Why to be cautious with the use of the frozen elephant trunk in acute type A aortic dissection
Already at the second meeting Aortic meeting in Bologna, I showed a slide confirming that type A dissection is a life-threatening disease with high rate of early mortality. What threatens the patients is blood in the pericardium causing tamponade. In Germany and The Netherlands patients are operated on within hours. This is true acute type A dissection surgery. The aortic tissue is so thin that you can literally see the blood streaming, requiring special handling, using Teflon felt between the layers and a Blalock suture diverting the tension away from the actual suture line, whatever technique you use, time consuming and performed under circulatory arrest with antegrade bilateral cerebral perfusion.
In type B dissection is was seen that by covering the intimal tear false lumen thrombosis does occur with decreasing diameter of the aorta in the stented segment with possible but hard to prove advantages for the future with less operations on the post dissected aorta.
To apply this concept to the setting of acute type A dissection is appealing, however, this innovative concept has a price. In a selected group of relatively young patients operated by the highly experienced group from Hannover (1), actually two surgeons who are on duty all year, the mortality rate is low, but as to be expected in this relatively young group of patients, considering that age is a significant risk factor for death (2), however with a rate of dialysis at discharge of 11%, permanent neurological deficit 14% and spinal cord injury rate 8%, figures we never have seen in surgery for type A dissection, unless present before operation.
It may be that closing off upper intercostals arteries together with dissected subclavian arteries with compromised perfusion of vertebral arteries in hemodynamic instability may account for the dreadful complication of spinal cord injury, however, it may also be central body temperatures which in my opinion should be at least 25 degrees or less.
In further building experience Hannover improved their results, however, still with significant neurologic complications (3). We have to realize these results are the best in the world in FET for acute type A dissection.
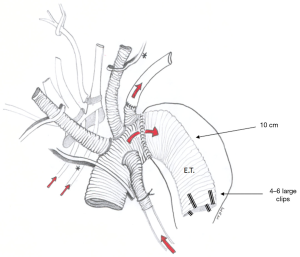
In a patient with type B dissection during pregnancy a rapid post-dissection dilatation was seen of the descending aorta. Since also her root was dilated we decided to perform a valve sparing root first with arch replacement with a classical elephant trunk (Figure 1). The operation went fine but the operation field was narrow because the distal arch was not dilated, providing for body arrest times of 34 and 24 minutes with 10 minutes of reperfusion in between. A difficult elective operation with the best possible circumstances and in day time.
Arch surgery in type A dissection is extremely difficult as was stressed by de group of Freiburg, having seen a 30%-mortality, thereby suggesting to limit the initial operation to hemiarch only and to be liberal with early reoperation in elective setting as the results of this sequential approach were excellent (4).
To apply this difficult arch surgery now combined with a FET in an emergent operation in the middle of the night may easily turn into a nightmare. Not only do you have to make a difficult distal anastomosis as in the technique from Bologna, first reconstructing it with patches, but also to making an anastomosis on a most friable, remote and dissected subclavian artery. No wonder that the operation is also burdened by a recurrent nerve palsy in one fifths of the patients (1), a complication not to be underestimated, especially for this young patient group.
The recommendations of the EACTS expert group for the use of FET trunk in acute type A dissection are the combination of lower body malperfusion, a re-entry or a tear in the distal arch or proximal ascending aorta, clinically stable and young patients (preferably <70 years of age) (3). Let’s be clear, this is only a minority of the patients.
Hannover’s latest policy on this issue on this issue is based on these guidelines, but what is most important is their add that surgery should be performed by a surgical team experienced in performing the procedure (3).
Malakh Shrestha, Eric Roselli, Stephen Lansman, Jo Coselli and Jo Bavaria are regular guests to the Bologna Aortic Meeting every 2 years. They are invited because they have a large experience, a large exposure to the most difficult kind of surgery, the dissected aorta.
In USA, the highest number of root operations are done in only few centers, by these regular guests (5). The rest of the centers are exposed to less than six roots per year! Let’s say one type A per surgeon per year.
It is these surgeons who may be the majority in the audience both in Bologna as well as in the New York Aortic Meeting. Certainly not all are exposed to regular aortic surgery during daytime. Results of operation are obviously better if exposure to aortic surgery is higher, as could be depicted from the above-mentioned STS database study (5), a conclusion which was acknowledged by Lenos and Urbansky in their recent study on acute type A dissection (6), demonstrating better results for experienced surgeons, even considering that these surgeons performed more extensive surgery at the initial operation.
Should surgery then be postponed to the working next day, or even longer? Results will certainly improve and equal the excellence from Professor Sun from Beijing whose acute type A patients may take up to 2 weeks to reach his hospital (7). However, people may die waiting, exposing the total group of type patients to higher risk. The results of the patients who do not reach the hospital or who die during resuscitation are never published. In this respect the mortality for type A dissection should be considered the sum of the mortality of delay plus the mortality of operation.
The question is: should I apply the FET technique being a more experienced aortic surgeon? I sincerely have my doubts. What I do believe is exclusion of the entry tear.
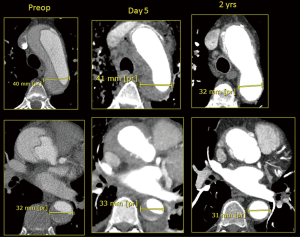
In a patient who presented with malperfusion, cold legs and bloody diarrhea, closing off the entry tear will achieve the same results as in stenting a type B dissection with opening the true lumen and improvement of mesenteric and distal perfusion, as well as a thrombosing false lumen and reducing diameters at follow up (Figure 2). In closing the entry tear we may show the same postoperative images as those from Hannover for patients treated with FET for type A dissection.
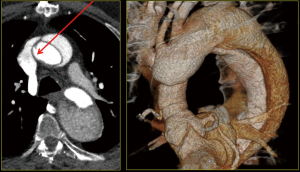
It is persistent proximal false lumen perfusion as in this patient in whom a dilatation of the thoraco-abdominal aorta requires early re-intervention (Figure 3).
This importance of excluding the entry tear was recognized in the extensive experience of Kazui, one of our teachers, a regular guest to the meeting in Bologna and New York (8). The same principle is recognized by the patients from the group of Halstead et al. from New York (9). They found only nine patients to come back for re-operation in future. We found the same in a group of almost 600 patients from the St. Antonius hospital in Nieuwegein, the Netherlands. Yes, people may have died in follow-up years, but only 22 patients came for re-operation at long-term follow-up (10).
And even if an operation on the post-dissection thoracoabdominal aorta is indicated this can be done with good results and with no need for further operation future, and with survival equalling that of the normal Dutch population (11).
It may be worthwhile to concentrate on the aortic root instead as reoperation rate after type A is higher if is the root was dissected, and if the root was reconstructed instead of replaced as was seen with Kazui (8), but also by others (12,13) as also by our group (10).
This principle is also recognized by the experienced group from Hannover, reporting the largest experience with David I procedure in patients with acute type A dissection (14). Results are to be expected from this relatively young patient group with almost the same age as in the FET group. But let’s have a look at the operation time! Aortic cross-clamp time, cerebral perfusion time and total operation time is already quite significant and to add this to the time one need for the complex operation of FET, it may prove to be too much, it may prove to be one mountain too high.
If one has so much believe in stenting the proximal descending aorta, I think it is worthwhile to consider to insert a TEVAR downstream combining it with hit and run ascending and proximal arch replacement as was suggested by the group of Matt from Basel (15), and can be performed with excellent results. The same principle was applied by the group of Sultan and Bavaria (16) in addition to ascending and hemi-arch replacement. However, this relatively easy extension of surgery, almost doubles circulatory arrest time and increases the operation time by one hour, up to 7 hours average. Yes, false lumen trombosis does occur, but not complete in even half of the patients. And yes, there is a significant increase of true lumen diameter but the total lumen diameter does not change.
Techniques like this have to be used overseas as the FET is still not FDA approved, leaving the European and Asian patients being exposed to the inevitable risks of innovation.
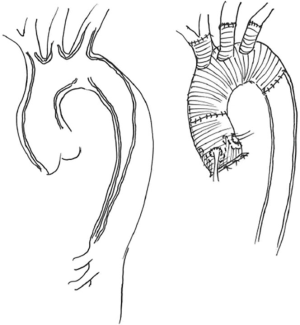
For me, in acute type A dissection, the only indication would be an entry far in the arch, especially those with distal malperfusion, although a complete arch operation is also possible (Figure 4). For all other cases, especially in setting of limited aortic surgery exposure, I think experts should advise on life saving surgery and on focus more on aortic root problems. For the audience, I think it is wise not to go along with all innovations as in the old days of Bologna with people showing off their wealth by building towers and to carefully study the reports of the expert-centers, who do have to be honored for their efforts and to be cautious to implement new techniques, as in the end only one or two techniques will remain, and even these bending over in time.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author is consultant with Vascutek Inc.
References
- Shrestha M, Kaufeld T, Beckmann E, et al. Total aortic arch replacement with a novel 4-branched frozen elephant trunk prosthesis: Single-center results of the first 100 patients. J Thorac Cardiovasc Surg 2016;152:148-59.e1. [Crossref] [PubMed]
- Jussli-Melchers J, Panholzer B, Friedrich C, et al. Long-term outcome and quality of life following emergency surgery for acute aortic dissection type A: a comparison between young and elderly adults. Eur J Cardiothorac Surg 2017;51:465-71. [PubMed]
- Shrestha M, Haverich A, Martens A. Total aortic arch replacement with the frozen elephant trunk procedure in acute DeBakey type I aortic dissections. Eur J Cardiothorac Surg 2017;51:i29-34. [Crossref] [PubMed]
- Rylski B, Beyersdorf F, Kari FA, et al. Acute type A aortic dissection extending beyond ascending aorta: Limited or extensive distal repair. J Thorac Cardiovasc Surg 2014;148:949-54; discussion 954. [Crossref] [PubMed]
- Hughes GC, Zhao Y, Rankin JS, et al. Effects of institutional volumes on operative outcomes for aortic root replacement in North America. J Thorac Cardiovasc Surg 2013;145:166-70. [Crossref] [PubMed]
- Lenos A, Bougioukakis P, Irimie V, et al. Impact of experience on outcome in acute type A aortic dissection. Eur J Cardiothorac Surg 2015;48:491-6. [Crossref] [PubMed]
- Ma WG, Zheng J, Zhang W, et al. Frozen elephant trunk with total arch replacement for Type A aortic dissections: Does acuity affect operative mortality? J Thorac Cardiovasc Surg 2014;148:963-70; discussion 970-2. [Crossref] [PubMed]
- Kazui T, Washiyama N, Bashar AH, et al. Surgical outcome of acute type A dissection: Analysis of risk factors. Ann Thorac Surg 2002;74:75-81; discussion 81-2. [Crossref] [PubMed]
- Halstead JC, Meier M, Etz C, et al. The fate of the distal aorta after repair of acute type A aortic dissection. J Thorac Cardiovasc Surg 2007;133:127-35. [Crossref] [PubMed]
- Malvindi PG, van Putte BP, Sonker U, et al. Reoperation after type A aortic dissection repair: a series of 104 patients. Ann Thorac Surg 2013;95:922-7. [Crossref] [PubMed]
- Alfonsi J, Murana G, Smeenk HG, et al. Open surgical repair of post-dissection thoraco-abdominal aortic aneurysms: Early and late outcomes of a single center study involving over 200 patients. Eur J Cardiothorac Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Immer FF, Aeschimann R, Englberger L, et al. Resuspension of the aortic valve in acute type A aortic dissection: long-term results. J Heart Valve Dis 2008;17:94-7; discussion 97. [PubMed]
- Piccardo A, Regesta T, Pansini S, et al. Fate of the aortic valve after root reconstruction in type A aortic dissection: a 20-year follow up. J Heart Valve Dis 2009;18:507-13. [PubMed]
- Beckmann E, Martens A, Pertz J, et al. Valve sparing David I procedure in acute type A aortic dissection: a 20-year experience with more than 100 patients. Eur J Cardiothorac Surg 2017;52:319-24. [Crossref] [PubMed]
- Matt P, Banerjee P, Grapow M, et al. Modified frozen elephant trunk for acute type A aortic dissection: a comparative study with standard repair technique. Eur J Cardiothorac Surg 2017;51:754-60. [PubMed]
- Sultan I, Wallen TJ, Habertheuer A, et al. Concomitant antegrade stent grafting of the descending thoracic aorta during transverse hemiarch reconstruction for acute DeBakey I aortic dissection repair improves aortic remodeling. J Card Surg 2017;32:581-92. [Crossref] [PubMed]
Cite this article as: Morshuis WJ. Why to be cautious with the use of the frozen elephant trunk in acute type A aortic dissection. J Vis Surg 2018;4:73.