Thoracoscopic pulmonary combined with right S1a + S2a subsegmentectomy for deep intersegmental nodule surgery
Introduction
With the development of high resolution computerized tomography (HRCT) and low-dose helical CT, the rate of detection of early stage lung cancer is rising (1). Intentional segmentectomy for early stage lung cancer has been widely developed (2-4). Various medical centers have confirmed the excellent prognosis of intentional segmentectomy for treating early stage lung cancer, in particular adenocarcinoma in situ (AIS) and minimally invasive adenocarcinoma (MIA) (5,6). Due to the complicated anatomical variations of segmental bronchi and vessels, thoracoscopic segmentectomy is technically much more demanding than lobectomy.
Our medical center began initiating thoracoscopic segmentectomy since 2010, and took the lead in using preoperative three-dimensional computed tomography bronchography and angiography (3D-CTBA) for surgery planning in China. Preoperative 3D-CTBA reveals the anatomical structures and variations of the segmental bronchi and vessels, in addition to segmental anatomic relationships of the nodule. With the use of preoperative 3D-CTBA, we found several lesions located at the intersegmental plane and in proximity to the intersegmental vein (named intersegmental nodule). In order to resect these kinds of nodules and ensure a safe margin, traditional segmentectomy had to expend resection (7). This could lead to injury of the intersegmental vein and the loss of lung parenchyma. Our center developed a new method, termed “combined subsegmentectomy”, to resect the intersegmental nodule. This paper presents a case in which a combined subsegmentectomy in the right S1a + S2a was performed to treat early stage lung cancer.
Patient and work up
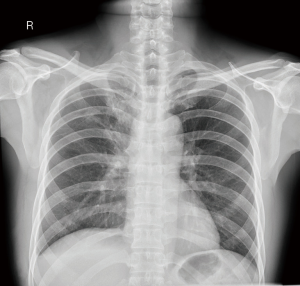
A 55-year-old man with no history of smoking was admitted to our hospital diagnosed with a mixed ground-glass nodule (GGN). CT defined a 1.7×1.27×1.86 cm nodule with mixed ground-glass opacity between the right apical (S1) and dorsal (S2) segment. There was no significant enlargement of the hilar and mediastinal lymph nodes (bilaterally) (Figure 1).
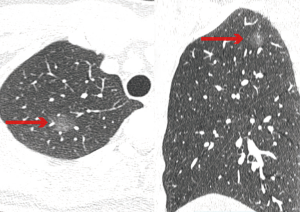
We performed 3D-CTBA reconstruction on the patient using the softwares Osirix and DeepInsight prior the surgery (Figure 2). An 18-mm nodule was located between the right S1a and S2a in proximity to the intersegmental vein (V2a).

The anatomical configuration of the segmental bronchus, artery, and vein are presented in figure (Figure 2) and can be summarized as follows; the bronchus branches into the apicoposterior segmental bronchus (B1+2) and the anterior segmental bronchus (B3). The apical (A1) and the posterior (A2) segment arteries share the common truncus; A2 branches into the dorsal subsegmental arteries (A2a), and the horizontal subsegmental arteries branches (A2b1, A2b2). A1 branches into the apical subsegmental artery branches (A1a1, A1a2) and the ventral subsegmental arteries (A1b). V2a drains blood from S1a and S2a.
As the nodule was located between the S1a and S2a approaching V2a, we intended to resect the right S1a + S2a subsegmentectomy for sufficient margin. The bronchi of B1a and B2a were required to be resected. Furthermore, arteries of A1a1 + A1a2, A2a, and V2a had to be resected.
Surgery (Figure 3)

Three-port thoracoscopic right S1a + S2a subsegmentectomy was performed with the patient under general anesthesia under single-lung ventilation. After dissecting the posterior mediastinum pleura, we sampled the subcarinal lymph nodes and exposed peripherally the right upper lobar bronchus to reveal A2a and A2b2. Subsequently, we dissected the anterior mediastinum pleura and exposed peripherally the truncus of A1 + A2. A2 was exposed, which facilitated the identification of A2a and A2b1 later on. Then, A2a was dissected. We exposed A1 to identify A1a1, A1a2, and A1b. A1a1 and A1a2 were cut to expose B1a and B1b, following which dissecting B1a was required. The distal of A2a stump was exposed peripherally to identify B2a, which was dissected afterwards. Lastly, we dissociated the distal stump of B2a to expose V2a to be dissected.
The intersubsegmental plane was identified by the inflated-deflated line and was separated with electrocautery and endoscopic staplers. We sampled the hilar, paratracheal, and tracheobronchial lymph nodes and was identified as MIA. Total surgical time was about 150 min, with about 20 mL of blood loss.
Postoperative management
The postoperative course was uneventful. A chest drain was removed in POD2 (postoperative 2 days), and the patient was discharged in POD 4. Postoperative radiographic X-ray showed the expanded pulmonary without residual air or fluid (Figure 4). The final diagnosis was T1aN0M0 adenocarcinoma. There was no lymph nodule metastasis.
Discussion
Thoracoscopic pulmonary segmentectomy can preserve lung function and reduce postoperative complications (9). Multi-center research studies have shown that segmentectomy showed equal oncologic outcomes as lobectomy in deep early stage lung cancer (2-4). Therefore, intentional pulmonary segmentectomy has become a widely used treatment for early stage non-small cell lung cancer (NSCLC), notably GGO predominant lesions (10). Due to the complicated anatomical variations of segmental bronchus and vessels, there are still technical and anatomical pitfalls that must be overcome to achieve a safe and precise segmentectomy.
Recently, several studies have confirmed the value of the reconstruction of 3D-CTBA (11-13). Preoperative 3D-CTBA reconstruction is helpful for surgery planning, as it details, nodule location, identification of targeted vessels, bronchus, surgical margins, anatomical variations, simulating safe margins, and planning of surgical approach. In our medical center, reconstruction of 3D-CTBA has become a necessary and routine procedure before segmentectomy. The advantage is that surgeons better understand the pulmonary anatomy of each patient before and during surgical procedures, thus reducing the risk of operation and shortening surgery times.
With the assistance of pre-operative 3D-CTBA, we found lesions located at the intersegmental plane and in proximity to the intersegmental vein, which we termed, intersegmental nodule. Single segmentectomy could lead to insufficient margin, which increases the risk of local recurrence (14,15). The problem with the extended segmentectomy is that it could damage lung function. Our medical team devised a new method to prevent such occurrence. This was performed by resecting the lesion and combining subsegments around the intersegmental nodule. In this report, the tumor was located between S1a and S2a in proximity to V2a, and extended segmentectomy resected S2 and S1a. The combined subsegmentectomy right S1a + S2a reduced the loss of S2b.
Conclusions
In this report we describe a patient with intersegmental nodule that was treated using the combined subsegmentectomy right S1a + S2a. This preserved more lung function and ensured sufficient margin, which led to a good prognosis. Thus the combined subsegmentectomy is an effective technique to treat intersegmental nodules.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.06.10). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patz EF Jr, Goodman PC, Bepler G. Screening for lung cancer. N Engl J Med 2000;343:1627-33. [Crossref] [PubMed]
- Okada M, Yoshikawa K, Hatta T, et al. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg 2001;71:956-60; discussion 961. [Crossref] [PubMed]
- Kodama K, Higashiyama M, Okami J, et al. Oncologic Outcomes of Segmentectomy Versus Lobectomy for Clinical T1a N0 M0 Non-Small Cell Lung Cancer. Annals of Thoracic Surgery 2016;101:504-11. [Crossref] [PubMed]
- Koike T, Kitahara A, Sato S, et al. Lobectomy Versus Segmentectomy in Radiologically Pure Solid Small-Sized Non-Small Cell Lung Cancer. Ann Thorac Surg 2016;101:1354-60. [Crossref] [PubMed]
- Yanagawa N, Shiono S, Abiko M, et al. The correlation of the International Association for the Study of Lung Cancer (IASLC)/American Thoracic Society (ATS)/European Respiratory Society (ERS) classification with prognosis and EGFR mutation in lung adenocarcinoma. Ann Thorac Surg 2014;98:453-8. [Crossref] [PubMed]
- Yoshizawa A, Motoi N, Riely GJ, et al. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 2011;24:653-64. [Crossref] [PubMed]
- Okada M. Radical segmentectomy. Nihon Geka Gakkai Zasshi 2014;115:137-42. [PubMed]
- Xu XF, Chen L, Wen W, et al. Combined right S1a + S2a subsegmentectomy. Asvide 2018;5:597. Available online: http://www.asvide.com/article/view/25646
- Keenan RJ, Landreneau RJ, Maley RH Jr, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 2004;78:228-33; discussion 228-33. [Crossref] [PubMed]
- Yoshida J, Nagai K, Yokose T, et al. Limited resection trial for pulmonary ground-glass opacity nodules: fifty-case experience. J Thorac Cardiovasc Surg 2005;129:991-6. [Crossref] [PubMed]
- Wu WB, Xu XF, Wen W, et al. Three-dimensional computed tomography bronchography and angiography in the preoperative evaluation of thoracoscopic segmentectomy and subsegmentectomy. J Thorac Dis 2016;8:S710-5. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Wu WB, Xu XF, Wen W, et al. Thoracoscopic Pulmonary Sub-Subsegmentectomy Based on Three-Dimensional Images. Ann Thorac Surg 2016;102:e389-91. [Crossref] [PubMed]
- Mohiuddin K, Haneuse S, Sofer T, et al. Relationship between margin distance and local recurrence among patients undergoing wedge resection for small (</=2 cm) non-small cell lung cancer. J Thorac Cardiovasc Surg 2014;147:1169-75; discussion 1175-7. [Crossref] [PubMed]
- Khullar OV, Liu Y, Gillespie T, et al. Survival After Sublobar Resection versus Lobectomy for Clinical Stage IA Lung Cancer: An Analysis from the National Cancer Data Base. J Thorac Oncol 2015;10:1625-33. [Crossref] [PubMed]
Cite this article as: Xu XF, Chen L, Wen W, Wu WB, Zhu Q. Thoracoscopic pulmonary combined with right S1a + S2a subsegmentectomy for deep intersegmental nodule surgery. J Vis Surg 2018;4:131.