Uniportal video-assisted removal of a right paratracheal pericardial cyst: an unusual location
Introduction
Pleuropericardial cysts (PCs) are a very rare entity, most cases are congenital with a reported incidence of one case in 100,000 people (1). Generally, the most frequent locations of PC are the cardiophrenic angles (2,3). The first reported resection of a PC trough a thoracotomy access was performed by Pickhardt in 1931 (4). The surgical strategy to remove PC has undergone several modifications over the years from standard thoracotomy/sternotomy to video-assisted thoracoscopic surgery (VATS) (5,6). Recently, VATS moved from three port access to a single incision thoracoscopic surgery (SITS) (7). We use the SIST approach to remove a PC in unusual location in the right paratracheal space. To our knowledge this is the first case reported using this technique.
Case presentation
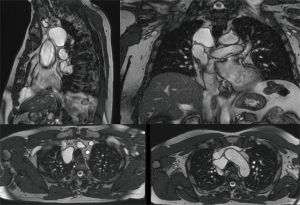
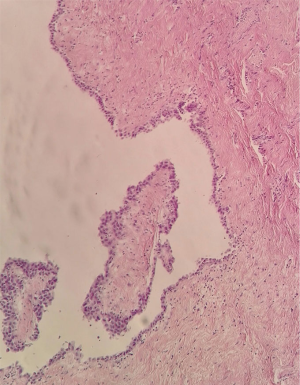
A 56-year-old man was referred to our department because of detection of a right paratracheal lesion of unclear interpretation. The patient complained of atypical chest pain and dry cough in the last 12-months. The patient underwent cardiological evaluation that was negative for ischemic disease or valvulopathy. Physical evaluation and laboratory were normal. The chest X-ray demonstrated an enlargement of the right superior mediastinum over the paratracheal region. Thus, the patient was studied with magnetic resonance imaging (MRI) that confirmed the presence of a homogeneous unilocular mass with low signal intensity on T1-weighted images and increased signal intensity on T2-weighted images located in the right paratracheal region in the space between the azygos vein, the trachea and the epiaortic trunks (Figure 1). The preoperative diagnosis mainly due by anatomical location was bronchogenic cyst. We decided to surgically resect because of symptoms and strong motivation of the patient. The operation was performed using a uniportal video assisted approach. After double lumen endotracheal tube ventilation, a single 3–4 cm incision was made in the fifth intercostal space in between the mid and anterior axillary line. A 10-mm 30° thoracoscope, harmonic scalpel (Harmonic ACE®, Ethicon Inc., USA) and diathermic hook were used as dedicated instrument to allow the dissection of the cyst. The mediastinal pleura was incised in a triangular shape with the azygos vein at the base, the vena cava and vagal nerve on the lateral side. Macroscopically the lesion was clearly water filled and at the end of the dissection we found a clear peduncle connected to the pericardium under the vena cava (Figure 2). Pathological examination of the surgical specimen confirms the diagnosis of PC (Figure 3). The single 24-Fr chest tube was removed in the first post-operative day (POD). The patient was discharged in the 2th POD in optimal clinical condition.

Discussion
Mesothelial cysts represent a rare entity, in particular the right paratracheal location has been reported in only a few cases in literature (5,9,10). This kind of lesion located close to the main bronchi or trachea goes into differential diagnosis, in particular with bronchial cyst even using refined image methods like RMN (5). Generally, PC are asymptomatic and in most cases are detected incidentally (3,5). In this case, conservative management could be an option, but data regarding safety with this strategy are lacking. Surgery is recommended in large cyst cases with compression or impending compression to the nearly structures, in symptomatic patients and to prevent rare, but described complications such as cardiac tamponade, infection, haemorrhagia and sudden death. In the past, thoracotomy or sternotomy were the favorite surgical accesses to remove PC. Nowadays in the era of video assisted thoracic surgery, open surgery is indicated only in a few cases with complicated anatomy or extensive adhesions mainly due to inflammation or infection (5,10). Standard three port VATS is the most frequent technique reported in literature with excellent results (5,6). To reduce further the invasiveness, we used a SITS approach that allowed us an easily dissection and removal of the cyst located in the same place in which we perform lymphadenectomy of station 4R and 2R in the treatment of lung cancer. The operation was performed without complications, the cyst was removed intact, the postoperative period was uneventful and the patient was discharged the 2th POD painless and in optimal clinical condition. Video-assisted mediastinoscopy has been reported in literature as an alternative approach to remove PC located in the paratracheal region with good result (6,10). We decided to use SITS because in our opinion thoracoscopy guarantees complete resection of the cyst wall, and is the best way to avoid recurrence, which is not even possible using mediastinoscopy (10). Moreover, we feel that VATS approach is more safe and reproducible due to the extensive experience borrowed with this technique in the treatment of lung cancer (7). In particular using an SITS approach the aesthetics and post-operative course are comparable with mediastinoscopy.
In conclusion, the right paratracheal location of PC is rare but possible, the awareness of this entity is important in differential diagnosis. Minimally invasive surgery, like SITS, is a viable option to remove completely the cyst and resolve symptoms whenever present and avoid rare but severe complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Patel J, Park C, Michaels J, et al. Pericardial cyst: case reports and a literature review. Echocardiography 2004;21:269-72. [Crossref] [PubMed]
- Cohen AJ, Thompson L, Edwards FH, et al. Primary cysts and tumors of the mediastinum. Ann Thorac Surg 1991;51:378-84. [Crossref] [PubMed]
- Maisch B, Seferović PM, Ristić AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J 2004;25:587-610. [Crossref] [PubMed]
- Pickhardt OC. Pleuro-diaphragmatic cyst. Pleuro-diaphragmatic cyst. In: Transactions of the New York Surgical Society-Stated Meeting held April 12, 1933. Ann Surg 1934;99:814-6.
- Kar SK, Ganguly T. Current concept of diagnosis and management of pericardial cyst. Indian Heart J 2017;69:364-70. [Crossref] [PubMed]
- Mouroux J, Venissac N, Leo F, et al. Usual and unusual locations of intrathoracic mesothelial cyst. Is endoscopic resection always possible? Eur J Cardiothorac Surg 2003;24:684-8. [Crossref] [PubMed]
- Rocco G. One port (uniportal) video-assisted thoracic surgical resections - a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Dell'Amore A, Campisi A, Giunta D, et al. Uniportal VATS removal of the right paratracheal pericardial cyst. Asvide 2018;5:129. Available online: http://www.asvide.com/article/view/23407
- Chang WC, Tzao C, Hsu HH. Unusual location of right paratracheal pericardial cyst. J Med Sci 2004;24:55-8.
- Pop D, Venissac N, Leo F, et al. Video-assisted mediastinoscopy: a useful technique for paratracheal mesothelial cysts. J Thorac Cardiovasc Surg 2005;129:690-1. [Crossref] [PubMed]
Cite this article as: Dell’Amore A, Campisi A, Giunta D, Congiu S, Dolci G, Agosti R. Uniportal video-assisted removal of a right paratracheal pericardial cyst: an unusual location. J Vis Surg 2018;4:55.


