Hemorrhagic complication during robotic surgery in patient with thymomatous myasthenia gravis
Introduction
Most clinicians have demonstrated that the surgical approach for thymectomy in concert with optimized medical management can be considered an effective treatment for myasthenia gravis, although nowadays controversies remain around patient’s age, sex, thymic pathology or duration of disease before surgery (1). Several studies have showed that robotic thymectomy offers perceptible clinical benefits over trans-sternal approach in terms of less postoperative pain, shorter postoperative hospital stay, lower perioperative complications and better cosmetic results (2). To facilitate gentle and precise dissection in an incredibly narrow space as the anterior mediastinum, some authors have also recognized robotic technology as superior to surgeon’s hand in open surgery and to conventional thoracoscopy thanks to instrument’s articulating tips that provide seven degrees of freedom (3).
Case presentation
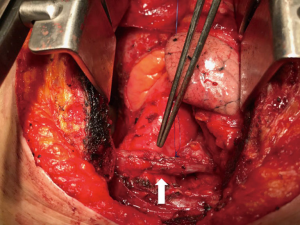
A 74-year-old woman with persistent and moderate generalized myasthenia gravis in medical treatment with acetylcholinesterase inhibitors and steroids, presented to our hospital, upon the recommendation of her neurologist, for surgical removal of an anterior mediastinal mass suspected to be a thymoma. Cervical-thoracic computed tomography scan revealed a homogeneous mass located in the anterior mediastinum, beyond the left innominate vein, and measuring 33 mm × 16 mm. Radical thymectomy was planned through a minimally invasive approach using the da Vinci robot system. With patient positioned supine on the operating table, the left hemithorax was elevated by a roll placed from the patient’s hip to the level of the tip of scapula. Using three-port access, with CO2 insufflation into the pleural cavity, the surgical resection started but during dissection the mass showed partial pericardial infiltration. To ensure a radical resection, pericardium was opened and the dissection continued with an en bloc pericardial resection. In the superior mediastinum, due to the infiltration of the left innominate vein, the maneuvers of resection caused a venous injury that was managed initially through the minimally invasive approach with the packing of the bleeding vessel by gauzes and the pressure held by means of a robotic instrument (Figure 1). For the anatomic location of the injury and to ensure the patient a safe procedure, surgical team decided to convert to median sternotomy. The source of bleeding was carefully inspected and, with proximal and distal vascular control of the left innominate vein encircled by umbilical tapes enclosed into tourniquets (Figure 2), surgeons performed an assessment of injury that was repaired primarily with the application of a permanent monofilament suture, after surgical resection of the mass (Figure 3). Through the trans-sternal approach radical thymectomy was then completed removing all the soft tissue in the anterior mediastinum. Two 28-Fr chest tubes were left in place with sternal and minimally invasive thoracic incisions closure. The patient had an uneventful postoperative stay. She didn’t need any blood transfusion and was discharged on the fifth postoperative day. Histologic examination showed Type B3 thymoma. The patient was in Masaoka Stage III.


Discussion
In the surgical treatment of patients with myasthenia gravis, many authors suggest to plan a minimally invasive approach using the da Vinci robot system because the trans-sternal approach led to early clinical outcomes less excellent in terms of hospital stay, need of postoperative medication and cosmetic satisfaction (5-7). In our case it was necessary to complete the surgical procedure through conversion to trans-sternal approach for three reasons: the minimally invasive thymectomy couldn’t be safely completed due to a vascular injury not easy to manage for its anatomic location; some authors argue that a radical surgical resection is the main predictive factor of outcome and survival in patients with extensive thymoma (Masaoka stages III–IV) (8); in the surgical treatment of myasthenia gravis many authors advocate the so called radical thymectomy: en bloc resection of the anterior mediastinal adipose tissues including the thymus gland (9). In presence of an iatrogenic vascular injury, however, it’s advisable, before planning conversion to open approach, immediate control of hemorrhage under clear view of the operative field. In the management of our hemorrhagic complication we have applied pressure immediately to the bleeding vessel with a temporary gauze packing of the superior mediastinum through minimally invasive access incisions and, only after achieving an adequate hemostasis, we evaluated the need to convert. Although many authors have shown that patients undergoing robotic thymectomy demonstrate better early clinical outcomes than those treated with sternotomy approach (5,10), we think that this minimally invasive procedure still has limitations such as the lack of tactile feedback that is very important in the manipulation of delicate tissues. If conversion to sternotomy is chosen due to a vascular injury, the robot has to be undocked and moved away from the operative field and the robotic instrument can’t continue to held pressure on the bleeding vessel: in this case an external pressure by means of a non-robotic instrument could not be a quick solution due to the small size of the access port. During a video-assisted thoracoscopic surgery (VATS) lobectomy with anterior approach, the conversion to thoracotomy in case of major bleeding is facilitated by the mini-thoracotomy placed directly over the major pulmonary vessel (11). Unfortunately, in the anterior mediastinal dissection using the da Vinci robot system, an eventual conversion to sternotomy due to a vascular injury isn’t facilitated by the access ports and requires more time than the extension of a mini-thoracotomy.
Conclusions
Although some authors have demonstrated that thymectomy in patients with thymomatous myasthenia gravis is associated with a poorer outcome than those with non-thymomatous myasthenia gravis (12), surgery is indicated even for elderly patients with thymomatous myasthenia gravis because thymoma is considered a potential malignancy (13). A minimally invasive approach using the da Vinci robot system for radical thymectomy can be proposed because provides excellent postoperative early clinical outcomes in comparison to the trans-sternal approach. However, in case of a vascular injury in the superior mediastinum one should not hesitate to convert to sternotomy if the bleeding control hasn’t been definitely established. This recommendation is also related to the limitations described above regarding the management of major vascular injuries in the mediastinum during robotic surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Frist WH, Thirumalai S, Doehring CB, et al. Thymectomy for the myasthenia gravis patient: factors influencing outcome. Ann Thorac Surg 1994;57:334-8. [Crossref] [PubMed]
- Kumar A, Asaf BB. Robotic thoracic surgery: The state of the art. J Minim Access Surg 2015;11:60-7. [Crossref] [PubMed]
- Nakamura H, Taniguchi Y. Robot-assisted thoracoscopic surgery: current status and prospects. Gen Thorac Cardiovasc Surg 2013;61:127-32. [Crossref] [PubMed]
- Amore D, Scaramuzzi R, Di Natale D, et al. Surgical excision of extensive thymoma using the da Vinci robot system. Asvide 2018;5:093. Available online: http://asvidett.amegroups.com/article/view/22985
- Seong YW, Kang CH, Choi JW, et al. Early clinical outcomes of robot-assisted surgery for anterior mediastinal mass: its superiority over a conventional sternotomy approach evaluated by propensity score matching. Eur J Cardiothorac Surg 2014;45:e68-73. [Crossref] [PubMed]
- Zahid I, Sharif S, Routledge T, et al. Video-assisted thoracoscopic surgery or transsternal thymectomy in the treatment of myasthenia gravis?. Interact Cardiovasc Thorac Surg 2011;12:40-6. [Crossref] [PubMed]
- Hess NR, Sarkaria IS, Pennathur A, et al. Minimally invasive versus open thymectomy: a systematic review of surgical techniques, patient demographics, and perioperative outcomes. Ann Cardiothorac Surg 2016;5:1-9. [PubMed]
- Vardas P, Birdas T. Debulking for Extensive Thymoma. In: Mark K. Ferguson, editor. Difficult Decisions in Thoracic Surgery, Springer 2014:717-23.
- Hatton PD, Diehl JT, Daly BD, et al. Transsternal radical thymectomy for myasthenia gravis: a 15-year review. Ann Thorac Surg 1989;47:838-40. [Crossref] [PubMed]
- Ye B, Li W, Ge XX, et al. Surgical treatment of early-stage thymomas: robot-assisted thoracoscopic surgery versus transsternal thymectomy. Surg Endosc 2014;28:122-6. [Crossref] [PubMed]
- Hansen HJ, Petersen RH. Video-assisted thoracoscopic lobectomy using a standardized three-port anterior approach – The Copenhagen experience. Ann Cardiothorac Surg 2012;1:70-6. [PubMed]
- Papatestas AE, Genkins G, Kornfeld P, et al. Effects of thymectomy in myasthenia gravis. Ann Surg 1987;206:79-88. [Crossref] [PubMed]
- Tsuchida M, Yamato Y, Souma T, et al. Efficacy and safety of extended thymectomy for elderly patients with myasthenia gravis. Ann Thorac Surg 1999;67:1563-7. [Crossref] [PubMed]
Cite this article as: Amore D, Scaramuzzi R, Di Natale D, Curcio C. Hemorrhagic complication during robotic surgery in patient with thymomatous myasthenia gravis. J Vis Surg 2018;4:41.


