Thoracoscopic S8 segmentectomy
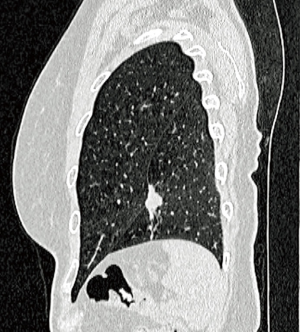
S8 segmentectomies are indicated for some cT1a non-small cell lung cancers (NSCLCs) for patients who had undergone a previous major pulmonary resection and/or have a compromised pulmonary function and/or who present with two synchronous or metachronous tumors. It can also be proposed for some solitary metastases (Figure 1).
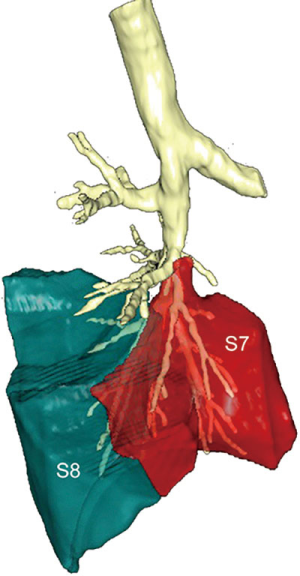
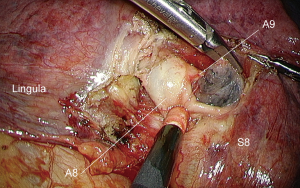
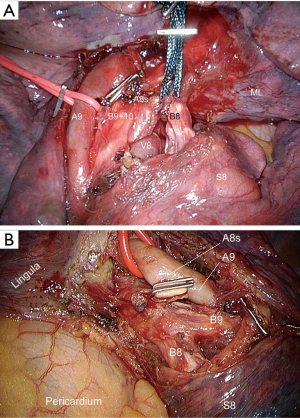
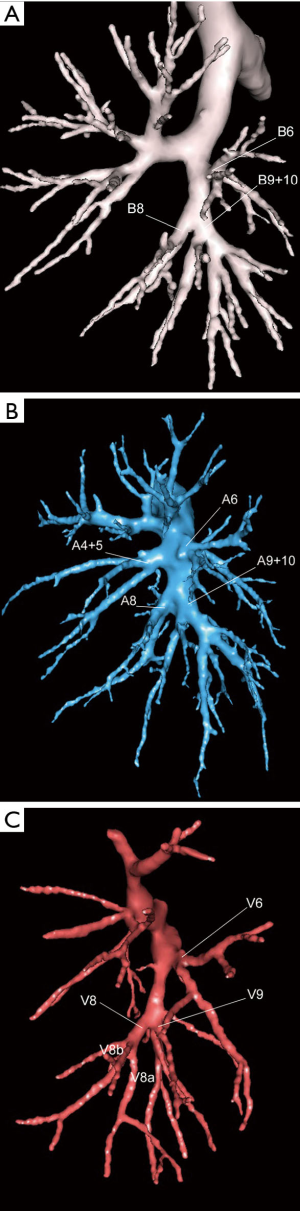
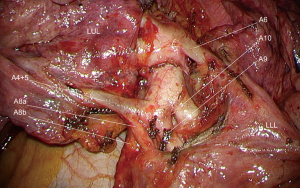
S8 segmentectomies are slightly easier on left side compared to right one because there is no S7 segment (Figure 2). Variations in the distribution of arteries and bronchi require a thorough examination of preoperative modelisation. In this article, we will base on the most frequent anatomical pattern, that is A8 and a A9+10 common arterial trunk with the corresponding B8 and B9+10 bronchi (Figure 3).
Anatomical landmarks
In most cases, the basilar arterial trunk branches in two arteries: A8 and A9+10 (1). This pattern is more frequent on the right side (90%) than on the left side (74%). In a minority of patients, the anatomy is reverse with the following distribution: A8+9 and A10 (8% on the right side and 16% on the left side) (Figure 4). On the left side all three arteries can be independent (10%) (1). All arteries to the lower lobe must be clearly identified in order to avoid misidentification, such as a low A8a being mistaken for an A9+10. When in doubt during dissection, it is advisable to control only the anterior branch of A8 (A8b), then the bronchus and eventually check the direction of the second branch. An important variation deserves to be known: on the right, A7 is lacking in 16% of the patients, explaining why A7 is sometimes not found, even after an extensive dissection of the PA branches. When present, it is discovered on the posterior aspect of the arterial basilar trunk at a variable level between the onset of the middle lobe artery and the basilar arteries (Figure 5).
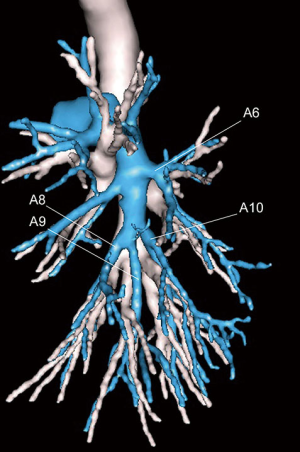
The basilar bronchial trunk usually separates in two branches: B8 and B9+10 which lie posterior to the segmental arteries. As for arteries, instead of a common B9+10 trunk, B9 can have a common birth with B8 (Figure 4).
The venous drainage is highly variable. The superior basal vein (SBV), which is the middle root of the IPV, does seldom represent the venous drainage of segment 8. Its posterior branch can drain segment 9 (Figure 3C). Actually, in most cases (88%), the inferior pulmonary vein has two tributaries: a V6 and a common basilar vein. If is thus safer to control the vein within the parenchyma and divide only the anterior branch of the vein (V8b) which runs immediately behind the bronchus, rather than controlling V8 centrally in the inferior pulmonary vein.
Surgical technique
The basic principles of our technique have been described (2), as well as the need for preoperative modelisation (3).
Opening the fissure and controlling the artery
This step is similar to the dissection of the fissure during a lower lobectomy or a basilar segmentectomy. But the dissection of arteries must be pursued as low as possible and all branches to the lower lobe must be clearly identified.
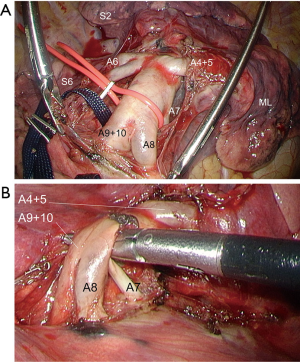
Both A8 and A9+10 are looped (Figure 6), so that one can retract them forward or backward to expose B8. Dissection must be pursued on a sufficient length to detect any anatomical variation such as a lingular artery raising from A8 (Figure 7). A8 is clipped. All lymph nodes located in the arterial division must be dissected, removed and sent for frozen section (Figure 8). If invaded, the procedure should be extended, either to a basilar segmentectomy or even a lower lobectomy in patients operated for NSCLC.
On the right side, a middle lobe artery can raise from A8 and similarly on the left side a lingular artery can raise from A8. This stresses the need for an extensive dissection of all arterial branches in the fissure (Figure 9).

Dissecting and controlling the bronchus
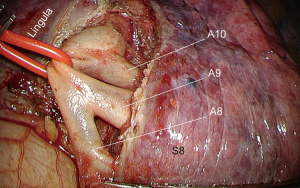
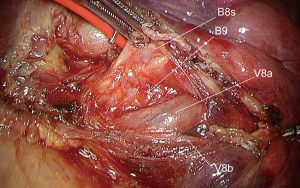
By retracting B9+10 backward, B8 is exposed (Figure 10). It is carefully dissected to avoid any tear of the vein (V8a) that runs just behind it. It is then stapled after a reventilation test.
Dissecting and controlling the vein
There is no need to dissect the inferior pulmonary vein (1,5). Once the bronchus has been stapled, its stump is gently lifted up and its backside is denuded with caution to expose the anterior branch of the vein (V8b). Its posterior branch (V8a), that partially drains S9, is preserved (Figure 11).
Intersegmental plane
The intersegmental plane is determined by systemic injection of indocyanine green (ICG) at the dose of 0.3 mg/kg with fluorescence imaging system (Novadaq™) (6). Cautery dots are made on the parenchyma on this demarcation line, i.e., the plan between S8 and S9.
A long clamp is applied on the parenchyma, following the cautery spots that have been applied. It is checked that the bronchial stump stays remote and will not get stuck within the stapler jaws. The conic shape of S8 can make precise application of the stapler difficult with a risk of plication of the parenchyma. Thanks to use of two grasping forceps, the parenchyma can be stretched to expose the whole segment 8 and ease stapling.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alessandro Brunelli) for the series “Uncommon Segmentectomies” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The series “Uncommon Segmentectomies” was commissioned by the editorial office without any funding or sponsorship. DG is consultant for an instrument manufacturer (Delacroix Chevalier). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nomori H, Okada M. Illustrated anatomical Segmentectomy for Lung Cancer. Tokyo: Springer-Verlag, 2012.
- Gossot D. Atlas of endoscopic major pulmonary resections - 2nd edition. Springer-Verlag, 2018:180.
- Yang Q, Xie B, Hu M, et al. Thoracoscopic anatomic pulmonary segmentectomy: a 3-dimensional guided imaging system for lung operations. Interact Cardiovasc Thorac Surg 2016;23:183-9. [Crossref] [PubMed]
- Seguin-Givelet A, Brian E, Grigoroiu M, et al. Dissection of A8 artery arising from the lingular artery. Asvide 2018;5:746. Available online: http://www.asvide.com/article/view/27167
- Miyajima M, Watanabe A, Uehara M, et al. Total thoracoscopic lung segmentectomy of anterior basal segment of the right lower lobe (RS8) for NSCLC stage IA (case report). J Cardiothorac Surg 2011;6:115. [Crossref] [PubMed]
- Guigard S, Triponez F, Bédat B, et al. Usefulness of near-infrared angiography for identifying the intersegmental plane and vascular supply during video-assisted thoracoscopic segmentectomy. Interact Cardiovasc Thorac Surg 2017;25:703-9. [Crossref] [PubMed]
Cite this article as: Seguin-Givelet A, Brian E, Grigoroiu M, Gossot D. Thoracoscopic S8 segmentectomy. J Vis Surg 2018;4:196.