Uniportal video-assisted thoracoscopic surgery segmentectomy
The case for lobectomy
Lobectomy was established as the standard of care for lung cancer resection since Dr. Ginsberg published his landmark article in 1995 (1). Limitations of this study include the small sample size of about 120 patients in each arm, and the combining of wedge resection and segmental resection into a single category of limited resection. Since then, many studies have been performed to show the role of segmentectomy as a definitive treatment for lung cancer in selected patient populations.
Multiple primary lung cancer (MPLC)
The disease pattern of lung cancer is changing. Adenocarcinomas are becoming more common, and lung cancer incidence is rapidly rising in non-smokers. In Asia, we are seeing more frequently patients with MPLC who are never-smokers. A case in point was a 69-year-old gentleman who had coronary artery disease and was found to have a 1.6 cm ground glass opacity (GGO) with solid component in the right lower lobe. There were also multiple other GGOs in the lung bilaterally of various sizes (Figure 1). This patient underwent coronary artery bypass surgery followed by uniportal video-assisted thoracoscopic surgery (UVATS) lobectomy of the right lower lobe. Multiple other GGOs in the right lung were also resected concurrently. He was found to have a total of nine separate primary lung adenocarcinomas ranging in size from 1 to 16 mm (Figure 2). These were all completely resected and the patient has no recurrence or progression at 2-year follow up.
The case for segmentectomy
It is clear that early resection of lung cancer offers a survival advantage; with worsening survival as the lung cancer becomes larger. The increasing prevalence of patients with MPLC illustrates the need for early complete resection of lung cancers while preserving lung. Key considerations for segmentectomy preoperatively, operatively, and postoperatively were summarized (Tables 1-3).
Table 1
| Histology and grade |
| Size and solid component |
| Location—which lobe/segment |
| Lung function |
| Presence of lung diseases such as ILD |
| SUV |
| Age—advanced octogenarians (where 5-year survival is impactful) or young (with many years still ahead for further changes) |
| Multiple comorbidities |
ILD, interstitial lung disease; SUV, standardized uptake value.
Table 2
| Anatomical resection |
Table 3
| Curative resection |
|---|
| Both cancer free survival & overall survival |
| Preserving function and minimizing suffering |
| Full recovery back to normal life |
Case presentations of UVATS segmentectomy
Case 1
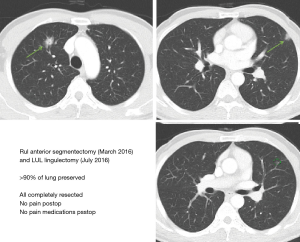
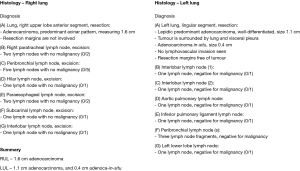
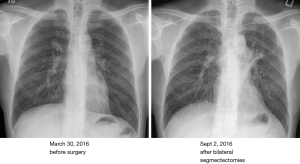
A 53-year-old gentleman who never smoked was found to have a speculated lung mass in the anterior segment of the right upper lobe, and two GGOs in the left lingua (Figure 3). He underwent sequential UVATS right upper lobe anterior segmentectomy followed by UVATS left upper lobe lingulectomy. Complete mediastinal nodal dissection was performed each time. Ninety percent of his lung volume was preserved. Histology showed 1.6 cm adenocarcinoma in the RUL anterior segment, and a 1.1 cm adenocarcinoma and a 0.4 cm adenocarcinoma in situ (AIS) in the lingula (Figure 4). All lesions were completely resected and chest radiograph showed well expanded lung fields bilaterally (Figure 5).
Case 2
A 68-year-old lady who has never smoked with past medical history of diabetes, hypertension, hyperlipidemia, sick sinus syndrome with pacemaker was found to have two lung nodules in the left upper lobe and a GGO in the anterolateral basal segment of the right lower lobe (Figure 6). She underwent UVATS left upper lobectomy followed by UVATS right lower lobe anterolateral basal segmentectomy. Complete mediastinal nodal dissection was performed during each operation. The upper lobe nodules were found to be two separate primaries (2.1 cm lepidic and papillary adenocarcinoma, and 0.8 cm mucinous adenocarcinoma), and the right lower lobe nodule in the anterolateral basal segment was found to be a 1.7 cm non-mucinous AIS. There were no nodal metastasis and all tumors were completely resected (Figure 7).


Case 3
A 79-year-old gentleman was found to have a 3.3 cm mass in the posterior segment of the right lower lobe. PET scan showed mild avidity with SUV 3.2 (Figure 8). He underwent UVATS right upper lobe posterior segmentectomy and mediastinal nodal dissection. Histology showed a 3.3 cm typical carcinoid tumor with mitotic activity less than 1 per 2 mm2. All nodes were negative and the tumor was completely resected.

Conclusions
UVATS segmentectomy with true anatomical dissection and complete nodal dissection may be considered for:
- Lesions ≤2 cm for adenocarcinoma, minimally invasive adenocarcinoma (MIA), AIS;
- Especially for lesions with lepidic pattern, low SUV (<3.3), or low-grade neoplasm such as typical carcinoid tumor;
- No known nodal metastasis (cN0);
- Patients with multiple lung lesions who may require multiple resections now or in the future;
- Especially for patients with advanced age, poor/borderline lung function, or multiple comorbidities;
- In properly selected patients, UVATS segmentectomy allows the achievement of complete resection with good anatomical margin, full pathological staging, and lung parenchymal sparing resulting in full and early functional recovery.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jose Luis Danguilan) for the series “Dedicated to the 6th Asian Single-port VATS Symposium 2018” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.07.23). The series “Dedicated to the 6th Asian Single-port VATS Symposium 2018” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
Cite this article as: Tam JKC. Uniportal video-assisted thoracoscopic surgery segmentectomy. J Vis Surg 2018;4:167.