Con—debate: short circulatory arrest times in arch reconstructive surgery: is simple retrograde cerebral perfusion or hypothermic circulatory arrest as good or better than complex antegrade cerebral perfusion for open distal involvement or hemi-arch?
Aortic arch open surgery continues to represent a formidable challenge for heart surgeons.
In fact, the interruption of physiological brain perfusion is a major detrimental effect during the systemic circulatory arrest resulting in a series of neurological complications. In order to protect the brain from these injuries, three techniques have been proposed and widely utilized as a means of protecting the brain: deep hypothermic circulatory arrest (DHCA), retrograde cerebral perfusion (RCP) and antegrade cerebral perfusion (ACP). The basis for all the techniques is the protection afforded by hypothermia with the consequent metabolic suppression.
The duration of cerebral protection is an important consideration, which has to be evaluated in the selection of the appropriate cerebral protection method. In fact, although the three techniques have provided for safer thoracic aortic surgery and increased perfusion times, the time of brain perfusion is not unlimited and in light of this, debate remains as to the better cerebral circulatory management technique for arch reconstructive surgery with short circulatory arrest times. It is universally accepted that DHCA, although is a simple and valid method of brain protection, has the main disadvantage of a limited “safe” time of circulatory arrest. In fact, the “safe” time-period of DHCA to prevent neurologic injuries has been showed to be less than 45 minutes at 18 °C, with some authors who showed an increase of the rate of neurologic deficit with DHCA-time ranged between 30 and 50 minutes (1). It is clear how, in order to increase the “safe” time of DHCA, adjunct techniques of RCP and ACP with various levels of hypothermia have been adopted.
In 1992, Ueda and co-workers published the first series on continuous RCP in combination with DHCA during aortic arch surgery (2). Before DHCA introduction, the technique was realized using the bypass connecting the arterial and venous lines of the extracorporeal circuit to reverse the flow into the superior vena cava cannula (2,3). In this landmark paper, circulatory arrest times ranged from 11 to 56 minutes and nasopharyngeal temperatures ranged from 16 to 18 °C (2). Thereafter, the same technique evolved, operative times shorten, early mortality and morbidity improved and many other series finally validated the efficacy of RCP for cerebral protection (1,4-7). However, during the same decades, the excellent results coming from the ACP with a direct cannulation of the supraaortic vessels progressively clouded the retrograde technique (8-10).
Although potential benefits of the RCP have been proved in terms of the embolic debris, intracranial hypothermia maintenance and cerebral metabolic support, other possible disadvantages have been identified in clinical and experimental studies.
Reich et al. performed preoperative and postoperative neuropsychological evaluation in 21 patients undergoing DHCA and RCP during elective thoracic aortic repair (11). The overall cognitive and memory dysfunctions had strong associations with RCP, even when controlling separately for age and cerebral ischemic time. In another study, Okita and colleagues (12) compared 60 consecutive patients who underwent total arch replacement using DHCA with RCP or with selective ACP. They performed serial brain imaging CT scan, neurological examination, and cognitive function tests. Both methods of brain protection resulted in acceptable levels of mortality and morbidity but the incidence of transient brain dysfunction was significantly higher in the RCP group than in the ACP group (33% vs. 13%, P=0.05) (12).
In a prospective randomized trial, Harrington and coworkers (13) assess neuropsychometric outcomes in 38 patients requiring elective aortic arch surgery using hypothermic circulatory arrest plus RCP or hypothermic circulatory arrest alone. At 6 weeks postoperatively, 77% of the hypothermic circulatory arrest group and 93% of the hypothermic circulatory arrest plus RCP group had a deficit. Moreover, neuropsychometric change did not correlate with hypothermic circulatory arrest duration and procedure. They conclude that hypothermic circulatory arrest despite the use of RCP is associated with a high incidence of neuropsychometric changes even in apparently safe arrest duration.
In a primate study, Boeckxstaens and Flameng (14) compared DHCA alone and with RCP after 1 hour of circulatory arrest at 18 °C temperature. Results showed a significant reduction in the brain flow during RCP with less than 1% of arterial inflow returned to the aortic arch and histologic analysis identified slightly more glial edema in the RCP group.
Similarly, Juvonen and colleagues (15) developed a porcine model to assess the impact on histologic and behavioral outcome of provoked cerebral arterial embolization, comparing RCP with continued antegrade perfusion. Complete behavioral recovery was seen in all surviving animals but demonstrated that significant mild ischemic damage occurred after RCP, even in non-embolized animals, compared to the control group.
On the other hand the studies comparing antegrade vs. retrograde cerebral protection failed to provide definite answers for a true benefit of RCP (1,16,17).
A meta-analysis including over 5,000 patients concluded that no differences existed between ACP and RCP (16). In particular, 2,855 were treated with DHCA plus antegrade perfusion and 1,897 were treated with DHCA plus retrograde perfusion (16). However, of the 15 comparative studies selected for the analysis only 1 reported a circulatory arrest time above 60 minutes whereas all the others ranged from 18 to 44 minutes.
Okita et al. (18) according to the Japanese adult cardiovascular surgery database reporting the results of 16,218 total arch replacement between 2009 and 2012, provide comparable clinical outcomes with regard to mortality and stroke rates between the two methods of cerebral protection. However, DHCA with RCP resulted in a higher incidence of prolonged intensive care stay and towards an increased incidence of stroke (6.7% vs. 8.6%) compared to ACP.
Moreover the study failed to report data regarding brain perfusion time or circulatory arrest time.
In the Leipzig experience (17) the authors clearly reported in 636 consecutive aortic arch replacement, as ACP is associated with significantly less neurologic complications than RCP and DHCA, despite longer circulatory arrest times. Circulatory arrest time was 22±17 minutes with unilateral cerebral perfusion, 23±21 minutes with bilateral cerebral perfusion, 18±12 minutes with RCP and 15±13 minutes with DHCA. The results showed a significantly lower incidence of permanent neurological deficit among ACP patients (9% vs. 15%, P=0.035) and the use of any form of antegrade perfusion was identified as protective against the development of neurological dysfunction at multivariate analysis.
The only randomized controlled trial comparing DHCA with ACP confirmed this hypothesis after a deep analysis of the pre- and post-arrest cerebral metabolism between the two techniques (19). Forty-two patients undergoing elective or emergency aortic arch surgery via a median sternotomy were assigned to HCA or ACP. HCA occurred at a nasopharyngeal temperature of 15 °C and ACP at a corporeal temperature of 25 °C. Neurological monitoring was conducted using metabolic (oxygen measurements and extraction), transcranial Doppler and Neuropsychometric examinations. The study clearly showed as ACP attenuates the cerebral metabolic deficit seen after HCA as no decrease in jugular venous pO2 and a reduction in transcranial oxygen extraction were observed after reinstituting total body perfusion (19).
In summary, studies evidences and clinical practice indicates that RCP efficacy in cerebral protection could be justified in short period of DHCA but seems very limited for prolonged DHCA time. Truly, a reasonable doubt concerns also the possibility to prolong cerebral ischemic times during arch surgery. Who can really anticipate short DHCA during elective or limited aortic arch surgery? This complex surgery can always hide unexpected complications causing a prolonged procedure time. Another limitation for the RCP regards the possibility to use two different techniques in the same surgical staff (retrograde perfusion for hemiarch procedures and antegrade for total arch procedures), as mentioned by Milewski et al. of the University Hospital of Pennsylvania (1). Usually these challenging aortic procedures, to achieve satisfactory results, require standardized protocols and confidence in the operative technique. It is very difficult to modify every time the operative practice according to the extension of the arch repair if there is already a cerebral protection strategy that has proved to be effective in the short and long run. In fact, it is not always easy to respect the initial program regarding the extension of the arch replacement.
To confirm these hypotheses, a clear trend towards ACP is noticeable in literature and real world data (18,20-22). Since its first introduction by Kazui et al. (23) in the 1990s this method of cerebral protection has long been used as an adjunctive cerebral protective technique. Of course ACP was refined over time according to different philosophies for blood gas management, ideal temperature, ACP-flows and possibilities of concomitant myocardial or descendent aortic perfusion. Today the most commonly adopted a strategy involves moderate hypothermia (nasopharyngeal 25–26 °C), bilateral hemisphere perfusion and a cerebral flow rate of 10–15 mL/kg/min adjusted to maintain a right radial arterial pressure between 40 and 70 mmHg.
In a recent European survey on current trends in cannulation and neuroprotection-strategies during surgery of the aortic arch, retrograde perfusion was used as method of cerebral protection only in 3% of the cases and exclusively in acute clinical presentation (20). Furthermore, Urbanski et al. (21) in a more recent multicentre analysis collected the data of 1,232 consecutive patients who underwent elective aortic arch repair with reimplantation of at least one supra-aortic artery and only 1/1,232 patient from 11 European cardiovascular centres involved in the study received a RCP (21).
In Japan, according to the recent analysis based on the Japan Adult Cardiovascular Surgery Database there was also a progressive increase in the use of ACP during the years. During the study-period, of the overall population, 7,038 patients had ACP and 1,141 patients had hypothermic circulatory arrest with RCP. Moreover, in the matched population antegrade perfusion increased from 18.1% in 2009 to 32.4% in 2012 becoming the most favorite method of cerebral protection over RCP used in the 30.9% of cases (18).
Only in North America, according to the Society of Thoracic Surgeons Database (n=12,521 cases of aortic arch repair), RCP is still the preferred method of cerebral protection (16% against 14% of antegrade perfusion) (22). However, during the study interval only 17% of the procedures were performed under moderate hypothermia instead the remaining arch procedures were supported by lesser degrees of hypothermic circulatory arrest (<24 °C) which probably provided additional cerebral protection regardless of the strategy chosen during arch repair; and also in this study the median circulatory arrest time was shorten than 30 minutes (22). Nevertheless, it has been documented that profound hypothermia causes coagulation disorders, predisposing to postoperative bleeding and that prolonged periods of perfusion for cooling and rewarming are associated with clotting-factor depletion and interference with blood coagulation (24).
Table 1 is reporting a comprehensive overview of the principal series comparing different strategies for cerebral protection.
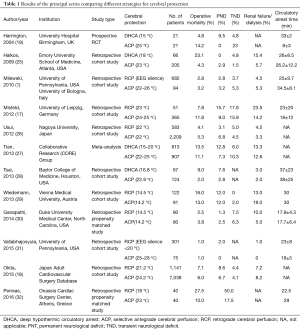
Full table
In conclusion, only 30 years ago retrograde and anterograde cerebral perfusion represented two equally distributed strategies for cerebral protection. Nowadays, despite the proven safety of RCP during open arch surgery for limited circulatory arrest time there is a widespread acceptance of ACP as preferred choice of cerebral protection. We think that, also for short circulatory arrest time, ACP with moderate hypothermia and bilateral perfusion represent the best solution, and with reference to the topic of the debate, we strongly believe that “complex” is the arch reconstructive surgery, not the ACP technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Milewski RK, Pacini D, Moser GW, et al. Retrograde and antegrade cerebral perfusion: results in short elective arch reconstructive times. Ann Thorac Surg 2010;89:1448-57. [Crossref] [PubMed]
- Ueda Y, Miki S, Kusuhara K, et al. Deep hypothermic systemic circulatory arrest and continuous retrograde cerebral perfusion for surgery of aortic arch aneurysm. Eur J Cardiothorac Surg 1992;6:36-41. [Crossref] [PubMed]
- Ueda Y, Miki S, Kusuhara K, et al. Surgical treatment of aneurysm or dissection involving the ascending aorta and aortic arch, utilizing circulatory arrest and retrograde cerebral perfusion. J Cardiovasc Surg (Torino) 1990;31:553-8. [PubMed]
- Yang Y, Yang L, Sun J, et al. A modified protocol for retrograde cerebral perfusion: magnetic resonance spectroscopy in pigs. Eur J Cardiothorac Surg 2013;43:1065-71. [Crossref] [PubMed]
- Estrera AL, Miller CC 3rd, Lee TY, et al. Ascending and transverse aortic arch repair: the impact of retrograde cerebral perfusion. Circulation 2008;118:S160-6. [Crossref] [PubMed]
- Safi HJ, Miller CC 3rd, Lee TY, et al. Repair of ascending and transverse aortic arch. J Thorac Cardiovasc Surg 2011;142:630-3. [Crossref] [PubMed]
- Ueda Y. A reappraisal of retrograde cerebral perfusion. Ann Cardiothorac Surg 2013;2:316-25. [PubMed]
- Pacini D, Leone A, Di Marco L, et al. Antegrade selective cerebral perfusion in thoracic aorta surgery: safety of moderate hypothermia. Eur J Cardiothorac Surg. 2007;31:618-22. [Crossref] [PubMed]
- Di Bartolomeo R, Di Eusanio M, Pacini D, et al. Antegrade selective cerebral perfusion during surgery of the thoracic aorta: risk analysis. Eur J Cardiothorac Surg 2001;19:765-70. [Crossref] [PubMed]
- Dossche KM, Morshuis WJ, Schepens MA, et al. Bilateral antegrade selective cerebral perfusion during surgery on the proximal thoracic aorta. Eur J Cardiothorac Surg 2000;17:462-7. [Crossref] [PubMed]
- Reich DL, Uysal S, Ergin MA, et al. Retrograde cerebral perfusion during thoracic aortic surgery and late neuropsychological dysfunction. Eur J Cardiothorac Surg. 2001;19:594-600. [Crossref] [PubMed]
- Okita Y, Minatoya K, Tagusari O, et al. Prospective comparative study of brain protection in total aortic arch replacement: deep hypothermic circulatory arrest with retrograde cerebral perfusion or selective antegrade cerebral perfusion. Ann Thorac Surg 2001;72:72-9. [Crossref] [PubMed]
- Harrington DK, Bonser M, Moss A, et al. Neuropsychometric outcome following aortic arch surgery: a prospective randomized trial of retrograde cerebral perfusion. J Thorac Cardiovasc Surg 2003;126:638-44. [Crossref] [PubMed]
- Boeckxstaens CJ, Flameng WJ. Retrograde cerebral perfusion does not perfuse the brain in nonhuman primates. Ann Thorac Surg 1995;60:319-27. [Crossref] [PubMed]
- Juvonen T, Weisz DJ, Wolfe D, et al. Can retrograde perfusion mitigate cerebral injury after particulate embolization? A study in a chronic porcine model. J Thorac Cardiovasc Surg 1998;115:1142-59. [Crossref] [PubMed]
- Hu Z, Wang Z, Ren Z, et al. Similar cerebral protective effectiveness of antegrade and retrograde cerebral perfusion combined with deep hypothermia circulatory arrest in aortic arch surgery: a meta-analysis and systematic review of 5060 patients. J Thorac Cardiovasc Surg 2014;148:544-60. [Crossref] [PubMed]
- Misfeld M, Leontyev S, Borger MA, et al. What is the best strategy for brain protection in patients undergoing aortic arch surgery? A single center experience of 636 patients. Ann Thorac Surg 2012;93:1502-8. [Crossref] [PubMed]
- Okita Y, Miyata H, Motomura N, et al. A study of brain protection during total arch replacement comparing antegrade cerebral perfusion versus hypothermic circulatory arrest, with or without retrograde cerebral perfusion: analysis based on the Japan Adult Cardiovascular Surgery Database. J Thorac Cardiovasc Surg 2015;149:S65-73. [Crossref] [PubMed]
- Harrington DK, Walker AS, Kaukuntla H, et al. Selective antegrade cerebral perfusion attenuates brain metabolic deficit in aortic arch surgery: a prospective randomized trial. Circulation 2004;110:II231-6. [Crossref] [PubMed]
- De Paulis R, Czerny M, Weltert L, et al. Current trends in cannulation and neuroprotection during surgery of the aortic arch in Europe. Eur J Cardiothorac Surg 2015;47:917-23. [Crossref] [PubMed]
- Urbanski PP, Luehr M, Di Bartolomeo R, et al. Multicentre analysis of current strategies and outcomes in open aortic arch surgery: heterogeneity is still an issue. Eur J Cardiothorac Surg 2016;50:249-55. [Crossref] [PubMed]
- Englum BR, He X, Gulack BC, et al. Hypothermia and cerebral protection strategies in aortic arch surgery: a comparative effectiveness analysis from the STS Adult Cardiac Surgery Database. Eur J Cardiothorac Surg 2017;52:492-8. [Crossref] [PubMed]
- Kazui T, Kimura N, Yamada O, Komatsu S. Surgical outcome of aortic arch aneurysms using selective cerebral perfusion during. Ann Thorac Surg 1994;57:904-11. [Crossref] [PubMed]
- Pacini D, Di Marco L, Di Bartolomeo R. Methods of cerebral protection in surgery of the thoracic aorta. Expert Rev Cardiovasc Ther 2006;4:71-82. [Crossref] [PubMed]
- Halkos ME, Kerendi F, Myung R, et al. Selective antegrade cerebral perfusion via right axillary artery cannulation reduces morbidity and mortality after proximal aortic surgery. J Thorac Cardiovasc Surg 2009;138:1081-9. [Crossref] [PubMed]
- Usui A, Miyata H, Ueda Y, et al. Risk-adjusted and case-matched comparative study between antegrade and retrograde cerebral perfusion during aortic arch surgery: based on the Japan Adult Cardiovascular Surgery Database: the Japan Cardiovascular Surgery Database Organization. Gen Thorac Cardiovasc Surg 2012;60:132-9. [Crossref] [PubMed]
- Tian DH, Wan B, Bannon PG, et al. A meta-analysis of deep hypothermic circulatory arrest versus moderate hypothermic circulatory arrest with selective antegrade cerebral perfusion. Ann Cardiothorac Surg 2013;2:148-58. [PubMed]
- Tsai JY, Pan W, Lemaire SA, et al. Moderate hypothermia during aortic arch surgery is associated with reduced risk of early mortality. J Thorac Cardiovasc Surg 2013;146:662-7. [Crossref] [PubMed]
- Wiedemann D, Kocher A, Dorfmeister M, et al. Effect of cerebral protection strategy on outcome of patients with Stanford type A aortic dissection. J Thorac Cardiovasc Surg 2013;146:647-55.e1. [Crossref] [PubMed]
- Ganapathi AM, Hanna JM, Schechter MA, et al. Antegrade versus retrograde cerebral perfusion for hemiarch replacement with deep hypothermic circulatory arrest: Does it matter? A propensity-matched analysis. J Thorac Cardiovasc Surg 2014;148:2896-902. [Crossref] [PubMed]
- Vallabhajosyula P, Jassar AS, Menon RS, et al. Moderate versus deep hypothermic circulatory arrest for elective aortic transverse hemiarch reconstruction. Ann Thorac Surg 2015;99:1511-7. [Crossref] [PubMed]
- Perreas K, Samanidis G, Thanopoulos A, et al. Antegrade or Retrograde Cerebral Perfusion in Ascending Aorta and Hemiarch Surgery? A Propensity-Matched Analysis. Ann Thorac Surg 2016;101:146-52. [Crossref] [PubMed]
Cite this article as: Di Marco L, Murana G, Leone A, Pacini D. Con—debate: short circulatory arrest times in arch reconstructive surgery: is simple retrograde cerebral perfusion or hypothermic circulatory arrest as good or better than complex antegrade cerebral perfusion for open distal involvement or hemi-arch? J Vis Surg 2018;4:46.


