Automated Suturing Technology for Minimally Invasive Aortic Valve Replacements. Ann Thorac Surg 2018;105:645-9. [Crossref] [PubMed]
Cite this article as: Johnson CA Jr, Melvin AL, Lebow BF, Yap A, Knight PA. Video assisted right mini-thoracotomy for aortic valve replacement. J Vis Surg 2018;4:39.


