The future of minimally invasive thymectomy: the uniportal subxiphoid video-assisted thoracic surgery technique—a case series
Introduction
Thoracic surgical techniques have evolved significantly over the last two decades. For anterior mediastinal masses, of which thymoma is the most frequent, very often surgical treatment is recommended as the principal management. The gold standard surgical approach to anterior mediastinal masses like thymomas, has been median sternotomy. Nowadays, alternative less invasive surgical techniques are possible thanks to video-assisted thoracoscopic surgery (VATS). Thoracoscopy offers the benefit of reduced postoperative pain allowing for earlier mobilisation which facilitates shorter hospital lengths of stay. It is reported that recovery to normal function is faster and patients experience fewer post-operative complications (1-3).
For thymectomy, cervical and standard lateral thoracic VATS has been described. The cervical approach has not become popular because of the small size of the neck wound (4).
At present, the lateral approach through a thoracoscopic incision is the most common surgical approach; however, it can be challenging to achieve a satisfactory visualisation of the whole thymus from ‘phrenic to phrenic’ and passing through the intercostal space could lead to postoperative acute and chronic pain due to intercostal nerve injuries (4).
Uniportal subxiphoid VATS (SVATS) approach has been proposed to potentially reduce the invasiveness and the surgical stress providing exposure of entire thymus and a bilateral vision of the phrenic nerves. In this technique, a single vertical incision is made in the subxiphoid region, allowing muscle-sparing and avoiding intercostal incisions and intercostal nerve damage (5).
The SVATS technique is becoming established as an alternative thoracoscopic approach increasingly utilised for a range of thoracic surgical procedures including lobectomies, segmentectomies, pneumonectomy (6-12). Here we present our case series of SVATS thymectomy demonstrating that this technique should be considered as an alternative approach to anterior mediastinal masses.
Methods
The reported surgeries were performed in Shanghai Pulmonary Hospital, Shanghai, China, between October 2014 and January 2018.
Patient demographics, intraoperative and postoperative data were collected from patients notes and electronic records. The following are considered contraindications to SVATS:
- stage 3–4 thymic tumours;
- body mass index >30 kg/m2;
- impaired ventricular function and/or cardiomegaly;
- severe arrhythmia.
Surgical technique
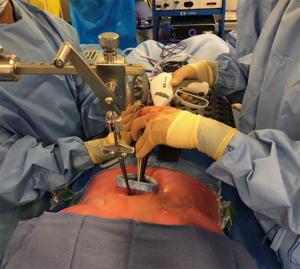
Our technique for SVATS thymectomy has been previously described (8). In summary: the operation is performed with the patient positioned supine on the operating table ventilated through a double lumen tube to permit selective ventilation to facilitate the procedure. Access is through a 4 cm subxiphoid vertical incision and a wound retractor positioned upon entry into the pleural spaces. The xiphoid process can be resected to provide an optimal view if required. The sternum is elevated using a table mounted retractor to maximise the anterior mediastinal operating space (Figure 1). A 10 mm 30o angle thoracoscope (Karl Storz, Tutlingen, Germany) was used. Subxiphoid VATS instruments are used to perform the procedure (Shanghai Medical Instruments Group Ltd, Shanghai, China).
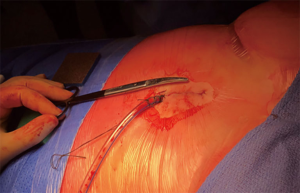
The right pleural cavity is opened initially, with the left lung being selectively ventilated. Electrocautery dissection is used to mobilise the right lobe of the thymus and any pericardial and epiphrenic fat pads, with clear visualisation of the phrenic nerve provided by SVATS. The large neck veins are well visualised using this approach and guide the superior dissection. Subsequently, the left pleural cavity is opened and the thymus dissected from the pericardium in a similar manner. The resected specimen can then be retrieved through the subxiphoid incision (Figure 2).
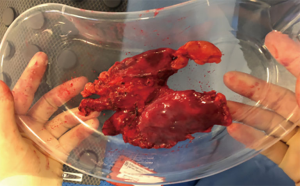
At the end of the procedure, one or two chest drains are placed through the subxiphoid incision (Figure 3). The patients are usually extubated on the operating table.
Data collection
Data was retrieved from a prospectively maintained database with additional data retrieved retrospectively from patient notes and electronic patient records. Data concerning patient demographics, intraoperative details and post-operative course were collected.
Results
Patient characteristics
Over a period of study, 39 SVATS thymectomies were performed for thymic lesions. Patient characteristics are summarised in Table 1. The mean age of patients was 60 years.
Table 1
| Characteristic | Values |
|---|---|
| Sex | |
| Male | 22 |
| Female | 17 |
| Age, mean [range] | 60 [26–80] |
| Smoking | |
| Yes | 13 |
| No | 26 |
| BMI | 24.3 [14.37–32.46] |
| FEV1, L | |
| Actual | 2.33±0.73 |
| % predicted | 88.72±18.68 |
| Albumin, mg/L | 38.79±3.90 |
| Haemoglobin, g/dL | 133.0±13.63 |
| Lesion size, mm | 30 [12–77] |
BMI, body mass index.
Intraoperative details
Intraoperative details are summarised in Table 2. The mean length of surgery was 2 hours with a range of 1–4 hours. Injury to the innominate vein resulted in one patient requiring conversion to thoracotomy in the series. There was a low intra-operative blood loss with a mean loss of 93 mL. Comparing the first 20 cases to the more recent 19 cases, it is evident that there was a significant improvement in terms of reduced operative duration (2.55 vs. 1.68 hours, P=0.005).
Table 2
| Characteristic | Entire cohort | First 20 cases | Last 19 cases | P value |
|---|---|---|---|---|
| Surgical duration (hours) | 2.13±0.98 | 2.55±1.01 | 1.68±0.74 | 0.005 |
| Conversion to thoracotomy | 1 | 1 | 0 | 0.99 |
| Operative blood loss (mL) | 93.33±74.31 | 111.0±92.90 | 74.73±42.86 | 0.21 |
| Drainage in first 24 hours (mL) | 244.21±179.82 | 271.0±183.73 | 214.44±175.70 | 0.39 |
| Postoperative length of stay (days) | 4.33±2.84 | 4.20±1.79 | 4.47±3.68 | 0.64 |
Statistical analysis comparing first 20 and last 19 cases—Mann-Whitney U test.
Postoperative course
One patient’s postoperative course was complicated by a myasthenic crisis. The patient required intubation and respiratory support for 1 week. The patient was discharged on day 9. The median length of hospital stay was 4 days. There were no instances of phrenic nerve palsy. There was no 30-day mortality in this patient series.
Post-operative pathological examination of the resected thymic lesions is summarised in Table 3. Thymic cysts were the commonest pathology observed.
Table 3
| Type | Frequency |
|---|---|
| Thymic cyst | 21 |
| Thymic bronchial cyst | 6 |
| Thymic hyperplasia | 2 |
| Ectopic thyroid tissue | 2 |
| B2 thymoma | 3 |
| AB thymoma | 5 |
Discussion
This report demonstrates that the uniportal subxiphoid VATS approach can be considered as an alternative approach to performing thoracoscopic resection of anterior mediastinal masses. The approach provides excellent visualisation of the entire thymus from phrenic-to-phrenic allowing for radical resection under direct vision, whilst performing a minimally invasive surgery.
In recent years, VATS has been increasingly used as a surgical approach for thymectomy using a lateral approach. While the lateral approach is ideal for lobectomy and tumour resections, performing a total thymectomy via the lateral approach can be challenging. In particular, the lateral approach does not allow a complete vision of the contralateral phrenic nerve (4). However, in comparison to sternotomy there are many advantages reported including reduced intraoperative blood loss, earlier removal of chest drains, reduced requirement for blood products, reduced inflammatory cytokine response, shorter hospital stay and superior cosmetic result (13), without compromising the oncological outcome.
In an attempt to further refine the thoracoscopic technique and improve post-operative outcomes, the SVATS approach has been developed with the advantage of avoiding intercostal incision and manipulation (6-11,14). Since the postoperative chest drains do not enter the thoracic cavity through intercostal spaces postoperatively, they do not impinge on the intercostal neurovascular bundle. This has the potential benefit of allowing early aggressive mobilization which is recognised to be associated with reduced risk of venous thromboembolism and may facilitate a reduction in pulmonary atelectasis and development of lower respiratory tract infections. Together this offers the potential for reduced hospital length of stay (15). To date, there is only one randomised controlled trial comparing SVATS to standard VATS—in patients undergoing bullectomy and pleurectomy. They observed a significant reduction on postoperative pain in the SVATs group which was associated with earlier mobilisation and reduced risk of complication (16).
The SVATS approach is particularly suited to thymectomy as it provides excellent views of the anterior mediastinum as well as of the two pleural spaces including the phrenic nerves. This access and view provide the surgeon the opportunity to perform an oncologically radical and safe resection of the thymus with low risk of injuring the phrenic nerves or other intrathoracic structures. To date there have been a small number of reports of SVATS thymectomy, but our study represents the largest case series to date (7,17-19). One recent series has reported performing robotic SVATS thymectomy (20), highlighting the versatility of the subxiphoid incision. In all of the published series there have been no mortality to date, and the incidence of intraoperative and postoperative complication is very small.
Our case series adds further to the evidence that the uniportal SVATS approach is a safe and appropriate method for thymic resection particularly in non-obese patients with Masaoka stage I tumours and without significant underlying cardiorespiratory disease. In our practice, comparing this case series with our early experience, the surgical duration, operative blood loss, 24-hour drainage and hospital stay have all decreased. This observation supports the concept that there is a learning curve and that over time with increased skill, outcomes can continue to improve. We would predict that this approach is associated with reduced pain and earlier postoperative mobility and discharge and intend to examine this further in a randomised controlled trial.
Conclusions
The uniportal SVATS technique should be considered as an alternative approach to thoracoscopic resection of an anterior mediastinal mass. The uniportal SVATS technique is particularly suitable for thymectomy since it allows an extended view of the anterior mediastinum as well as the right and left pleural spaces from phrenic-to-phrenic. It allows the surgeon to perform a radical oncological thymectomy with lower risk of damaging adjacent nerves and vessels.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.10.13). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Shanghai Pulmonary Hospital Ethical committee (No. 010029) and informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Demmy TL, Nwogu C. Is video-assisted thoracic surgery lobectomy better? Quality of life considerations. Ann Thorac Surg 2008;85:S719-28. [Crossref] [PubMed]
- Demmy TL, Curtis JJ. Minimally invasive lobectomy directed toward frail and high-risk patients: a case-control study. Ann Thorac Surg 1999;68:194-200. [Crossref] [PubMed]
- Sugiura H, Morikawa T, Kaji M, et al. Long-term benefits for the quality of life after video-assisted thoracoscopic lobectomy in patients with lung cancer. Surg Laparosc Endosc Percutan Tech 1999;9:403-8. [Crossref] [PubMed]
- Suda T, Hachimaru A, Tochii D, et al. Video-assisted thoracoscopic thymectomy versus subxiphoid single-port thymectomy: initial results†. Eur J Cardiothorac Surg 2016;49:i54-8. [PubMed]
- Suda T. Uniportal subxiphoid video-assisted thoracoscopic thymectomy. J Vis Surg 2016;2:123. [Crossref] [PubMed]
- Fok M, Karunanantham J, Ali JM, et al. Subxiphoid approach for spontaneous bilateral pneumothorax: a case report. J Vis Surg 2017;3:146. [Crossref] [PubMed]
- Karunanantham J, Fok M, Ali JM, et al. Subxiphoid single incision thoracoscopic surgery approach for thymectomy: a case report. J Vis Surg. 2017;3:147-7. [Crossref] [PubMed]
- Karunanantham J, Fok M, Ali JM, et al. Subxiphoid single incision thoracoscopic surgery approach for thymectomy: a case report. J Vis Surg 2017;3:147. [Crossref] [PubMed]
- Ali JM, Kaul P, Jiang L, et al. Subxiphoid pneumonectomy: the new frontier? J Thorac Dis 2018;10:4464-71. [Crossref] [PubMed]
- Aresu G, Wu L, Lin L, et al. The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies. J Vis Surg 2016;2:135. [Crossref] [PubMed]
- Aresu G, Weaver H, Wu L, et al. The Shanghai Pulmonary Hospital uniportal subxiphoid approach for lung segmentectomies. J Vis Surg 2016;2:172. [Crossref] [PubMed]
- Gonzalez-Rivas D, Lirio F, Sesma J, et al. Subxiphoid complex uniportal video-assisted major pulmonary resections. J Vis Surg 2017;3:93. [Crossref] [PubMed]
- Raza A, Woo E. Video-assisted thoracoscopic surgery versus sternotomy in thymectomy for thymoma and myasthenia gravis. Ann Cardiothorac Surg 2016;5:33-7. [PubMed]
- Aresu G, Jiang L, Bertolaccini L. Subxiphoid video-assisted major lung resections: the Believers' speech. J Thorac Dis 2017;9:E387-9. [Crossref] [PubMed]
- Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016;50:1060-6. [Crossref] [PubMed]
- Li L, Tian H, Yue W, et al. Subxiphoid vs intercostal single-incision video-assisted thoracoscopic surgery for spontaneous pneumothorax: A randomised controlled trial. Int J Surg 2016;30:99-103. [Crossref] [PubMed]
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Subxiphoid uniportal VATS thymectomy. J Vis Surg 2017;3:171. [Crossref] [PubMed]
- Numanami H, Yano M, Yamaji M, et al. Thoracoscopic Thymectomy Using a Subxiphoid Approach for Anterior Mediastinal Tumors. Ann Thorac Cardiovasc Surg 2018;24:65-72. [Crossref] [PubMed]
- Weaver H, Ali JM, Jiang L, et al. Uniportal subxiphoid video-assisted thoracoscopic approach for thymectomy: a case series. J Vis Surg 2017;3:169. [Crossref] [PubMed]
- Zhang H, Chen L, Zheng Y, et al. Robot-assisted thymectomy via subxiphoid approach: technical details and early outcomes. J Thorac Dis 2018;10:1677-82. [Crossref] [PubMed]
Cite this article as: Ali JM, Volpi S, Jiang L, Yang C, Wu L, Jiang G, Aresu G. The future of minimally invasive thymectomy: the uniportal subxiphoid video-assisted thoracic surgery technique—a case series. J Vis Surg 2018;4:222.