Uniportal VATS lobectomies—masterclass in Bratislava
Introduction
Modern thoracoscopic surgery began in 1991. Lobectomies were performed in the early 1990’s through multiple ports. Uniportal VATS has developed over the last 10 years (1). We started performing minimally invasive surgery in our institution in 1993, paradoxically not with thoracoscopy but with the laparoscopic cholecystectomy. Shortly after that we began with thoracoscopies. In that time only standard simple procedures were performed such as operations for malignant effusions, pneumothorax, lung biopsy, etc. In 2006 we started with antireflux procedures and in 2009 with miniinvasive esophagectomies. Finally in 2012 the first VATS lobectomy was performed. We started using four ports VATS and after we gained enough experience, we reduced the number of ports and since 2016 we perform VATS lobectomies mostly uniportally.
In the first year only six cases were successfully finished, but we have raised the numbers and now we do more than 50% of the cases in minimally invasive way.
We have organized several meetings on VATS lobectomy in our institution including live presentation of the procedures in cooperation with Prof. Batirel.
On February 5–6, we have organized a Masterclass on uniportal VATS lobectomy in Bratislava, attended among others by Prof. Hasan Batirel, the ESTS director of education, Dr. Diego Gonzalez, inventor of uniportal approach to pulmonary resections and Dr. Tomaz Stupnik, inventor of simulators for training VATS lobectomy procedure (Figure 1). On the first day some interesting presentations were given by the participants and there was a possibility to try the simulators under leadership of Prof. Batirel and Dr. Stupnik (Figure 2).

The other day two cases were performed by Dr. Diego Gonzalez, both procedures were transmitted to the conference room, where more than 50 surgeons had the possibility to watch and to discuss the operation (Figures 3,4).

Presentation of the patients
Case no. 1
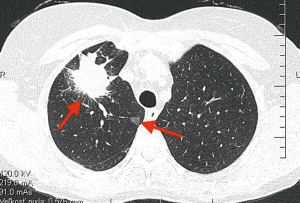
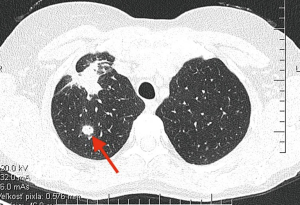
- Patient presented with a large spiculated mass in the RUL with satellite nodule and a GGO in the same lobe and mediastinal lymphadenopathy (Figures 5,6);
- No definitive histology was obtained by bronchoscopy;
- Negative previous oncologic history;
- Positive smoking history.
Case no. 2
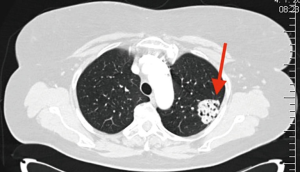
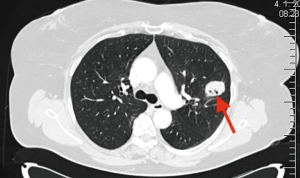
- Patient presented with two tumorous masses in the LUL (Figures 7,8);
- Previous oncologic disease—endometrial carcinoma;
- Negative smoking history;
- Suspected metastatic lesions.
Procedures
The patient is placed in a lateral decubitus position with support under the chest. Two surgeons are requested, in case of upper lobectomy, the camera man stands opposite to the operating surgeon, while the operating surgeon stands in front of the patient. We use a 30 degree scope. Standard incision in the fifth intercostal space is made approximately in middle axillary line depending on the patients constitution. In case no.1 huge lymphadenopathy was present and it was challenging to perform radical resection. Advanced instrumentation was required not to harm the lymphonodes and remove them en-bloc. Powered vascular stapler was used to transect vessels and mechanical endostapler was used for the bronchus. Both procedures were perfectly completed. We started to implement ERAS program, so the patients were verticalised 4 hours after the procedure, with their chest tubes removed the next day and they were discharged day two after the operation (Figure 9—uniportal VATS right upper lobectomy, Figure 10—uniportal VATS left upper lobectomy).


Discussion
We started with VATS lobectomies pretty late in Slovakia. But in short time we were able to accelerate the program and we have improved the necessary skills. More than 50% of all lung resections are performed in minimally invasive way, both uniportal and two portal. We operate on patients also after induction chemotherapy, with centrally localised tumors. Nowadays we plan to extend the spectrum of the procedures with advanced procedures like sleeve lobectomy and double sleeve lobectomy. We have also completed several subxiphoid uniportal VATS lobectomies, but longer instruments are needed, so this procedure was temporarily ceased. After we obtain the proper instrumentarium we plan to proceed. We also plan to organize this type of event in our institution on regular basis together with Diego Gonzalez, as he promised, with the aim to spread the procedure in our country (Figure 11).
We also started the educational program to teach young surgeons the procedure. The training program is based on participating in similar procedures, followed by performing simple antireflux procedures and focusing on teaching particular phases of VATS lobectomy.
VATS lobectomy seems to be a golden standard in surgical treatment of lung cancer in selected patients (4-7).
Acknowledgements
This event was supported by Johnson and Johnson co.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ng CS, Gonzalez-Rivas D, D'Amico TA, et al. Uniportal VATS-a new era in lung cancer surgery. J Thorac Dis 2015;7:1489-91. [PubMed]
- Janik M, Juhos P. Uniportal VATS right upper lobectomy. Asvide 2018;5:413. Available online: http://www.asvide.com/article/view/24379
- Janik M, Juhos P. Uniportal VATS right upper lobectomy. Asvide 2018;5:414. Available online: http://www.asvide.com/article/view/24380
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Aragón J, Pérez Méndez I. From open surgery to uniportal VATS: asturias experience. J Thorac Dis 2014;6:S644-9. [PubMed]
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [PubMed]
- Hartwig MG, D'Amico TA. Thoracoscopic lobectomy: the gold standard for early-stage lung cancer? Ann Thorac Surg 2010;89:S2098-101. [Crossref] [PubMed]
Cite this article as: Janik M, Juhos P. Uniportal VATS lobectomies—masterclass in Bratislava. J Vis Surg 2018;4:78.