Video-assisted thoracic surgery (VATS): impressions from members of the Brazilian Society of Thoracic Surgery
Introduction
For the past 20 years the development of minimally invasive surgery has been steadily accelerating. This technique minimizes the response to trauma and optimizes patient recovery without compromising the final surgical result (1-5). Thoracic surgery followed this tendency, so that anatomic pulmonary resections through video-assisted thoracic surgery (VATS) are routinely performed in hospitals around the world and the number of studies reporting complex procedures such as resection of tumors with hilar lymph node enlargement or sleeve resections has increased in recent years (6-11).
Even with the proven advantages of the minimally invasive approach, technical and financial constraints have hampered its implementation, especially in developing countries such as India, Mexico and Brazil (12,13). Our previous work reports results of VATS lung resections performed in several Brazilian institutions and it shows results comparable to big databases, such as the European Society of Thoracic Surgery (ESTS) and STS. It is, therefore, feasible and its practice should be encouraged in our country (14).
Main objective
The main objective of this study was to report the current setting of VATS surgery in Brazil, applied for anatomic lung resections, such as lobectomies.
Secondary objectives
- To define the number of surgeons who employ VATS in their practice, as well as their preferable techniques;
- To evaluate the characteristics of these surgeons and their work place;
- To analyze surgeons’ perceptions regarding the barriers for the wide implementation of the technique.
Methods
This is a transversal study supported by the Brazilian Society of Thoracic Surgery (BSTS). Recruitment was accomplished by the BSTS’ mailing, newsletter and social network. A survey was elaborated to be taken by thoracic surgeons, members of the BSTS, who placed their consents. Participants’ identities were preserved through a coding system and a link to take the survey was sent via e-mail. Participants responded the survey from January to April of 2015.
Survey was developed in REDCap™ software. Inquiries involved participants’ demographic characteristics, their concepts of VATS, the techniques they apply, their perceptions and difficulties with the method. Time required to answer the survey ranged from 5 to 15 minutes. This survey was strongly influenced and inspired by a previous survey applied to members of the ESTS, as described by Rocco et al. (15). The full questionnaire, translated to English, is available in Supplement I.
Definition of outcomes and variables
Main outcome consisted of characteristics of all thoracic surgeons who responded the survey and the thoracic surgeons who perform VATS lobectomies.
Secondary outcomes concerned surgeons’ perceptions and employed techniques and, with that, presumable reasons and causes that facilitate the usage of video-assisted surgery in the country, as well as the counterpoints that hamper its full implementation.
- Characteristics of all participants (section 1 of the survey);
- Characteristics of participants who perform VATS lobectomy;
- Surgeons’ perceptions (section 2 of the survey);
- Employed techniques (section 3 of the survey).
Data analysis
One of the outcomes in this study is to identify the number of subjects who adhere to VATS technique, therefore, sample was not calculated. Categorical variables are presented as absolute numbers and percentages. Numerical variables are expressed as mean and standard deviation when they have normal distribution or as median and quartiles 25–75 when they have asymmetrical distribution. All numerical variables were tested for normality using graphic methods and the Shapiro-Wilk test.
We analyzed features that may influence surgeons performing VATS lobectomy or not. To identify those features we used logistic regression (backwards method) and considered P≤0.05 as statistically significant, so variables with P>0.05 were excluded from the model. Statistical analysis was performed with software SPSS V.20 from IBM®.
This study was approved by the Ethics Commission of the School of Medicine of the University of São Paulo under the number: CAAE: 40434414.6.0000.0065.
Results
A total of 714 invitations to participate in the survey were sent, from which 224 (31.3%) thoracic surgeons responded, being 219 (97.8%) complete answers and 5 (2.2%) incomplete answers. There were 209 men (93.3%), mean age was 44.24 years (29–76 years, SD 10.5). Most participants (n=153, 68.3%) performed at least one VATS lobectomy. However, only 84 surgeons perform VATS lobectomy over traditional thoracotomy in more than 30% of their procedures. Participants’ characteristics are summarized in Table 1.
Table 1
| Characteristic | Number |
|---|---|
| Age, years (average, range) | 44.24 [29–76] |
| Gender, n (%) | |
| Male | 209 (93.3) |
| Female | 15 (6.7) |
| Time since completion of medical residency, years (average, range) | 14.78 [0–47] |
| Surgeons that work in cities with more than a million inhabitants, n (%) | 128 (57.1) |
| Type of institution, n (%) | |
| University hospital | 103 (22.2) |
| Public hospital | 132 (28.4) |
| Private hospital | 173 (37.3) |
| Philanthropic hospital | 56 (12.1) |
| Annual volume of lobectomies, median, IQ 25–75% | 20 [10–30] |
| Surgeons that perform VATS lobectomies, n (%) | 153 (68.3) |
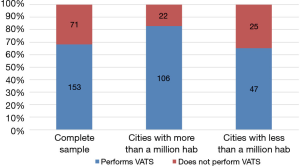
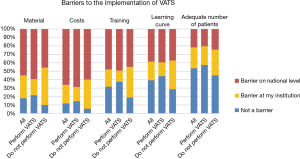
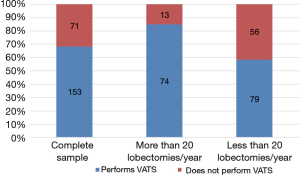
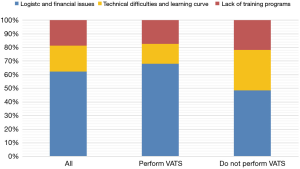
Surgeon’s annual volume of lobectomies positively influenced chances of performing VATS (OR 1.04; 95% CI, 1.01–1.07; P=0.004), as did the place where the surgeon performs: cities with more than one million inhabitants increased the chance of performing VATS (OR 2.58; 95% CI, 1.27–5.24; P=0.009) (Figures 1,2). Median volume of lobectomies per year was 20. One hundred and twenty-eight surgeons perform their activities in cities with more than a million inhabitants, 72 surgeons are in cities with less than a million inhabitants and 24 participants did not inform their cities. Participants found logistic and financial issues to be the main reason for VATS not to be completely implemented in our country, followed by lack of training programs, as shown on Figure 3. According to local or national barriers, the later and other issues are reported on Figure 4.
Concerning the concepts of VATS surgery, most surgeons (n=103, 36.7%) agreed with employing the term “video-assisted thoracic surgery”, as opposed to videothoracoscopy (n=93, 33.1%) or minimally invasive thoracic surgery (n=85, 30.2%). The absence of rib spreading was considered the main definition of a VATS procedure for 157 (70.4%) respondents. The best advantage of VATS lobectomy, for 149 (66.8%) surgeons, is better and faster post-operative recovery. Eighty-six (33.8%) surgeons received their VATS training during their medical residency and short durations courses promoted by the industry, while 79 (31.1%) respondents were trained only during their thoracic surgery residency.
The technique most surgeons (n=84, 55.3%) employ involves the use of 2 other ports in addition to the main incision, the mini thoracotomy. The most frequent counter indications to VATS lobectomy were tumor size—114 (50.9%) responses, and the need for arterioplasty—106 (47.3%) responses, while the factor that would lead a surgeon to convert a VATS lobectomy to an open thoracotomy is bleeding—129 (57.6%) responses. Pleural drainage with one drain is the preferred approach for 136 (60.7%) surgeons and a minority (n=26, 11.6%) makes use of gas insufflation.
Discussion
Video-assisted pulmonary lobectomies and other lung resections already constitute the majority of thoracic procedures throughout the world, in large thoracic surgery centers. The initial implementation of VATS surgery in our country, as well as in other developing countries was somewhat delayed due to the costs associated to the procedure and the necessary equipment. The opinion of Brazilian surgeons corroborates that fact and shows that, even today, there are places where it is hard to find suitable equipment and structure to perform VATS surgery.
Aspects of nomenclature and technique were in agreement with most Brazilian surgeons and they did not differ from the European survey by Rocco et al. The latter showed a clear difference from our survey concerning reasons that hamper VATS’ wide popularity spread: while most of Brazilian surgeons felt that logistic and financial issues were the main accountable reasons, the majority of responses from the European survey pointed at learning curve and difficult technique (15).
Volume of surgery was a clear influencer of the odds of performing VATS lobectomy, increasing these when the surgeons perform more than 20 lobectomies per year. City size had the same influence and probably because in the big cities lie the largest number of patients and, therefore, surgeries. It has been suggested that a center that performs VATS lobectomies should do it at least 20 times a year, should contribute to a national database and have a regular attendance to symposiums of minimally invasive surgery (6).
In spite of all these barriers, VATS surgery supporters continuously increase within the country as VATS’ benefits are progressively clearer, such as better post-operative pain control, shorter length of ICU and hospital stay, patients’ satisfaction with the procedure. In order to VATS surgery to continue its growth, we must invest in training programs and pressure suppliers and government to provide acceptable prices and low taxes, respectively, for the equipment, so that everyone can benefit from this type of surgery. The same applies to robotic-assisted thoracic surgery (RATS). It is up to the Thoracic Society to promote continuous training in VATS surgery, to residents and to already experienced surgeons, so that we can all employ this technique in our practice with quality, for patients’ benefits.
Supplementary
Supplement I Questionnaire Sent to the Members of the Brazilian Society of Thoracic Surgery (BSTS)
- Fields that allow only one response among the alternatives
- Fields that allow several responses among the alternatives
Please answer the questions and check the alternatives with which you agree the most.
Section 1—Characteristics of all participants
How old are you? ________ years old
Gender
- Female
- Male
How long has it been since the completion of your medical residency? __________________________________ (In years, at the time of filling this Questionnaire)
Which State do you work in?
- SP
- MG
- RJ
- ES
- PR
- SC
- RS
- GO
- MT
- MS
- DF
- MA
- PI
- CE
- RN
- PB
- PE
- AL
- SE
- BA
- AM
- RO
- AC
- RR
- AP
- PA
- TO
In which city do you perform most of your surgeries? ____________________________________________________________
Type of institution you work at
- University
- Public
- Private
- Philanthropic
What’s your annual volume of lobectomies? ____________________________________________________________________
(in the 12 months prior to completing this Questionnaire)
Do you perform lobectomies by video-assisted thoracic surgery (VATS)?
- No
- Yes
How many VATS lobectomies have you performed? _____________________________________________________________
Which percentage of your lobectomies is VATS?
- More than 50%
- Between 30% and 50%
- Between 10% and 30%
- Less than 10%
What is your formation and training in VATS? (You can mark more than one alternative)
- Residency
- Specialization, “Fellowship”, long duration courses (more than 6 months)
- Short-term courses (less than 6 months) promoted by universities or societies
- Short-term courses promoted by the industry
- I have no formal training in video-assisted surgery
When did your lobectomies VATS program start? (in relation to the moment of filling this Questionnaire)
- More than 10 years ago
- Between 5 and 10 years ago
- Between 3 and 5 years ago
- Between 1 and 3 years ago
- Less than a year ago
Section 2—Surgeons’ perceptions
Which terminology do you prefer and use to describe less invasive thoracic procedures? (Check how many alternatives you deem appropriate)
- Video-assisted thoracic surgery
- Videothoracoscopy
- Minimally invasive thoracic surgery
- Thoracic surgery with small access
- Other
- Don't know
What criterion do you consider as the principal in defining a lobectomy as video-assisted? (Choose only one alternative)
- Skin incision smaller than 8 cm
- Intercostal incision smaller than 8 cm
- Preserve chest wall muscles
- No rib spreading
- No rib incision or fracture
And which criterion do you consider as the second most important to define a lobectomy as video-assisted? (Choose only one alternative)
- Skin incision smaller than 8 cm
- Intercostal incision smaller than 8 cm
- Preserve chest wall muscles
- No rib spreading
- No rib incision or fracture
Which of the following actions, in your opinion, preclude a lobectomy from being considered as video-assisted? (Check how many alternatives you deem appropriate)
- Skin incision larger than 8 cm
- Intercostal incision larger than 8 cm
- Incision of chest wall muscles
- Rib spreading
- Rib incision or fracture
- Viewing most of the surgery through the thoracotomy
- Viewing any part of the surgery through the thoracotomy
- More than 4 incisions (including thoracotomy)
What are your main indications for VATS?
- Diagnostic procedures only (mediastinoscopy, pleuroscopy)
- Diagnostic and small procedures (wedge resection, surgery for pneumothorax)
- Diagnostic, small and large procedures (anatomical segmentectomy, lobectomy, thymectomy)
What surgeries do you perform by VATS? (You can mark more than one alternative)
- None
- Pleuroscopy
- Sympathectomy
- Pneumothorax surgery (bullectomy)
- Pulmonary decortication
- Non-anatomical resection and lung biopsy—interstitial disease or peripheral nodules
- Lobectomies
- Anatomic segmentectomy
- Chest wall resections
- Resections with bronchoplasty
- Resections with arterioplasty
When there is a need to access the pleural cavity, how often do you use lateral muscle-sparing thoracotomy?
- More than 50% of times
- Between 30% and 50% of times
- Between 10% and 30% of times
- Less than 10% of times
And how often do you use non-sparing posterior-lateral thoracotomy
- More than 50% of times
- Between 30% and 50% of times
- Between 10% and 30% of times
- Less than 10% of times
Among the items described, which do you consider to be the main advantage of VATS lobectomy? (Choose only one alternative)
- Better tolerance to the procedure in patients with comorbidities and poor lung function
- Better oncological outcome
- Better aesthetic aspect
- Better and faster post-operative recovery
- Lesser pain during post-operative time
- Shorter in-hospital time
And which do you consider to be the second most important advantage of VATS lobectomy? (Choose only one alternative)
- Better tolerance to the procedure in patients with comorbidities and poor lung function
- Better oncological outcome
- Better aesthetic aspect
- Better and faster post-operative recovery
- Lesser pain during post-operative time
- Shorter in-hospital time
Which factors, in the course of time, have influenced the likelihood of you performing minimally invasive procedures? (Check how many alternatives you deem appropriate)
- Evidences on safety and effectiveness
- Patients’ demands for less invasive options
- Medical staff’s demands for less invasive options
- Legal/litigious scenery
- Changes in available technology
- Colleagues’ opinion
In your opinion, what is the main reason that precludes VATS lobectomy from being broadly spread across Brazil? (Choose only one alternative)
- Not enough evidence to ensure safety and effectiveness
- Technical difficulty, learning curve
- Resistance to innovation on behalf of surgeons
- Logistic and financial issues
- Lack of training and re-training
And what do you consider the second reason that precludes VATS lobectomy from being broadly spread across Brazil? (Choose only one alternative)
- Not enough evidence to ensure safety and effectiveness
- Technical difficulty, learning curve
- Resistance to innovation on behalf of surgeons
- Logistic and financial issues
- Lack of training and re-training
Do you consider that robotic surgery (RATS) is part of minimally invasive thoracic surgery?
- Yes, it is an evolution of VATS
- Yes, because it avoids sternotomy or thoracotomy
- Yes, because it allows less manipulation of the lungs
- No, my criteria for minimally invasive surgery are not compatible with robotics
Why do you think robotic surgery is yet to reach popularity? (You can mark more than one alternative)
- Financial issues
- Technological limitation of the equipment
- Robotics will not gain popularity until VATS is more accepted and consolidated
- Lack of evidence showing the superiority of RATS over VATS
If you were head of a service with 4 thoracic surgeons, how many should receive training in thoracoscopic surgery and perform VATS lobectomies?
- Depends on the workload and available resources, but at least one
- Only one
- Two
- Three
- All four
How do you idealize residency training in VATS lobectomy?
- Through steps, from classic open surgery to small VATS procedures and then to VATS lobectomy
- With separate VATS training after the conventional training
Do you consider any of the items below as hindrances to the implementation of VATS lobectomies?
- Material
- Costs
- Training
- Learning curve
- Number of adequate patients to the procedure
- √ No, I don’t consider it a barrier
- √ Yes, it is a barrier at my institution
- √ Yes, it is a barrier in my country
Do you believe that every thoracic surgeon must perform VATS lobectomy?
- No
- Yes
Do you believe that every patient benefits from VATS lobectomy?
- No
- Yes
Section 3—Employed techniques
How many incisions, apart from the mini thoracotomy, do you use?
- None (uniportal)
- 1
- 2
- 3
- 4 or more
Which of the following do you consider as counterindications for VATS lobectomy? (You can mark more than one alternative)
- Tumor size
- Hilar lymphadenopathy
- Mediastinal lymphadenopathy
- Neoadjuvant therapy
- Bronchoplasty
- Arterioplasty
- Chest wall resection
- Previous surgery
- Bronchiectasis
- Other
Which of the following have driven you to convert a VATS lobectomy VATS to an open thoracotomy lobectomy? (You can mark more than one alternative)
- Tumor size
- Hilar lymphadenopathy
- Mediastinal lymphadenopathy
- Incomplete fissure
- Bronchoplasty
- Arterioplasty
- Chest wall tumoral invasion
- Bleeding
- Other
Which of these do you use during VATS lobectomy?
- Electrocautery
- Harmonic/ultrasonic cautery
- Sealants
- Other
- Indifferent
How many drains/chest tubes do you place after VATS lobectomy?
- None
- 1
- 2
- 3 or more
What kind of anesthesia do you employ during VATS lobectomy?
- General anesthesia only
- General + epidural block
- General + intercostal lock
- General + local anesthesia
Do you use gas inflation?
- No
- Yes
Section 1—Characteristics of all participants
How old are you? ________ years old
Gender
- Female
- Male
How long has it been since the completion of your medical residency? __________________________________ (In years, at the time of filling this Questionnaire)
Which State do you work in?
- SP
- MG
- RJ
- ES
- PR
- SC
- RS
- GO
- MT
- MS
- DF
- MA
- PI
- CE
- RN
- PB
- PE
- AL
- SE
- BA
- AM
- RO
- AC
- RR
- AP
- PA
- TO
In which city do you perform most of your surgeries? ____________________________________________________________
Type of institution you work at
- University
- Public
- Private
- Philanthropic
What’s your annual volume of lobectomies? ____________________________________________________________________
(in the 12 months prior to completing this Questionnaire)
Do you perform lobectomies by video-assisted thoracic surgery (VATS)?
- No
- Yes
How many VATS lobectomies have you performed? _____________________________________________________________
Which percentage of your lobectomies is VATS?
- More than 50%
- Between 30% and 50%
- Between 10% and 30%
- Less than 10%
What is your formation and training in VATS? (You can mark more than one alternative)
- Residency
- Specialization, “Fellowship”, long duration courses (more than 6 months)
- Short-term courses (less than 6 months) promoted by universities or societies
- Short-term courses promoted by the industry
- I have no formal training in video-assisted surgery
When did your lobectomies VATS program start? (in relation to the moment of filling this Questionnaire)
- More than 10 years ago
- Between 5 and 10 years ago
- Between 3 and 5 years ago
- Between 1 and 3 years ago
- Less than a year ago
Section 2—Surgeons’ perceptions
Which terminology do you prefer and use to describe less invasive thoracic procedures? (Check how many alternatives you deem appropriate)
- Video-assisted thoracic surgery
- Videothoracoscopy
- Minimally invasive thoracic surgery
- Thoracic surgery with small access
- Other
- Don't know
What criterion do you consider as the principal in defining a lobectomy as video-assisted? (Choose only one alternative)
- Skin incision smaller than 8 cm
- Intercostal incision smaller than 8 cm
- Preserve chest wall muscles
- No rib spreading
- No rib incision or fracture
And which criterion do you consider as the second most important to define a lobectomy as video-assisted? (Choose only one alternative)
- Skin incision smaller than 8 cm
- Intercostal incision smaller than 8 cm
- Preserve chest wall muscles
- No rib spreading
- No rib incision or fracture
Which of the following actions, in your opinion, preclude a lobectomy from being considered as video-assisted? (Check how many alternatives you deem appropriate)
- Skin incision larger than 8 cm
- Intercostal incision larger than 8 cm
- Incision of chest wall muscles
- Rib spreading
- Rib incision or fracture
- Viewing most of the surgery through the thoracotomy
- Viewing any part of the surgery through the thoracotomy
- More than 4 incisions (including thoracotomy)
What are your main indications for VATS?
- Diagnostic procedures only (mediastinoscopy, pleuroscopy)
- Diagnostic and small procedures (wedge resection, surgery for pneumothorax)
- Diagnostic, small and large procedures (anatomical segmentectomy, lobectomy, thymectomy)
What surgeries do you perform by VATS? (You can mark more than one alternative)
- None
- Pleuroscopy
- Sympathectomy
- Pneumothorax surgery (bullectomy)
- Pulmonary decortication
- Non-anatomical resection and lung biopsy—interstitial disease or peripheral nodules
- Lobectomies
- Anatomic segmentectomy
- Chest wall resections
- Resections with bronchoplasty
- Resections with arterioplasty
When there is a need to access the pleural cavity, how often do you use lateral muscle-sparing thoracotomy?
- More than 50% of times
- Between 30% and 50% of times
- Between 10% and 30% of times
- Less than 10% of times
And how often do you use non-sparing posterior-lateral thoracotomy
- More than 50% of times
- Between 30% and 50% of times
- Between 10% and 30% of times
- Less than 10% of times
Among the items described, which do you consider to be the main advantage of VATS lobectomy? (Choose only one alternative)
- Better tolerance to the procedure in patients with comorbidities and poor lung function
- Better oncological outcome
- Better aesthetic aspect
- Better and faster post-operative recovery
- Lesser pain during post-operative time
- Shorter in-hospital time
And which do you consider to be the second most important advantage of VATS lobectomy? (Choose only one alternative)
- Better tolerance to the procedure in patients with comorbidities and poor lung function
- Better oncological outcome
- Better aesthetic aspect
- Better and faster post-operative recovery
- Lesser pain during post-operative time
- Shorter in-hospital time
Which factors, in the course of time, have influenced the likelihood of you performing minimally invasive procedures? (Check how many alternatives you deem appropriate)
- Evidences on safety and effectiveness
- Patients’ demands for less invasive options
- Medical staff’s demands for less invasive options
- Legal/litigious scenery
- Changes in available technology
- Colleagues’ opinion
In your opinion, what is the main reason that precludes VATS lobectomy from being broadly spread across Brazil? (Choose only one alternative)
- Not enough evidence to ensure safety and effectiveness
- Technical difficulty, learning curve
- Resistance to innovation on behalf of surgeons
- Logistic and financial issues
- Lack of training and re-training
And what do you consider the second reason that precludes VATS lobectomy from being broadly spread across Brazil? (Choose only one alternative)
- Not enough evidence to ensure safety and effectiveness
- Technical difficulty, learning curve
- Resistance to innovation on behalf of surgeons
- Logistic and financial issues
- Lack of training and re-training
Do you consider that robotic surgery (RATS) is part of minimally invasive thoracic surgery?
- Yes, it is an evolution of VATS
- Yes, because it avoids sternotomy or thoracotomy
- Yes, because it allows less manipulation of the lungs
- No, my criteria for minimally invasive surgery are not compatible with robotics
Why do you think robotic surgery is yet to reach popularity? (You can mark more than one alternative)
- Financial issues
- Technological limitation of the equipment
- Robotics will not gain popularity until VATS is more accepted and consolidated
- Lack of evidence showing the superiority of RATS over VATS
If you were head of a service with 4 thoracic surgeons, how many should receive training in thoracoscopic surgery and perform VATS lobectomies?
- Depends on the workload and available resources, but at least one
- Only one
- Two
- Three
- All four
How do you idealize residency training in VATS lobectomy?
- Through steps, from classic open surgery to small VATS procedures and then to VATS lobectomy
- With separate VATS training after the conventional training
Do you consider any of the items below as hindrances to the implementation of VATS lobectomies?
- Material
- Costs
- Training
- Learning curve
- Number of adequate patients to the procedure
- √ No, I don’t consider it a barrier
- √ Yes, it is a barrier at my institution
- √ Yes, it is a barrier in my country
Do you believe that every thoracic surgeon must perform VATS lobectomy?
- No
- Yes
Do you believe that every patient benefits from VATS lobectomy?
- No
- Yes
Section 3—Employed techniques
How many incisions, apart from the mini thoracotomy, do you use?
- None (uniportal)
- 1
- 2
- 3
- 4 or more
Which of the following do you consider as counterindications for VATS lobectomy? (You can mark more than one alternative)
- Tumor size
- Hilar lymphadenopathy
- Mediastinal lymphadenopathy
- Neoadjuvant therapy
- Bronchoplasty
- Arterioplasty
- Chest wall resection
- Previous surgery
- Bronchiectasis
- Other
Which of the following have driven you to convert a VATS lobectomy VATS to an open thoracotomy lobectomy? (You can mark more than one alternative)
- Tumor size
- Hilar lymphadenopathy
- Mediastinal lymphadenopathy
- Incomplete fissure
- Bronchoplasty
- Arterioplasty
- Chest wall tumoral invasion
- Bleeding
- Other
Which of these do you use during VATS lobectomy?
- Electrocautery
- Harmonic/ultrasonic cautery
- Sealants
- Other
- Indifferent
How many drains/chest tubes do you place after VATS lobectomy?
- None
- 1
- 2
- 3 or more
What kind of anesthesia do you employ during VATS lobectomy?
- General anesthesia only
- General + epidural block
- General + intercostal lock
- General + local anesthesia
Do you use gas inflation?
- No
- Yes
Acknowledgments
We sincerely thank all the colleagues who took their time to participate in this survey.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Minimally Invasive Surgery - Robotics and VATS in Brazil”. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.01.08). The series “Minimally Invasive Surgery - Robotics and VATS in Brazil” was commissioned by the editorial office without any funding or sponsorship. RMT served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Commission of the School of Medicine of the University of São Paulo under the number: CAAE: 40434414.6.0000.0065. Written informed consent was obtained from all participants for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Taioli E, Lee DS, Lesser M, et al. Long-term survival in video-assisted thoracoscopic lobectomy vs open lobectomy in lung-cancer patients: a meta-analysis. Eur J Cardiothorac Surg 2013;44:591-7. [Crossref] [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Swanson SJ, Herndon JE 2nd, D'Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [Crossref] [PubMed]
- Flores RM, Park BJ, Dycoco J, et al. Lobectomy by video-assisted thoracic surgery (VATS) versus thoracotomy for lung cancer. J Thorac Cardiovasc Surg 2009;138:11-8. [Crossref] [PubMed]
- Lewis RJ, Caccavale RJ, Sisler GE, et al. Video-assisted thoracic surgical resection of malignant lung tumors. J Thorac Cardiovasc Surg 1992;104:1679-85; discussion 1685-7.
- Chin CS, Swanson SJ. Video-assisted thoracic surgery lobectomy: centers of excellence or excellence of centers? Thorac Surg Clin 2008;18:263-8. [Crossref] [PubMed]
- Brunelli A, Falcoz PE, D'Amico T, et al. European guidelines on structure and qualification of general thoracic surgery. Eur J Cardiothorac Surg 2014;45:779-86. [Crossref] [PubMed]
- Cooke DT, Wisner DH. Who performs complex noncardiac thoracic surgery in United States academic medical centers? Ann Thorac Surg 2012;94:1060-4. [Crossref] [PubMed]
- Terra RM, Waisberg DR, Almeida JL, et al. Does videothoracoscopy improve clinical outcomes when implemented as part of a pleural empyema treatment algorithm?. Clinics (Sao Paulo) 2012;67:557-64. [Crossref] [PubMed]
- Cirino LM, Milanez de Campos JR, et al. Diagnosis and treatment of mediastinal tumors by thoracoscopy. Chest 2000;117:1787-92. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Piwkowski C, Gabryel P, Gałęcki B, et al. High costs as a slow down factor of thoracoscopic lobectomy development in Poland - an institutional experience. Wideochir Inne Tech Maloinwazyjne 2013;8:334-41. [Crossref] [PubMed]
- Swanson SJ, Meyers BF, Gunnarsson CL, et al. Video-assisted thoracoscopic lobectomy is less costly and morbid than open lobectomy: a retrospective multiinstitutional database analysis. Ann Thorac Surg 2012;93:1027-32. [Crossref] [PubMed]
- Terra RM, Kazantzis T, Pinto-Filho DR, et al. Anatomic pulmonary resection by video-assisted thoracoscopy: the Brazilian experience (VATS Brazil study). J Bras Pneumol 2016;42:215-21. [Crossref] [PubMed]
- Rocco G, Internullo E, Cassivi SD, et al. The variability of practice in minimally invasive thoracic surgery for pulmonary resections. Thorac Surg Clin 2008;18:235-47. [Crossref] [PubMed]
Cite this article as: Terra RM, Kazantzis T. Video-assisted thoracic surgery (VATS): impressions from members of the Brazilian Society of Thoracic Surgery. J Vis Surg 2019;5:17.