Technical aspects of laparoscopic non-anatomical left lateral sectionectomy of the liver
Case presentation
The patient is a 59-year-old man without chronic hepatitis B/C or other hepatic disease. One hepatic tumor in left liver was found in ultrasonography at regular physical examination. Further CT scan showed one 2 cm irregular hypodense tumor on the surface of segment 3 with rim-enhancement in arterial phase and without washout in portal venous phase. Alpha-fetoprotein is within normal limit. But the possibility of malignancy cannot be excluded by clinical imaging. Therefore, he underwent laparoscopic non-anatomical left lateral sectionectomy (partial segment 2 and 3). The pathology result is necrotic nodule with granuloma formation. He was discharged on post-operative day 7 without any adverse event (Figure 1).

General principles
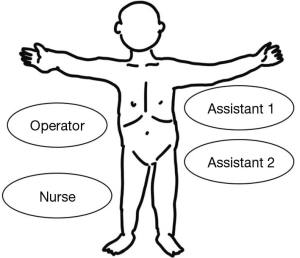
The patient was placed on reverse Trendelenburg position. The operator stood on patient’s right side and assistants stood on the opposite side (Figure 2). Pneumoperitoneum was created with pressure between 10 to 12 mmHg.
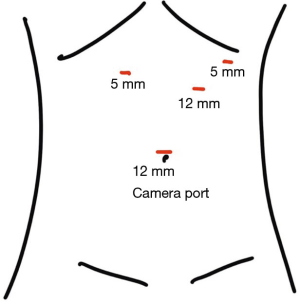
We utilized 10 mm 30-degree angle HD laparoscope. Two 12 mm ports and two 5 mm ports were placed as demonstrated (Figure 3). Intraoperative ultrasonography was used to identify tumor’s location and its relationship with adjacent Glissonean pedicle.
Dissection of hepatoduodenal ligament (HDL) started from left border of HDL. Hepatic artery into segment 2 and 3 (A2+3) in this patient was dissected and looped with vascular tape. Following that, test clamping on A2+3 demonstrated the demarcation line between left lateral section and left medial section.
Liver parenchyma transection started along the demarcation line by using Cavitron Ultrasonic Surgical Aspirator (CUSA, Integra LifeSciences Corp., New Jersey, USA), Harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH, USA), and bipolar electrocautery alternatively. We used Hem-o-lok clip (Weck Closure Systems, Research Triangle Park, NC, USA) or metallic clips for vascular ligation according to the diameter of vessels.
At last steps, left hepatic vein was divided with accompanied with some liver parenchyma by laparoscopic linear stapler (Ethicon Endo-Surgery, Cincinnati, OH, USA). The specimen was removed out from umbilical port wound.
Special technical steps
- To decrease blood loss, encircling HDL before liver parenchymal transection and employing inflow control with Pringle maneuver can prevent annoying massive haemorrhage during liver parenchyma transection (2). But we did not perform Pringle maneuver in this patient.
- Hemorrhage may occur when we divided liver parenchyma near the root of left hepatic vein. Reverse Trendelenburg position with head elevated about 15 to 30 degrees may reduce central venous pressure (CVP) level and reduce blood loss from hepatic veins. Other methods to reduce CVP by anesthesiologists also play an important role in hemorrhage control (3). The bloodless operation field is the key to smooth laparoscopic liver surgery.
- Always keep good exposure of target is very important. The direction of traction by assistants should change frequently according to the extent of liver parenchymal transection. Poor exposure of target will lead to wrong way and unnecessary blood loss.
- Precise analysis of anatomy in HDL and hepatic hilum from preoperative CT scan or 3D simulation software can identify abnormal anatomy and avoid inappropriate decision during operation especially for the trainees (4).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.07.19). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang PC, Ho CM, Hu RH. Technical aspects of laparoscopic non-anatomical left lateral sectionectomy of the liver. Asvide 2018;5:667. Available online: http://www.asvide.com/article/view/26337
- Tranchart H, O’Rourke N, Van Dam R, et al. Bleeding control during laparoscopic liver resection: a review of literature. J Hepatobiliary Pancreat Sci 2015;22:371-8. [Crossref] [PubMed]
- Kobayashi S, Honda G, Kurata M, et al. An experimental study on the relationship among airway pressure, pneumoperitoneum pressure, and central venous pressure in pure laparoscopic hepatectomy. Ann Surg 2016;263:1159-63. [Crossref] [PubMed]
- Ho CM, Wakabayashi G, Yeh CC, et al. Comprehensive evaluation of liver resection procedures: surgical mind development through cognitive task analysis. J Vis Surg 2018;4:21. [Crossref] [PubMed]
Cite this article as: Yang PC, Ho CM, Hu RH. Technical aspects of laparoscopic non-anatomical left lateral sectionectomy of the liver. J Vis Surg 2018;4:163.