Thoracic outlet syndrome: a surgical approach by videothoracoscopy
Introduction
Thoracic outlet syndrome (TOS) is the term used to describe various signs and symptoms caused by compression of neurovascular structures, such as the brachial plexus, subclavian artery and/or vein, when these structures are leaving the narrow space between the shoulder girdle and the first rib, in the region referred to as the cervicotoracobraquial outlet or only thoracic outlet, usually occurring by bone and/or musculoligamentous anomalies (1-4).
Inside these restricted spaces pass the subclavian artery and the brachial plexus. The subclavian vein passes anteriorly to the interscalene triangle and by the costoclavicular space (5).
Vascular and neurological problems are frequent because of extrinsic compression (6). The subclavian vein may suffer thrombosis, and post-stenotic dilation may occur in the subclavian artery, both are complicated by thromboembolic phenomena (7). Venous symptoms are characterized primarily by edema and cyanosis of the affected upper limb, and the arteries, by finger ischemia and/or claudication.
Nerve compressions are frequent, but they are more difficult to diagnose, because patients usually report symptoms of cooling and color changes due to the sympathomimetic stimuli resulting from the compression of sympathetic fibers that accompany the lower roots of the brachial plexus (C7 and T1) (5,8). They are manifested mainly by paraesthesia, weakness and/or pain not only of the upper limb but also of the cervical region (5,8).
When we can prove the neural commitment by means of specific exams, the TOS is called neurogenic (TOSn). When we cannot prove this, facing symptoms and signs of the neurogenic syndrome, it is classified as symptomatic TOS (sTOS). The narrow space of the thoracic outlet may be even more restricted with the presence of a cervical rib and, in this case, neurogenic symptoms usually prevail (9).
Cervical rib resection is traditionally performed through supraclavicular or axillary access. It can also be done by means of a scapular, although this is more commonly used in reoperations (8). Although technically attractive and associated with less invasiveness and safety, presenting a great aesthetic result, resection of the first rib of the chest by transaxillary video-assisted surgery (10) or video-assisted thoracic surgery (VATS) (11) is little reported in the literature, and none anomalous cervical rib resection reference was found by the last technique (VATS).
Anatomical and morphological variation
The term TOS was first used by Peet et al. in 1956 and describes a clinical picture attributed to compression of the brachial plexus, artery and subclavian veins in the thoracic outlet region.
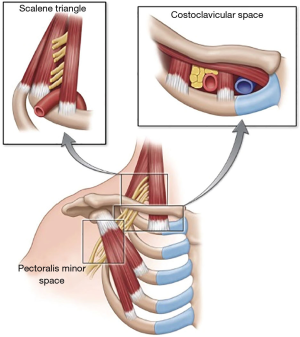
The thoracic outlet consists of two anatomical spaces (Figure 1):
- Space of the interscalene triangle: it comprises the space between the anterior scalene muscle (anteriorly), the middle and posterior scalene muscles (subsequently) and the first rib (inferiorly). The upper trunk of the brachial plexus (roots C5 and C6) and the middle trunk (root C7) occupy the upper portion of this space. The lower trunk (roots C8 and T1) occupies the lower part, posterior to the subclavian artery, which is situated on the lower margin of this space;
- Costoclavicular space: delimited by the medial half of the clavicle (superiorly), by the cranial face of the first rib (inferiorly), by the cost-clavicular or rhomboid ligament (previously) and by the posterior scalene muscle.
Epidemiology
The incidence of TOS varied from 3 to 80 cases/1,000 in habitants, predominating in women from 20 to 50 years old (12).
Classification system
Patients with the aforementioned syndrome can be divided into two large groups: neurogenic and vascular (13).
The neurogenic type is more common, with approximately 95% of the cases. It is subdivided into:
- TOS classic or true neurogenic: rare, 1–3% of cases, usually unilateral, affecting more adult women. It is associated with bone abnormalities (13-15);
- TOS atypical or controversial or non-specific neurogenic: it corresponds to more than 90% of the cases, is described mainly as bilateral and affects more young women (14,15). Its cause is controversial because there is no sign of objective neurological compression (14,16).
The vascular type, with approximately 5% of cases, is subdivided into:
- TOS arterial syndrome: rare, 2–3% of cases, usually unilateral, affecting young adults. Consists of complications of chronic arterial compression by bone abnormalities (13-15,17);
- TOS venous syndrome: rare, 1–2% of cases. Also known as
- Stress venous thrombosis or Paget-Schroetter syndrome. It affects more young adults. Spontaneous thrombosis of the subclavian vein occurs due to prolonged use of the upper extremity (13-15,17,18).
Diagnosis
Signs/symptoms
Over the years studying this syndrome, it has been noticed that neurological symptoms are more frequent, corresponding to 95% of cases with clinical symptoms, according to the Brazilian Journal of Vascular Surgery 2008. Arterial complications are rare, but potentially more serious and may lead to significant sequel.
TOS may have nervous and/or vascular symptoms, which are divided into arterial and venous (19).
Often there are nervous symptoms, which can affect sensitivity, motor and tropism. They manifest with pain of varying intensity and character, and may have inaccurate location, along with weakness, paresthesia, especially in the hands and fingers. In general, when the upper cord of the brachial plexus (C5, C6, C7) is compressed, the pains are in the lateral region of the head and neck, in the region of the rhomboid and suprascapularis muscle, the lateral aspect of the upper limb, the dorsal part of the hand, between 1 and 20. fingers. Compression of the lower cord (C8 and T1) is more common. The pain occurs in the suprascapular region, nuchal, medial face of the upper limb, 4th and 5th fingers.
In the presence of cervical ribs, due to local compression, the supraclavicular region may be spontaneously painful or triggered by movements that exacerbate compression, such as hyperabduction of the arm and when caring heavy objects, which promotes lowering of the shoulders.
The motricity change can range from weakness to incapacitation, just as trophic changes are like hypotrophy and as atrophies, most common in extrinsic muscles of the hand and forearm (19-21).
Arterial symptoms occur through ischemia, include pain, paleness, cyanosis, erythrocyanosis, paresthesia, fatigue, trophic changes such as ulcers and gangrene, local temperature decrease. They have as an aggravating factor the cold and the exercise (13,14,19,21). Vasomotor symptoms, mainly Raynaud’s phenomenon.
About the venous compression, symptoms are of weight sensation, pain and engorgement of the upper extremity, increased skin temperature, cyanosis, edema, venous turgidity, especially in the shoulder and pectoral region (14,19,21).
Clinical diagnosis
There are five physical examination maneuvers that aid in diagnosis:
- Wright’s maneuver;
- “Hands up” maneuver;
- ROOS test;
- Tinel’s maneuver;
- Adson’s maneuver.
However, none of these tests are accepted as a gold standard because they have 72% sensitivity and 53% specificity. The positivity of the five maneuvers in patients with compatible clinical history confers sensitivity and specificity of 84%. Among all, the most reliable is Adson’s Maneuver.
Laboratorial diagnosis
Besides the anamnesis and physical examination, we can perform complementary exams in order to diagnose TOS.
- Simple chest X-ray: may show bone abnormalities and tumor compression. However, it is normal in 85% of the patients with a clinical picture compatible with TOS;
- Electroneuromyography: it may be useful in the diagnosis of TOS of neurogenic origin. However, as the nerve clamping is intermittent and in only a short segment on the nerve, the examination may be normal or give a false-negative result;
- Angiography by digital subtraction: is one of the methods that can identify arterial compression, showing the location and type of narrowing and its dynamic variation with the change of position of the upper limb;
- Ultrasonography with color Doppler: can detect undiagnosed cases in clinical maneuvers. Besides not being invasive nor involving use of ionizing radiation. It may be used when there are contraindications to angiography;
- Computed angiotomography: it is less invasive than digital angiography because it only uses peripheral venous access. In transverse sections it has sensitivity and specificity of approximately 67% and 69%, respectively, and in sagittal sections, of 96% and 94%;
- Magnetic Resonance: this exam helps to elucidate the cause and the location of the compression.
Differential diagnosis
A series of examinations were performed to differentiate TOS from other causes of similar symptoms and signs. Superior pulmonary sulcus carcinoma and esophageal or cardiac disease were excluded by the appropriate tests.
Conservative management
Conservative treatment, initiated shortly after or during drug treatment is the initial conduct and seeks to alleviate the symptoms, especially if among them present the inflammation, it will first be directed elimination of the causative mechanism and control, with an emphasis on reducing pressure biomechanics and increasing the mobility of tissues in the affected region, being effective for improvement of function and return to work (22,23).
It is necessary to educate the patient about modify or eliminate postures and activities that cause symptoms such as hyper abduction of the upper limbs and/or carrying heavy objects (3,23).
When treatment fails conservative or the TOS is due to anomalies symptomatic bone or vascular complications or surgical treatment is indicated in approximately 15% of cases surgical techniques consist of decompression anatomic points such as resection of the scalene muscle, the cervical rib, the first rib, clavicle and fibrous flanges or other structures that may be leading to compression (3).
Surgical therapy
Resection of the first rib by video-assisted technique occurs with the patient in lateral decubitus, with the side to be operated facing upward, in a posterolateral thoracotomy position; under general anesthesia and mono-pulmonary ventilation.
Three incisions are used, the first one in the seventh intercostal space and the posterior axillary line, where a 5-mm Trocater is passed, through which 5-mm and 30-degree optics will be inserted; the second incision, in the fourth intercostal space and anterior axillary line also of 5 mm, where it will pass a Trocater of 5 mm and by him the harmonic scalpel; and finally the third incision in the axilla with approximately 3 cm, where we will perform the lowering of the first rib and also used to section the first rib and remove its fragments.
Used as a dedicated material a harmonic scalpel hook, because it causes less thermal injury, with a lower risk of injuries to the brachial plexus and subclavic vessels; a shears for first rib or drill for the section of the first rib and ropes from doyan and cobe type.
Once the patient is anesthetized and positioned, the ventilatory block of the lung is performed on the side to be operated and the first rib is exposed with the use of the harmonic scalpel, the section of the parietal pleura being performed initially by the lower edge of the rib (first intercostal space) and anterior scalene muscle section. Also, during this surgical time, the index finger is introduced through the axillary incision, pushing the first rib caudally, which will help to better expose the anterior and middle scalene muscles to its section and protect the neurovascular structures from the use of the harmonic scalpel. The costal dissection then follows towards the cost-vertebral joint. After this surgical time, we began to dissect the upper edge of the rib, where there is a greater risk of neurovascular lesions, keeping the pressure on the rib with the index finger until we can introduce the finger into the pleural cavity through the axillary incision, and cut the rib in its midpoint, where the costotome (sheaf) will be introduced and cut into ribs. The anteromedial dissection of the rib with a section of the costoclavicular ligament and the sternum-costal cartilage is followed, releasing the anterior segment of the rib and withdrawing it through the axillary incision.
After resection of the anterior portion, we began the dissection of the posterior portion of the rib, which can be used under direct and tactile vision of doyan and cobe’s routs with release of the posterior scalene muscle and release of the costovertebral ligaments with release and removal of the posterior segment of the rib. In this stage it is fundamental to release the rib posteriorly and never its section; since the remaining cote may lead to the formation of fibrosis with brachial plexus clamping.
Once the rib is removed, hemostasis and visualization of the vasculo-nerve structures are performed with their full release. We continue with pleural drainage under water seal with 28-Fr drain, pulmonary re-expansion and referral of the patient to the anesthetic recovery center.
Attached video teaching technique (Figure 2).
Conclusions
The surgical technique by videothoracoscopic video-assisted surgery is poorly reported, therefore, technically attractive and related to less invasiveness and greater safety.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ricardo M. Terra and Paula A. Ugalde) for the series “Minimally Invasive Surgery - Robotics and VATS in Brazil” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2018.12.13). The series “Minimally Invasive Surgery - Robotics and VATS in Brazil” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cruz M, Alves de Matos A, Saldanha T, et al. Angiography as a diagnostic tool in the neurovascular outlet syndrome. A clinical case. Rev Bras Reumatol 2003;43:267-71. [Crossref]
- Mezzalira GW, Malucelli AV, Carvalho TR, et al. Thoracic outlet syndrome and subclavian artery compression. Rev Méd Paraná 2005;63:26-8.
- Silvestri K, Wagner F, Dal Moro AN. Síndrome do desfiladeiro torácico: Revisão teórica. Arquivos Catarinenses de Medicina 2005;34:92-6.
- Rochkind S, Shemesh M, Patish H, et al. Thoracic outlet syndrome: a multidisciplinary problem with a perspective for microsurgical management without rib resection. Acta Neurochir Suppl 2007;100:145-7. [Crossref] [PubMed]
- Mackinnon SE, Novak CB. Thoracic outlet syndrome. Curr Probl Surg 2002;39:1070-145. [Crossref] [PubMed]
- Povlsen B, Belzberg A, Hansson T, Dorsi M. Treatment for thoracic outlet syndrome. Cochrane Database Syst Rev 2010;CD007218 Update in: Treatment for thoracic outlet syndrome [Cochrane Database Syst Rev 2014]. [PubMed]
- Thompson RW, Petrinec D, Toursarkissian B. Surgical treatment of thoracic outlet compression syndromes. II. Supraclavicular exploration and vascular reconstruction. Ann Vasc Surg 1997;11:442-51. [Crossref] [PubMed]
- Urschel HC, Kourlis H. Thoracic outlet syndrome: a 50-year experience at Baylor University Medical Center. Proc (Bayl Univ Med Cent) 2007;20:125-35. [Crossref] [PubMed]
- Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg 2007;46:601-4. [Crossref] [PubMed]
- Martinez BD, Wiegand CS, Evans P, et al. Computer-assisted instrumentation during endoscopic transaxillary first rib resection for thoracic outlet syndrome: a safe alternate approach. Vascular 2005;13:327-35. [Crossref] [PubMed]
- Ohtsuka T, Wolf RK, Dunsker SB. Port-access first-rib resection. Surg Endosc 1999;13:940-2. [Crossref] [PubMed]
- Huang JH, Zager EL. Thoracic outlet syndrome. Neurosurgery 2004;55:897-902; discussion 902-3. [Crossref] [PubMed]
- Garcia ND, Eskandari M, Tehrani H, et al. Thoracic Outlet Obstruction. eMedicine Journal 2003; October 24. Available online: http://www.emedicine.com/med/topic2774.htm
- Wilbourn AJ. 10 most commonly asked questions about thoracic outlet syndrome. Neurologist 2001;7:309-12. [Crossref] [PubMed]
- Sheth RN, Belzberg AJ. Diagnosis and treatment of thoracic outlet syndrome. Neurosurg Clin N Am 2001;12:295-309. [Crossref] [PubMed]
- Balci AE, Balci TA, Cakir O, et al. Surgical treatment of thoracic outlet syndrome: effect and results of surgery. Ann Thorac Surg 2003;75:1091-6; discussion 1096. [Crossref] [PubMed]
- Colli BK, Dias LAA. Síndrome do Desfiladeiro Torácico. Arq Bras Neurocirurg 1993;12:23-8.
- Scola RH, Werneck LC, Iwamoto FM, et al. Síndrome do Desfiladeiro Torácico Tipo Neurogênico Verdadeiro. Arq Neuro-Psiquiatr 1999;57:659-65. [Crossref]
- Adams JGJ, Silver D. Síndrome do Desfiladeiro Torácico. In: Sabiston DCJ, Lyerly HK. editors. Tratado de Cirurgia. As Bases Biológicas da Prática Cirúrgica Moderna. 15a. edição. Rio de janeiro: Editora Guanabara Koogan, 1999:1752-55.
- Owens JC. Thoracic Outlet Compression Syndromes. In: Hainovici H. editor. Vascular Surgery Principles & Techniques. New York: McGraw-Hill Book Company a Blakiston Publication, 1976:734-57.
- Araújo JD de, Arruda S. Síndromes Compressivas neurovasculares do Desfiladeiro Cervicotoracoaxilar e Síndrome do Túnel do Carpo. In: Maffei FHA, Lastória S, Yoshida WB, et al. Doenças Vasculares Periféricas. 2nd editon. Rio de Janeiro: MEDSI Editora Médica e Científica, 1995:1247-73.
- Vanti C, Natalini L, Romeo A, et al. Conservative treatment of thoracic outlet syndrome. A review of the literature. Eura Medicophys 2007;43:55-70. [PubMed]
- Kisner C, Colby LA. Exercícios Terapêuticos: fundamentos e técnicas. 4th edition. São Paulo: Manole, 2005.
- da Costa Ferreira HP, de Carvalho Maia B, Araújo NM. First rib resection by VATS. Asvide 2019;6:005. Available online: http://www.asvide.com/article/view/29419
Cite this article as: da Costa Ferreira HP, de Carvalho Maia B, Araújo NM. Thoracic outlet syndrome: a surgical approach by videothoracoscopy. J Vis Surg 2019;5:6.