Non-intubated uniportal video-assisted thoracoscopic surgery-lobectomy in Germany—the first 2 cases
Introduction
Since being first introduced into clinical practice in the early 90ies (1), minimally-invasive anatomical lung resection has gained widespread acceptance both nationally and internationally, and is increasingly considered gold standard for treatment of early-stage lung cancer (2,3).
Technical progress with continuously improving optical devices (up to 4K resolution for 5 mm 30° cameras), and ever developing thoracoscopic tools allow to routinely perform even extensive oncologic resections in a minimally-invasive approach (4-6). Additionally, live-surgery videos available through dedicated online-platforms and a broad offering of video-assisted thoracoscopic surgery (VATS)-courses help in spreading knowledge of minimally-invasive techniques. Currently most centers still perform VATS-lobectomies in a so-called “triportal technique”, which we already described several years ago (7). The most important innovation of these past years was the adoption of a uniportal approach for anatomical lung resections by Diego Gonzales Rivas (8), in which the 2 caudally placed incisions can be omitted. This technique allows to perform even complex procedures, including anatomical segmentectomies, pneumonectomies, carinal resections, angioplastic and bronchoplastic lobectomies or thymectomies, by just a single incision of 2–3 cm. Reported advantages of this approach include a further reduced operative trauma, less postoperative pain, better cosmetics whilst maintaining excellent oncological resection quality (9).
At the same time it is possible to altogether forego orotracheal intubation in selected patients with reduced pulmonary function to perform an anatomical lung resection under spontaneous breathing (10). This approach obviates classical drawbacks of mechanical ventilation as secretion of pro-inflammatory cytokines, induction of mechanical damage on alveolar level by barotrauma and atelectasis of the dependent lung after muscle relaxation (10,11).
In our experience this approach should be restricted to specialized surgeons well trained in minimally-invasive surgery. Avoidance of orotracheal intubation may lead to uncontrolled patient movement, coughing, mediastinal shift or marked diaphragmatic excursion, thus being extremely challenging for surgeons and anesthetists alike, especially when emergent conversion to thoracotomy is required.
We would like to report on the 2 first non-intubated uniportal lobectomies for NSCLC in Germany performed by Dr. Rivas in June 2018.
Patient selection
Our first patient was a 77-year-old female admitted for resection of an adenocarcinoma of the right upper lobe. She had a history of coronary artery disease with diastolic dysfunction, low-grade mitral stenosis, atrial fibrillation with running phenprocoumon treatment and implantation of a biological aortic valve (valve-in-valve TAVI) 1 year prior to admission.
Our second patient was a 77-year-old female as well, who was admitted for resection of a low-grade neuroendocrine tumor of the middle lobe. She had a history of breast cancer with amputation of the right breast, a monoclonal gammopathy and atrial fibrillation with running phenprocoumon treatment.
Both had a slightly impaired respiratory function, a BMI <25 and were in overall good health.
Technique (Figures 1,2)

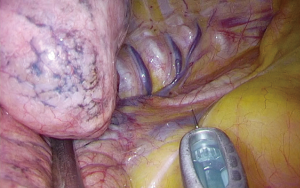
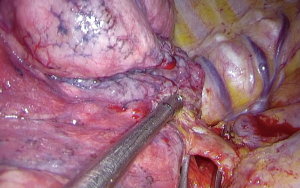
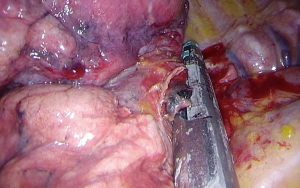
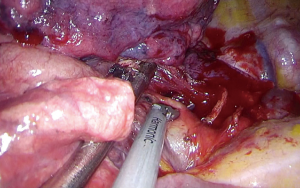
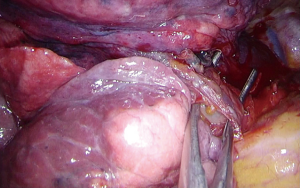
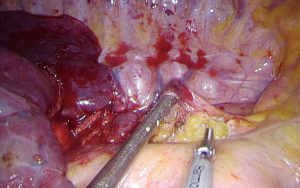
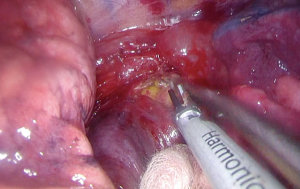
Our initial concept included constant inhalation with lidocaine (starting 30 min, prior to surgery, 1%—solution with an O2—flow of 6l), thoracic epidural catheter placement (thor. 6–7, initial bolus hyperbaric bupivacaine 0.5%, 5 mL, followed by ropivacaine 2 mg/mL, continuous flow rate 12–28 mg/h) as well as a local incisional infiltration (ropivacaine 7.5 mg/mL, 10 mL). Standard anesthesiological instrumentation (two venous lines 18G/16G), vital sign monitoring (ECG, pulsoxymetry, NIBP) and respiratory gas monitoring were initiated before patients were placed on a bean bag in lateral decubitus position. Under spontaneous breathing via laryngeal mask with additional suction option and continuous titration of sufentanil and propofol, a 3-cm long incision at the level of the 4th intercostal space was made and a 10-mm 30° scope was inserted into the chest through an Alexis-Retractor. To avoid coughing during the procedure, a selective paratracheal vagal blockade with 5 mL ropivacaine 7.5 mg/mL was made (Figure 3). In case of a right upper lobe resection the further steps don’t differ from our standard approach, and consist in initial dissection of the anterior hilum to expose the anterior trunk of the pulmonary artery (PA) (Figure 4). Vessel loops aren’t usually required as these branches can easily be passed with a standard stapling device. Underneath, the upper lobe bronchus can be readily identified thanks to lymph nodes often located on the proximal intermediate bronchus, and transected with a stapler in the same fashion (Figure 5). Now the posterior ascending branch of the PA (Figure 6) and the upper lobe vein (after isolating the portion draining the middle lobe, Figure 7) are identified and stapled in rapid succession. After completing the fissure and removing the lobe with a retrieval bag, lymph node dissection is feasible in the same way as usual (Figure 8), even though removing infracarinal nodes in spontaneous breathing patients without muscle relaxation is challenging (Figure 9).
Shortly after the procedure both patients were transferred to our observation unit before reaching our routine ward on the same evening.
Comments
Non-intubated major lung resection appears to be feasible if certain rules are respected. First of all patient selection is key. Especially obese patients and those with difficult airways should be ruled out at priori. Frail, elderly patients are likely to benefit most from avoidance of mechanical ventilation, and should thus be included preferentially. Then it is recommended to start a non-intubated program only in centers with a high degree of surgical and anesthesiological expertise. Only expert VATS surgeons comfortable in management of severe complications like major bleeding, and prepared to deal with potentially moving and coughing patients, should put their sights on non-intubated surgery. Furthermore good perioperative management is mandatory. Only if an overarching strategy, including preoperative inhalation with lidocaine, intraoperative analgesia and postoperative multidisciplinary pain management, is established, non-intubated procedures can be approached with confidence. Only after fulfilling all these prerequisites and gathering experience with smaller non-intubated procedures, an expert proctor should be contacted. Dr. Rivas kindly performed the first 2 non-intubated lobectomies at our institution and convinced us of the advantages of non-intubated lung surgery. Both patients did extremely well and were discharged after a few days.
Acknowledgments
We would like to acknowledge Johnson & Johnson for their financial support in this endeavour and Anna Junge for taking pictures and Marco Küster for his help during both procedures.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Teaching Uniportal VATS”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.07.18). The series “Teaching Uniportal VATS” was commissioned by the editorial office without any funding or sponsorship. DGR served as the unpaid Guest Editor of the series and serves as an unpaid associate editor-in-chief of Journal of Visualized Surgery. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lewis RJ, Caccavale RJ, Sisler GE, et al. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg 1992;104:1679-85; discussion 1685-7.
- Falcoz PE, Puyraveau M, Thomas PA, et al. Video-assisted thoracoscopic surgery versus open lobectomy for primary non-small-cell lung cancer: a propensity-matched analysis of outcome from the European Society of Thoracic Surgeon database. Eur J Cardiothorac Surg 2016;49:602-9. [Crossref] [PubMed]
- Yang CJ, Kumar A, Klapper JA, et al. A National Analysis of Long-term Survival Following Thoracoscopic Versus Open Lobectomy for Stage I Non-small-cell Lung Cancer. Ann Surg 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Ismail M, Swierzy M, Nachira D, et al. Uniportal video-assisted thoracic surgery for major lung resections: pitfalls, tips and tricks. J Thorac Dis 2017;9:885-97. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49:i6-16. [PubMed]
- Zardo P, Weidener C, Fischer S. Expertentechniken in der Thoraxchirurgie. VATS-Lobektomie. Z Herz- Thorax- Gefäßchir 2011;25:73.
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Gonzalez-Rivas D, Aymerich H, Bonome C, et al. From Open Operations to Nonintubated Uniportal Video-Assisted Thoracoscopic Lobectomy: Minimizing the Trauma to the Patient. Ann Thorac Surg 2015;100:2003-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Schilling T, Kozian A, Huth C, et al. The pulmonary immune effects of mechanical ventilation in patients undergoing thoracic surgery. Anesth Analg 2005;101:957-65. table of contents. [Crossref] [PubMed]
- Zardo P, Zinne N, Logemann F, et al. Non-intubated uniportal lobectomy of the right upper lobe with radical lymphadenectomy part 1. Asvide 2018;5:700. Available online: http://www.asvide.com/article/view/26573
- Zardo P, Zinne N, Logemann F, et al. Non-intubated uniportal lobectomy of the right upper lobe with radical lymphadenectomy part 2. Asvide 2018;5:701. Available online: http://www.asvide.com/article/view/26574
Cite this article as: Zardo P, Zinne N, Logemann F, Gras C, Rivas DG. Non-intubated uniportal video-assisted thoracoscopic surgery-lobectomy in Germany—the first 2 cases. J Vis Surg 2018;4:178.