Awake transcatheter aortic valve replacement—an anesthesiologist’s perspective
Transcatheter aortic valve replacement (TAVR) has become the standard of care for prohibitive or high-risk patients with severe aortic stenosis (1). Recent advancements in technology, especially better valve design to reduce perivalvular leak, much smaller sheath size, less requirements for rapid right ventricular pacing/balloon valvuloplasty and decreased need of intraoperative transesophageal echocardiography (TEE) guidance have made the procedure safer and simpler. Due to excellent outcomes of TAVR, this technology has entered the intermediate risk patient population.
Two major manufactures in the US TAVR market include Edwards Lifesciences Corporation (Irvine, CA, USA) and Medtronic (Minneapolis, MN, USA). US Food and Drug Administration approved the Sapien 3 transcatheter heart valve by Edwards Lifesciences Corporation on August 18 2017 for patients with severe, symptomatic aortic stenosis who are at intermediate risk for open-heart surgery. Edwards Sapine 3 valve in intermediate risk patients demonstrated 75% lower rates of 30-day all-cause mortality and disabling stroke compared to surgery with an impressive 1.1% all cause mortality, 1% disabling stroke and only 1.5% moderate to severe perivalvular leak (2,3). The newest Medtronic EvolutR TAVR valve showed a 1.7% mortality rate, 1.7% disabling stroke, 10% pacemaker rate and 0% moderate to severe perivalvular leak (4). It is expected that TAVR instead of surgical aortic valve replacement will become the mainstay treatment for aortic valve stenosis in the following years.
General anesthesia (GA) vs. monitored anesthesia care (MAC) for TAVR
GA is defined by the patient having been placed in a state of “unconsciousness” such that they are unaware of their physical state and are unable to communicate. Typically, this involves administration of either inhalational or intravenous anesthetic agents, paralyzing agents, insertion of an endotracheal tube, and artificial ventilation. The decision to choose GA vs. MAC for TAVR appears to be guided by only a few patient-related factors and dominated by local and national practice. TAVRs used to be performed routinely under GA with endotracheal intubation, comprehensive hemodynamic monitoring with arterial line, central line and pulmonary artery catheters, intraoperative TEE and mandatory ICU care postoperatively. The perceived benefits include full control of the airway, allowing quick conversion to open surgery if complications occur and the use of intraoperative TEE for accurate sizing and prompt recognition of complications (cardiac tamponade, dissection, valve embolization, annular rupture, etc.). In many centers, this is still the preferred approach.
MAC usually involves in varying levels of sedation, analgesia and anxiolysis when necessary. There are many terminologies in the literature regarding MAC. In this article, MAC refers to non-GA and the patient remains conscious and is able to respond to verbal/tactile commands i.e., awake TAVR. It is generally accepted that MAC becomes a GA when the patient loses the ability to respond to commands. Advantages of MAC include less hemodynamic manipulations required, shorter hospital stay, shorter ICU stay, no prolonged intubation (no tube to start with), early mobilization, the ability to assess neurological status throughout the procedure and reduced net cost to healthcare systems. In Germany and Israel, 100% of TAVRs were performed under MAC in 2014 (5). The use of MAC has increased significantly over the years and myocardial infarction, major stroke and in hospital death rates were found to be similar between GA and MAC groups (5). A recent systemic review and meta-analysis of seven studies found that MAC was associated with a shorter hospital stay by 3 days and a shorter procedure time by 36.3 minutes. Overall 30-day mortality was not significantly different between MAC and GA, also cardiac- and procedure-related mortality was similar between both groups (6). The recent ADVANCE study found no statistically significant differences existed between the MAC and GA groups in all-cause mortality, cardiovascular mortality, or stroke, through 2-year follow-up (7). The conversion rate from MAC to GA was 5.3% with majority of them due to procedural complications or patient discomfort (7).
When MAC for TAVR was initially started, high level of sedation was utilized including dexmedetomidine and propofol infusions to ensure patients’ tolerance of the insertion of TEE probe and large sheath introducers. In reality, these “Big MAC” patients have lost consciousness and are truly GA without an advanced airway. A true MAC for TAVR should be a patient who is comfortable and responsive to commands throughout the procedure with the use of generous local anesthetic infiltration by the cardiac surgeons/cardiologists and light sedative medications.
Preoperative evaluation & monitoring
The TAVR patient population is general very sick and many patients carry significant co-morbidities, including ventricular and other valvular dysfunctions, pulmonary insufficiency requiring home oxygen, stroke, kidney dysfunction and chronic pain syndromes. A detailed and frank discussion with patients by surgeons and anesthesiologists as soon as possible is critical for a successful awake TAVR program. Patients’ expectation to go to sleep for heart surgery must be reasoned with multiple reassurances from all team members. We state clearly that “you will be awake during this procedure and we will do everything we can to make sure you are comfortable. This is for your own safety.”
Narcotics are avoided in the preoperative area. Small dose of midazolam (0.5–1 mg) is given for the radial arterial line placement. Anticoagulation medications (aspirin, clopidogrel, warfarin etc.) are continued throughout the perioperative area because of reduced bleeding complications with newer and smaller sheath size and routine use of Perclose (Abbott Vascular, Abbott Park, IL, USA) devices in our practice. To minimize hypotensive events during valve deployment, beta-blockers and angiotensin converting enzyme inhibitors are withheld 24 hours before surgery. Two 16 G peripheral IV are placed in the preoperative area for intraoperative volume and medication administration.
With newer TAVR valve designs, pacemaker rates have dramatically decreased over the years. Preoperative ECGs are reviewed to identify any heart block. Transvenous pacemaker through right internal jugular vein is placed by anesthesiologists in preoperative area for any heart block regardless of the types of TAVR valves selected. Confirmation of adequate pacer lead position was achieved when consistent right ventricular pacing capture was obtained at 0.1 mA (Figure 1). Once the patient is in the OR, fluoroscopy is used to double check correct temporary pacer lead position in the apex of right ventricle.

Intraoperative management
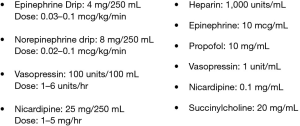
When the patient arrives in the hybrid operating room, standard American Society of Anesthesiologists monitors, radial arterial line, BIS monitor (Medtronic, Minneapolis, MN, USA) are placed. Nasal cannula with end tidal CO2 monitoring capacity is used to provide continuous supplemental oxygen and assess ventilation. Patients with severe aortic valve stenosis invariably have pulmonary hypertension. Any hypoxia or hypercardia from over-sedation could further worsen existing pulmonary hypertension and right heart failure. The level of sedation is evaluated closely and BIS value is kept between 70 and 80. The following medications are prepared but not spiked (Figure 2). Baseline transthoracic echocardiography (TTE) is performed by an echocardiography technician and cardiac anesthesiologist.
Ketamine is N Methyl-D-Aspartate (NMDA) antagonist and can provide dissociative amnesia, anesthesia and analgesia. Small dose (20–30 mg) of ketamine is given after monitors are placed and 1–2 mg midazolam has been given. Most patients will achieve a comfortable stage and require no more sedation (Figure 3) (8). Generous local anesthetics (Lidocaine) are applied by the interventionists before starting the procedure. Motion of patients is expected and accepted by all TAVR team members.

A temporary pacemaker is placed through femoral vein if there is no pacer placed preoperatively in the internal jugular vein. Aortic root injection catheter is placed through the femoral artery on one side and the TAVR introducer is placed on the other side. The most painful portion of the procedure is the placement of large TAVR introducer and a small dose of propofol might be required for comfort. Anesthesiologists use the side port of the pacer introducer as central line for volume and medication administration. When the introducer is placed in the femoral artery, heparin is given to maintain activated clotting time around 250 to prevent thrombosis.
When the wire crosses the aortic valve, significant arrhythmia will ensue. 1–2 mg magnesium and 100 mg lidocaine IV are given to mitigate arrhythmia. If arrhythmia persists, reposition of the wire is needed. When “the valve on a stick” is delivered across the aortic valve, the already stenotic aortic valve is now almost completely obstructed. Significant hypotension is inevitable and epinephrine/vasopressin is frequently required to maintain hemodynamic stability. Balloon valvuloplasty is skipped on many cases now due to smaller size of the delivery system. Right ventricular pacing may or may not be needed depending on the TAVR system used (YES for Edwards Sapien valve and NO for Medtronic Evolut valve). Once the valve is successfully deployed, close attention should be paid to possible heart block and pacemaker should be promptly initiated if needed. TTE is then performed to evaluate any perivalvular leak and pericardial effusion.
When the team is satisfied with the placement of TAVR valve, the anesthesiologist must get ready to treat hypertension now. Explanations for post TAVR hypertension include immediate relief of stenosis/afterload and a hyperdynamic left ventricle. Usually antihypertensives including nicardipine and nitroglycerin are required to treat impressive hypertension.
No more sedation is required after the valve is deployed and inotropes and vasopressors are turned off. Patient should be fully awake at the end of procedure and escorted to a step-down unit for recovery. Most patients go home the next day if no complication is identified.
Intraoperative focused TTE
Sizing of the TAVR valve has been achieved mainly by CT scan at our hospital and intraoperative TEE is not routinely required to size the valve any more. The goals of pre-TAVR focused TTE are to identify aortic valve annular size, severity of aortic stenosis, mitral valve diseases, left ventricular function and any pericardial effusion. Commonly used views are parasternal long axis view, aortic valve short axis view, left ventricular short axis view, apical four chamber view, apical two chamber view and 3D assessments.
Once the valve is deployed, TTE is used to assess position of the valve, severity and location of perivalvular leak, left ventricular function and any new pericardial effusion. Most useful views are parasternal long axis view, aortic valve short axis view, left ventricular short axis view, apical four chamber view, apical two chamber view (Figures 4,5) (9,10). When hemodynamic instability is encountered, TTE could also be used to figure out etiologies and guide therapies throughout the procedure.
Cardiac arrest during TAVR procedures
TAVR patients are generally very sick and cardiac arrest happens not uncommonly during the procedure. The TAVR team must be trained and well coordinated in emergent resuscitation to save patient’s life. Severe aortic stenosis and associated left ventricular hypertrophy make chest compression less effective and very high quality chest compressions must be given and guided by arterial line pressure. The goal is to maintain a mean blood pressure of 65–75 mmHg with each compression at a rate of 100 bpm.
When cardiac arrest is confirmed, airway should be secured and standard Advanced Cardiac Life Support protocols should be followed. TAVR valve should be quickly deployed and hemodynamics usually immediately improves. If asystole is encountered, transvenous pacer should be initiated. This should be the first step of resuscitation during TAVR and patients usually can be stabilized and extubated in the operating room. Cardiopulmonary bypass should be reserved if hemodynamics is not improved with TAVR deployment. Many of these TAVR patients are considered high risk or inoperable. Emergent sternotomy and surgical aortic valve replacement often leads to poor outcomes.
Summary
TAVR is a safe and effective procedure and has made great progress over the years. Awake TAVR can be performed with minimal sedation successfully with experiences and great teamwork.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 2014;370:1790-8. [Crossref] [PubMed]
- Thourani VH, Kodali S, Makkar RR, et al. Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: a propensity score analysis. Lancet 2016;387:2218-25. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Grube E, Van Mieghem NM, Bleiziffer S, et al. Clinical Outcomes With a Repositionable Self-Expanding Transcatheter Aortic Valve Prosthesis: The International FORWARD Study. J Am Coll Cardiol 2017;70:845-53. [Crossref] [PubMed]
- Dall'Ara G, Eltchaninoff H, Moat N, et al. Local and general anaesthesia do not influence outcome of transfemoral aortic valve implantation. Int J Cardiol 2014;177:448-54. [Crossref] [PubMed]
- Fröhlich GM, Lansky AJ, Webb J, et al. Local versus general anesthesia for transcatheter aortic valve implantation (TAVR)--systematic review and meta-analysis. BMC Med 2014;12:41. [Crossref] [PubMed]
- Brecker SJ, Bleiziffer S, Bosmans J, et al. Impact of Anesthesia Type on Outcomes of Transcatheter Aortic Valve Implantation (from the Multicenter ADVANCE Study). Am J Cardiol 2016;117:1332-8. [Crossref] [PubMed]
- Huang J, Wang S, Lu J. A true awake transcatheter aortic valve replacement. Asvide 2018;5:108. Available online: http://asvidett.amegroups.com/article/view/23014
- Huang J, Wang S, Lu J. Parasternal long axis view to assess valve position and perivalvular leak by transthoracic echocardiography. Asvide 2018;5:109. Available online: http://asvidett.amegroups.com/article/view/23016
- Huang J, Wang S, Lu J. Apical four chamber view to assess valve position and perivalvular leak by transthoracic echocardiography. Asvide 2018;5:110. Available online: http://asvidett.amegroups.com/article/view/23017
Cite this article as: Huang J, Wang S, Lu J. Awake transcatheter aortic valve replacement—an anesthesiologist’s perspective. J Vis Surg 2018;4:44.