
Why choosing a video-assisted thoracic surgery approach for pulmonary metastasectomy?
Introduction
Pulmonary metastases (PMs) develop in approximately 30% of patients with known primary solid cancer. Most such patients receive palliative systemic chemotherapy due to concomitant invasion of other organs. Yet, a non-negligible group of carefully selected patients with PMs might benefit from a complete surgical resection. Their survival might be increased compared to patients who did not undergo surgery, or to those whose resection was incomplete (1). This curative surgical management can be offered to selected patients provided that some criteria are met: primary tumor site is controlled; no other extra-thoracic lesions are detected; metastases are technically resectable and patient may tolerate surgery (2).
This approach is currently acceptable for PMs stemming from various primary malignancies and it represents almost 10% of the daily activity of thoracic surgery clinics. The improvement of radiological imaging has also increased the accuracy of nodule detection. Indirectly, this has increased the number of patients eligible for thoracic surgery. The use of video-assisted thoracic surgery (VATS) metastasectomy is debated for two reasons: there is a risk of missing additional nodules; surgical margins might be reduced by the limited mobility of surgical instruments. Both risks are minimal during thoracotomy (3). Furthermore, VATS has historically been associated with pleural and port-site seeding (4).
Over the past 2 decades, much progress has been achieved in minimally invasive surgery. Nowadays, it has become an acceptable surgical procedure for most pulmonary surgeries. Over the years, numerous new interventions were described, ranging from multiport to uniportal or subxiphoid approaches (5,6). In parallel, many radiological advances (thin slice chest CT-scan, pre- and peri-operative localization of the nodules) have been reported to decrease the associated morbidity and to optimize the surgical procedure (7,8).
It should also be noted that oncological patients frequently require multimodal therapies, including adjuvant chemotherapy and/or immunotherapy to adequately control tumoral growth. Therefore, the surgical and medical teams must strike a careful balance between the side-effects of an efficient oncologic treatment and the equally important quality of life of the patient, which can be improved advantages associated with VATS such as minimizing pain, shortening hospitalization and delaying adjuvant therapies (9).
In this context, minimally invasive approaches have gradually garnered interest as valid alternatives to thoracotomy (10-15). They seem to offer equivalent oncological outcomes (in terms of long-term survival and local recurrence) in cases of pulmonary metastasectomies, along with decreased morbidity and shorter hospital stays, even though no prospective randomized studies are available to directly compare them with standard thoracotomy (3,16). Minimally invasive approaches also meet the growing need of good quality surgical tissue samples to monitor biomarkers for subsequent targeted therapy (17). This review will focus on the role of minimally invasive approaches for pulmonary metastasectomy.
Rationale for VATS metastasectomy
Traditionally, the main objective of lung metastasectomy has been to confirm the metastatic nature of the disease and to achieve complete resection of all detectable lesions (18). However, metastatic diseases are not uniform and surgical management should be personalized based on various individual criteria such as histological characteristics of the primary tumor, number, size or localization of metastases (9).
Two possible metastatic pathways could have an influence on the clinical approach of lung metastasectomy: (I) late dissemination of metastatic cells from the primary tumor with migration and distant implantation after acquisition of sufficient genetic changes; (II) early dissemination during the oncological process spreading numerous dormant cell clusters able to induce a metastasis following genetic and environmental alterations. It is unclear if these processes take place separately or occur concomitantly, depending on tumor types and individuals (19,20). The current surgical metastasectomy approach is based on the idea that the former pathway might prevail (3). It is clear that surgical metastasectomy may not achieve complete resection of all metastatic cells/clusters if the latter pathway might prevail, as pre-metastatic niches are too small to be palpated. A resection approach with surveillance and possible redo surgeries should be favored in such cases. This would be particularly promising in cases where repeat thoracoscopies can be proposed (3).
Thoracotomy has historically been considered the standard because the surgeon can carry out a complete manual palpation of the lung to detect potential additional metastases that could have been missed by conventional pre-operative imaging (1). Nevertheless, up to 50% of patients will suffer disease recurrence during follow-up, a situation associated with substantial morbidity due to decreased pulmonary function and chronic pain (1). In more than 80% of cases, recurrence is located in the non-operated, contra-lateral lung or at a distant extra-thoracic site (21,22). Therefore, in cases deemed eligible for this procedure, a less aggressive approach such as VATS could be justified to avoid unnecessary additional morbidity related to thoracotomy (3). In addition, thoracotomy is reported to carry a high rate (some studies report up to 76%) of unnecessary resections of benign nodules with its surrounding lung parenchyma (23,24).
Since 1990, VATS has progressively gained acceptance for many benign or malignant thoracic conditions. With the standardization and advancement in instrumentations, VATS is now the preferred option in many centers for early stage cancer (25). Its benefits in comparison with thoracotomy are well described: shorter incisions, less pain, less morbidity, better quality of life, shorter length of hospitalization and better compliance to adjuvant treatment.
However, despite these clear advantages, the relevance of VATS in the context of lung metastasectomy was initially debated (Table 1). In a survey directed by the ESTS in 2008, VATS was considered a diagnostic procedure for the vast majority of surgeons and not a potentially curative approach (26).
Table 1
| Advantages over thoracotomy |
| Better visualization of the pleural cavity |
| Better acceptance by patients and referent physicians |
| Better quality of life |
| Shorter incisions |
| Decreased pain |
| Decreased rate of post-operative complications |
| Shorter length of hospital stays |
| Better tolerance to adjuvant treatment |
| Fewer adherences in the event of redo metastasectomy |
| VATS completion anatomical resection in case of non-small cell lung cancer on frozen section |
| Drawbacks compared to thoracotomy |
| Optimal margin resection |
| Port-site recurrence |
| Pleural dissemination |
| Difficulty to palpate the lung |
| Risk of missing additional nodules not detected by pre-operative chest CT-scan. |
| Necessity of peri-operative identification of the lesion in deep-located lesions. |
VATS, video-assisted thoracic surgery.
A more recent survey of cardiothoracic surgeons in Great Britain and Ireland reported that VATS was used by 85% of surgeons in case of isolated pulmonary metastatic lesions (27). In another recent survey including 22 centers with expertise in VATS surgery, 88% of surgeons considered that VATS should be proposed for isolated pulmonary metastasis (28). For the first time, an international society (Society of Thoracic Surgeons) proposed in their 2019 expert consensus statement that a minimally invasive pulmonary metastasectomy could be a valid alternative to traditional thoracotomy for selected patients due to the shorter postoperative recovery and favorable impact on quality of life (29). However, these authors added that if a complete resection and a pulmonary parenchymal sparing cannot be achieved by a minimally invasive technique, open techniques should be preferred. Even without strong evidence in the literature, these recommendations reflect a change in paradigm in favor of less invasive approaches, at least for solitary lesions.
PMs may resemble other conditions such as primary lung cancer or benign inflammatory lesions. Thus, surgery is sometimes the only possibility to histologically confirm metastatic disease. This point is particularly relevant in the context of the development of non-surgical therapies such as stereotaxic radiotherapy or radiological ablative techniques, where histological confirmation is rarely reported. Interestingly, in a recent series of cancer patients, VATS resection of a solitary nodule allowed clear-cut diagnosis of metastasis in only 50% of cases (30). These results suggest that histological confirmation of the nature of pulmonary nodules in cancer patients is crucial to avoid diagnostic uncertainty and sub-optimal treatments when other non-surgical therapies are being considered.
In addition to the complete resection of lung metastases, surgery also provides suitable metastatic tissue samples. These can be analyzed to identify biomarker shifts or resistance patterns for personalized oncological treatment such as targeted therapies or immunotherapies that may follow surgery (9). Current research and analytic tools allow surgeons to more accurately understand the biology and genetics of primary tumors, metastases and recurrent metastases (17). Therefore, the need to harvest good quality samples not only from the primary tumor but also from the metastatic lesions will increase in the future (31). Consequently, surgical indications will follow this evolution and surgeons will become important partners of the translational process leading to a more personalized treatment.
Indication for VATS metastasectomy
A VATS approach can be considered when two criteria are met: (I) the surgical team must have sufficient experience with minimally invasive pulmonary resections, including anatomical resections, and with pre-operative localization; (II) patients must be adequately selected.
Both criteria should be evaluated by a multidisciplinary board prior to any therapy.
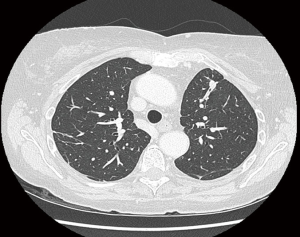
The quality of CT-scan imaging is crucial for a successful VATS pulmonary metastasectomy. Nowadays, thin slice 1-mm spiral CT-scan is recommended to analyze the entire lung volume during a single breath-hold, thus improving the accuracy of lung nodule detection by eliminating both the respiratory motion artifact and volume averaging. This recent imaging modality seems as efficient as direct bimanual palpation to detect lung metastases, with negative predictive values reaching 96% (7). Historically, several studies demonstrated that bilateral lung palpation increases the rate of identification of pulmonary nodules in 16% to 46% of patients compared to the preoperative CT-scan (24,32-34). However, most of these studies were performed on helical CT-scans with section reconstructions of 5-mm thickness or more. The new thin-slice CT-scans, on the other hand, can detect nodules of less than 5 mm in diameter. This increases the rate of false positive intra-pulmonary nodules, given that up to 50% of these nodules are benign. The concordance between radiological imaging and pathological findings was analyzed by the Spanish prospective registry of lung metastasectomy (35). Solitary nodules were present in 73% of colorectal cancer patients who underwent thoracotomy and bimanual palpation with radiological and pathological agreement in 95% of cases. In another series, only 7% of patients with a single nodule on pre-operative CT-scan presented more lesions during thoracotomy, of which 84% were malignant (23). Thus, these recent results suggest that the VATS approach is a suitable option at least for patients with a single lesion on pre-operative images.
Finally, the exact clinical significance of missing nodules has not been clearly established in the literature. Nodules not palpated during VATS procedure should not necessarily be interpreted as incomplete resections. The term “undetectable lesion” seems more appropriate since no data indicates how missing lung metastatic lesions will evolve over time, if left behind (3). These lesions do not necessarily lead to a similarly unfavorable prognosis as an incompletely resected nodule. To the best of our knowledge, there are no previous or ongoing prospective randomized trials comparing VATS with open metastasectomy. To date, most conclusions rely on retrospective studies. Yet, due to the aforementioned elements, we believe that in situations of single nodule on pre-operative CT-scans, a VATS approach should be preferred.
Optimal approach for VATS metastasectomy
Since the first surgical series of VATS resection for metastatic pulmonary lesions published in 1993 (36), the choice of surgical access is still debated. A wide spectrum of interventions has been described in the context of pulmonary metastasectomy, ranging from multiport VATS with or without utility incision, uniportal VATS, hybrid approach combining VATS and open approach, robotic-assisted technique or subxiphoid VATS (5,6). The principle of VATS is to avoid rib spreading and to perform complete resection with correct identification of the lesions.
We generally use a 3-ports technique with an inferior camera port, a posterior working port, and an anterior working port that can be extended to an utility incision (12). If the risk of conversion is high, then the VATS incisions should be located so as to overlap those of the anticipated thoracotomy. The goal of pulmonary metastasectomy remains a complete resection of lung nodules while sparing as much as possible lung parenchyma. Wedge resection with staplers is the preferred approach during VATS, because metastases are generally peripheral and easily accessible for wedge resection. During the initial experience of VATS approaches, local recurrences were reported both at original resection sites and at thoracoscopic port sites. These complications were published before the 2000s when no extraction bags were available (4). Moreover, macroscopic examination of the stapler line in connection with the metastasis is mandatory and, in case of doubt, a frozen section should be performed. Recently, laser resection has been proposed as an alternative to stapler resection to spare healthy parenchyma (37). The technique is currently under investigation and only a few centers have reported on their experience.
The rate of anatomical resection during VATS metastasectomy seems to increase when comparing to other historical open surgical series. In a large series of 154 VATS metastasectomies, complete resection was achieved by wedge resection in 110 patients, by lobectomy in 43 and by pneumonectomy in 1 patient (38). These results reflect the fact that some deeply located nodules are more easily amenable to a VATS lobectomy than to a complex segmentectomy, which is more easily performed by thoracotomy. Anatomical segmentectomy could be an alternative to lobectomy in cases of centrally located or multiple lesions in the same segment, although they are rarely chosen for the treatment of PMs, and only account for 3% to 23% of all pulmonary metastasectomies (39). This parenchymal-sparing technique is nonetheless particularly interesting in the context of lung metastasectomy where local recurrence and repeated resections are common. Segmentectomies can be technically challenging, but are gaining popularity among the VATS community since recent studies suggest that complex segmentectomies by VATS can be performed safely with acceptable morbidity and low mortality even during initial experiences (40). Interestingly, anatomical resections (segmentectomy or lobectomy) of colo-rectal lung metastasis have been reported to increase survival rates in comparison with non-anatomical resection in the Spanish multicenter prospective study for colorectal cancer (55 vs. 28.3 months) or for patient harboring KRAS mutations (101 vs. 45 months, P=0.02) (41,42). These results suggest that major resections could be justified for selected patient with larger or central PMs.
A VATS procedure may result in insufficient surgical margins leading to subsequent local recurrence. This is particularly true for VATS-based wedges, when the lesions are deeply located or large. Several methods are now routinely implemented to facilitate the peri-operative detection of nodules during VATS: hook wire localization; methylene blue or radioactive injection; sonography. We have previously reported our experience with 181 patients who underwent VATS resection of solitary nodules of unknown origin with pre-operative localization by hook wire (8). In our experience, this procedure was associated with low morbidity rate (pneumothorax requiring drainage in 2.3% of patients; migration of the hook wire in 3.7% of patients) and adequate localization of the nodule (96.4%). However, these procedures can be used only for radiologically detectable lesions. Thus, a conversion to thoracotomy should be performed when some lesions detected by CT-scan cannot be identified during surgery or clear surgical margins cannot be achieved. The rate of conversion has been estimated to be up to 20% (43). In our opinion, lung preservation should be favored in each situation, even for deeply located lesions. Therefore, a conversion to thoracotomy should not be considered as a failure but rather as a sign of mature surgical judgment.
Oncological results of VATS metastasectomy
To date, there are no randomized clinical trials comparing the outcome of lung metastasectomy performed via minimally invasive VATS approaches or via standard open techniques (3). Nevertheless, several single-center retrospective studies describe their experience with VATS compared to open pulmonary metastasectomy. In 2002, Mutsaerts et al. compared VATS and open approaches. He reported equivalent oncological outcomes for various tumor types in terms of recurrence rate (37% vs. 41%) and 2-year survival (70% vs. 68%) for a limited number of patients (8 vs. 12 patients) (43). Nakajima et al. reported 143 pulmonary metastasectomy performed during 1987 to 2005 either by VATS or by thoracotomy for metastatic colorectal cancer (44). The 5-year recurrence-free rate after a first pulmonary metastasectomy was 34.4% in the VATS group and 21.1% in the open group (P=0.047). The 5-year OS rate was 49.3% and 39.5% in the thoracoscopic and the open group respectively, without significant differences. Since then, many comparative studies showed equivalent oncological outcomes between VATS and open surgical approaches in term of local recurrence (VATS: 9–40% vs. open surgery: 13–53%) or 5-year survival (VATS: 49–69% vs. open surgery: 34–70%).
However, VATS procedures decreased morbidity and shortened the length of hospital stay for various primary tumors (45-49). More recently, the metastatic lung tumor study group of Japan published the largest series comparing VATS to thoracotomy for pulmonary metastasectomy in patients suffering from metastatic colorectal cancer (50). This multicentric (25 institutions) retrospective study included 1,047 patients who underwent pulmonary resection following a primary CRC either by VATS or thoracotomy. After computing a propensity score, the authors found a better survival rate in the VATS group (stratified log-rank test: P=0.0353). Dong et al. performed a meta-analysis of 6 retrospective studies including a total of 546 patients. They compared the survival rates between open (n=311) and VATS (n=235) pulmonary metastasectomy (51). VATS and open approaches resulted in significant differences neither in the 1-, 3- and 5-year survival rates nor in the 1-year disease-free survival rate. However, there was a statistically significant difference between the 3-year disease-free survival rate (P=0.04), in favor of the open group. Two recent systematic reviews, published in 2015 and including 8 studies each, analyzed the differences in overall survival and disease-free survival for patients who underwent pulmonary metastasectomy by thoracoscopy and thoracotomy (16,52). No statistically significant differences could be evidenced in either case. As a result, these articles concluded by promoting VATS as a suitable alternative for PMs.
Over time, the few series reporting single-center experience for VATS metastasectomy showed a progressive improvement in overall survival (Table 2). For instance, Landreneau et al. reported 80 VATS wedge resections of colorectal metastasis with no mortality, no major post-operative complications rate and short length of hospitalization (mean duration: 4.5 days) (10). This initial experience showed 24% of ipsilateral recurrence and a 5-year survival rate of 30.8%. Recently, Maeda et al. published 131 VATS resections (wedge: 103; lobectomy or segmentectomy: 28) for colorectal PMs (13). The 5-year survival rate and disease-free survival rate were 62.8% and 34.3%, respectively. Pulmonary recurrence was documented in 23.6% of patients. In 2017, Sun et al. reported an increased rate of anatomical resections performed by VATS for pulmonary metastasis in 154 patients between 2005 and 2015 (wedge: 103; segmentectomy: 5 and lobectomy: 46) (14). The cumulative 5-year overall survival rate after VATS pulmonary metastasectomy from CRC was 71.3%. Similarly, Lo Faso and colleagues published a single-center series of 212 VATS lung metastasectomy performed on 164 patients from 2000 to 2011 (38), which was updated in 2017 (15). They performed 22 segmentectomies, 54 lobectomies and 1 pneumonectomy for 133 wedge resections. The mean hospital stay was 5 days, and there was no post-operative death and a low rate of major complications (2.4%). There were no significant differences in long term survival between patients who underwent wedge resection in comparison to those who underwent anatomical resections. In a consecutive series of 77 patients undergoing VATS metastasectomy, we reported a complete resection in all patients: 93% were operated by wedge and 7% by anatomical resection. Overall survival (54% at 5 years) and pulmonary recurrence rate (30%) were comparable to those reported from traditional open surgical series (12).
Table 2
| Study | Number of patients | Primary tumor type | Number of metastases | Surgical procedure | Hospital stay (days) | Ipsilateral recurrence | 5-year overall-survival |
|---|---|---|---|---|---|---|---|
| Landreneau |
80 | Colorectal | Unique: 60; multiple: 20 | Wedge: 80 | 4.5±2.2 | 24% | 30.8% |
| Saisho |
48 | Multiple | Unique: 36; multiple: 12 | Wedge. 41; seg/lob: 12 | NA | 13/48 | 47% |
| Abdelnour |
77 | Multiple | Unique: 63; multiple 14 | Wedge 72; lobectomies 5 | 3 [2 |
10% | 54% |
| Maeda |
131 | Colorectal | Unique 77; multiple 54 | Wedge 103; seg/lob 28 | N/A | 31/131 | 62.8% |
| Sun |
154 | Colorectal | Unique: 125; multiple; 29 | Wedge 103segmentectomies 5; lobectomies 46 | NA | NA | 71.3% |
| Guerini |
224 | Multiple | Unique 127; multiple 97 | Wedge 155; lobectomies 68; pneumonectomy 1 | 5 [4 |
NA | 60.6% |
VATS, video-assisted thoracic surgery.
In light of these comparative studies and meta-analyses, both open surgery and VATS approaches seem to result in equivalent oncological outcomes in terms of local control and long-term survival even in the absence of formal bimanual palpation. Moreover, the recurrence rate within the operated lung seems to be equivalent with both techniques. In other words, the “radicality” of thoracotomy does not guarantee a reduction of local or distant recurrence rates.
Repeated VATS metastasectomy
Recurrent pulmonary metastasis is a situation occurring in almost 50% of cases (53). Some authors report that repeated VATS pulmonary metastasectomy is safe and effective to manage such recurrent lesions (12). The indications for redo surgery are identical to the indications for initial surgery. However, only a limited number of patients will fulfill the criteria for repeated resections due to the invasion of other organs or poor residual lung capacity.
In most cases, post-operative recurrences are found in the contra-lateral lung or in other extra-thoracic sites. Interestingly, local recurrence rates within the operated lung have been reported to be equivalent between VATS and open techniques suggesting that radicality of the surgery could not be significantly improved by bimanual palpation. In our series of 77 patients, an ipsilateral recurrence occurred in only 8 patients after VATS metastasectomy. Seven of them could benefit from a redo surgery, performed by VATS procedure in the vast majority of cases (5/7) (12). Initial VATS metastasectomy are associated with fewer intrapleural adherences, decreased operative time and less important intra-operative blood loss in comparison with an initial open approach (54). Since VATS procedures induce fewer adhesions and chest wall sequelae than thoracotomies, repeated VATS procedures are easier to perform and are better tolerated than repeated thoracotomies (Figures 1,2).

Lymphadenectomy and VATS metastasectomy
Mediastinal lymph node dissection or sampling is not routinely performed during lung metastasectomy. While survival of pulmonary metastatic patients is affected by metastatic invasion of the lymph nodes, it remains unclear if systematic lymph node dissection during pulmonary metastasectomy brings any advantage in terms of local recurrence or survival. In 2008, the ESTS survey reported that 56% of surgeons performed mediastinal sampling during lung metastasectomy, but only 13% did a complete dissection and 32% of them did not carry out any lymph node biopsy (26). The incidence of mediastinal lymph node involvement in the context of PMs has been reported to range between 12% and 32%. Survival was also correlated with lymph node invasion. Pfannschmidt et al. performed a systematic lymph node dissection during pulmonary metastasectomy on 245 patients, and they found that 32% of hilar or mediastinal lymph nodes were invaded (56). The median survival was 64 months for patients without nodal metastases and 33 and 21 months for patients with hilar and mediastinal metastases respectively. Hamaji et al. published a retrospective study including 518 lung metastasectomies from colorectal cancer (57). They compared three groups: no lymphadenectomy (199 patients), negative lymph node involvement (279 patients) and positive lymph node involvement (40 patients). Median survival of patients without lymph node invasion was 58.5 months and decreased to 34 months when the lymph nodes were invaded. Patients with unknown lymph node status had a median survival rate of 52 months. Interestingly, these results were statistically significant. The Spanish prospective registry of colorectal cancer PMs analyzed also the survival rate of 250 patients after lymph node dissection (58). Their 5-year survival rate was 58% in the absence of lymph node involvement, 25% when lymph nodes were invaded and 44% with unknown lymph node status.
These results suggest that lymph node assessment carries an important prognostic factor and could carry a therapeutic role, which needs to be clarified.
The complete mediastinal lymphadenectomy may increase the operative time, but is rarely correlated with high morbidity. Moreover, the efficacy of VATS lymphadenectomy in early stage lung cancer has been shown to be equivalent to thoracotomy in terms of number of nodes and nodal stations dissected (59,60). Although survival benefits after lymph node dissection remain unclear, complete mediastinal lymphadenectomy or sampling should be considered during VATS pulmonary metastasectomy to achieve accurate staging and guide subsequent adjuvant treatment.
Conclusions
To date, many retrospective and prospective studies support the idea that pulmonary metastasectomy has a curative role provided that complete resection is achieved. Although a VATS approach limits bimanual palpation and potential additional resection of nodules not identified by pre-operative imaging, oncological survival and local recurrence rates seem equivalent to those of thoracotomy for patients with a limited number of metastases. Additional advantages include decreased morbidity and length of hospitalization. Thus, VATS approach should be recommended for solitary PMs both to confirm the diagnosis and for curative purposes. Mediastinal lymph node dissection or sampling could be performed during VATS procedure, but needs to be assessed by further studies. Of course, thoracotomy should still be recommended for multiple pulmonary lesions to achieve complete resection of all nodules. In experienced centers, personalized management could be proposed based on imaging techniques to potentially offer VATS resections for multiple lesions. VATS approach can also be considered valuable if careful follow-up is planned so that repeated resection of newly discovered nodules can be performed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Visualized Surgery for the series “Advancement in the Surgical Treatment of Pulmonary Metastasis”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jovs.2019.04.03). The series “Advancement in the Surgical Treatment of Pulmonary Metastasis” was commissioned by the editorial office without any funding or sponsorship. MG served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- . Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. The International Registry of Lung Metastases. J Thorac Cardiovasc Surg 1997;113:37-49. [Crossref]
- Downey RJ. Surgical treatment of pulmonary metastases. Surg Oncol Clin N Am 1999;8:341. [Crossref] [PubMed]
- Perentes JY, Krueger T, Lovis A, et al. Thoracoscopic resection of pulmonary metastasis: current practice and results. Crit Rev Oncol Hematol 2015;95:105-13. [Crossref] [PubMed]
- Downey RJ, McCormack P, LoCicero J 3rd. Dissemination of malignant tumors after video-assisted thoracic surgery: a report of twenty-one cases. The Video-Assisted Thoracic Surgery Study Group. J Thorac Cardiovasc Surg 1996;111:954-60. [Crossref] [PubMed]
- Mineo TC, Sellitri F, Fabbi E, et al. Uniportal non-intubated lung metastasectomy. J Vis Surg 2017;3:118. [Crossref] [PubMed]
- Mineo TC, Ambrogi V, Paci M, et al. Transxiphoid bilateral palpation in video-assisted thoracoscopic lung metastasectomy. Arch Surg 2001;136:783-8. [Crossref] [PubMed]
- Kang MC, Kang CH, Lee HJ, et al. Accuracy of 16-channel multi-detector row chest computed tomography with thin sections in the detection of metastatic pulmonary nodules. Eur J Cardiothorac Surg 2008;33:473-9. [Crossref] [PubMed]
- Hanauer M, Perentes JY, Krueger T, et al. Pre-operative localization of solitary pulmonary nodules with computed tomography-guided hook wire: report of 181 patients. J Cardiothorac Surg 2016;11:5. [Crossref] [PubMed]
- Perentes JY, Zellweger M, Gonzalez M. Personalized surgery for the management of pulmonary metastasis. J Thorac Dis 2018;10:52-5. [Crossref] [PubMed]
- Landreneau RJ, De Giacomo T, Mack MJ, et al. Therapeutic video-assisted thoracoscopic surgical resection of colorectal pulmonary metastases. Eur J Cardiothorac Surg 2000;18:671-6; discussion 676-7. [Crossref] [PubMed]
- Saisho S, Nakata M, Sawada S, et al. Evaluation of video-assisted thoracoscopic surgery for pulmonary metastases: 11-years of experience. Surg Endosc 2009;23:55-61. [Crossref] [PubMed]
- Abdelnour-Berchtold E, Perentes JY, Ris HB, et al. Survival and Local Recurrence After Video-Assisted Thoracoscopic Lung Metastasectomy. World J Surg 2016;40:373-9. [Crossref] [PubMed]
- Maeda R, Suda T, Hachimaru A, et al. Video-Assisted Thoracoscopic Pulmonary Metastasectomy in Patients with Colorectal Cancer: A Recent 10-Year Single-Institution Experience. World J Surg 2016;40:1318-23. [Crossref] [PubMed]
- Sun F, Chen L, Shi M, et al. Prognosis of video-assisted thoracoscopic pulmonary metastasectomy in patients with colorectal cancer lung metastases: an analysis of 154 cases. Int J Colorectal Dis 2017;32:897-905. [Crossref] [PubMed]
- Guerrini GP, Lo Faso F, Vagliasindi A, et al. The Role of Minimally Invasive Surgery in the Treatment of Lung Metastases. J Invest Surg 2017;30:110-5. [Crossref] [PubMed]
- Meng D, Fu L, Wang L, et al. Video-assisted thoracoscopic surgery versus open thoracotomy in pulmonary metastasectomy: a meta-analysis of observational studies. Interact Cardiovasc Thorac Surg 2016;22:200-6. [Crossref] [PubMed]
- Moorcraft SY, Jones T, Walker BA, et al. Molecular profiling of colorectal pulmonary metastases and primary tumours: implications for targeted treatment. Oncotarget 2017;8:64999-5008. [Crossref] [PubMed]
- Rusch VW. Pulmonary metastasectomy. Current indications. Chest 1995;107:322S-31S. [Crossref] [PubMed]
- Sleeman JP. Metastasis: understanding is the beginning of order in chaos. Semin Cancer Biol 2012;22:173. [Crossref] [PubMed]
- Fidler IJ. The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer 2003;3:453-8. [Crossref] [PubMed]
- Younes RN, Fares AL, Gross JL. Pulmonary metastasectomy: a multivariate analysis of 440 patients undergoing complete resection. Interact Cardiovasc Thorac Surg 2012;14:156-61. [Crossref] [PubMed]
- Casiraghi M, De Pas T, Maisonneuve P, et al. A 10-year single-center experience on 708 lung metastasectomies: the evidence of the "international registry of lung metastases". J Thorac Oncol 2011;6:1373-8. [Crossref] [PubMed]
- Ludwig C, Cerinza J, Passlick B, et al. Comparison of the number of pre-, intra- and postoperative lung metastases. Eur J Cardiothorac Surg 2008;33:470-2. [Crossref] [PubMed]
- Eckardt J, Licht PB. Thoracoscopic versus open pulmonary metastasectomy: a prospective, sequentially controlled study. Chest 2012;142:1598-602. [Crossref] [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
- Internullo E, Cassivi SD, Van Raemdonck D, et al. Pulmonary metastasectomy: a survey of current practice amongst members of the European Society of Thoracic Surgeons. J Thorac Oncol 2008;3:1257-66. [Crossref] [PubMed]
- Jegatheeswaran S, Satyadas T, Sheen AJ, et al. Thoracic surgical management of colorectal lung metastases: a questionnaire survey of members of the Society for Cardiothoracic Surgery in Great Britain and Ireland. Ann R Coll Surg Engl 2013;95:140-3. [Crossref] [PubMed]
- Caristo JM, Tian DH, Yan TD. Pulmonary metastasectomy: a cross sectional survey. J Thorac Dis 2018;10:3757-66. [Crossref] [PubMed]
- Handy JR, Bremner RM, Crocenzi TS, et al. Expert Consensus Document on Pulmonary Metastasectomy. Ann Thorac Surg 2019;107:631-49. [Crossref] [PubMed]
- Bellier J, Perentes JY, Abdelnour-Berchtold E, et al. A plea for thoracoscopic resection of solitary pulmonary nodule in cancer patients. Surg Endosc 2017;31:4705-10. [Crossref] [PubMed]
- Schirren J, Schirren M, Lampl L, et al. Surgery for pulmonary metastases: quo vadis? Eur J Cardiothorac Surg 2017;51:408-10. [Crossref] [PubMed]
- Cerfolio RJ, McCarty T, Bryant AS. Non-imaged pulmonary nodules discovered during thoracotomy for metastasectomy by lung palpation. Eur J Cardiothorac Surg 2009;35:786-91; discussion 791. [Crossref] [PubMed]
- McCormack PM, Bains MS, Begg CB, et al. Role of video-assisted thoracic surgery in the treatment of pulmonary metastases: results of a prospective trial. Ann Thorac Surg 1996;62:213-6; discussion 216-7. [Crossref] [PubMed]
- Margaritora S, Porziella V, D'Andrilli A, et al. Pulmonary metastases: can accurate radiological evaluation avoid thoracotomic approach? Eur J Cardiothorac Surg 2002;21:1111-4. [Crossref] [PubMed]
- Marron MC, Lora D, Gamez P, et al. Agreement Between Computed Tomography and Pathologic Nodule Counts in Colorectal Lung Metastases. Ann Thorac Surg 2016;101:259-65. [Crossref] [PubMed]
- Dowling RD, Keenan RJ, Ferson PF, et al. Video-assisted thoracoscopic resection of pulmonary metastases. Ann Thorac Surg 1993;56:772-5. [Crossref] [PubMed]
- Mc Loughlin JB, O'Sullivan KE, Brown RH, et al. Limax Nd:YAG laser-assisted thoracoscopic resection of pulmonary metastases; a single centre's initial experience. Ir J Med Sci 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Lo Faso F, Solaini L, Lembo R, et al. Thoracoscopic lung metastasectomies: a 10-year, single-center experience. Surg Endosc 2013;27:1938-44. [Crossref] [PubMed]
- Berry MF. Role of segmentectomy for pulmonary metastases. Ann Cardiothorac Surg 2014;3:176-82. [PubMed]
- Bedat B, Abdelnour-Berchtold E, Krueger T, et al. Clinical outcome and risk factors for complications after pulmonary segmentectomy by video-assisted thoracoscopic surgery: results of an initial experience. J Thorac Dis 2018;10:5023-9. [Crossref] [PubMed]
- Renaud S, Seitlinger J, Lawati YA, et al. Anatomical Resections Improve Survival Following Lung Metastasectomy of Colorectal Cancer Harboring KRAS Mutations. Ann Surg 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Hernandez J, Molins L, Fibla JJ, et al. Role of major resection in pulmonary metastasectomy for colorectal cancer in the Spanish prospective multicenter study (GECMP-CCR). Ann Oncol 2016;27:850-5. [Crossref] [PubMed]
- Mutsaerts EL, Zoetmulder FA, Meijer S, et al. Long term survival of thoracoscopic metastasectomy vs metastasectomy by thoracotomy in patients with a solitary pulmonary lesion. Eur J Surg Oncol 2002;28:864-8. [Crossref] [PubMed]
- Nakajima J, Murakawa T, Fukami T, et al. Is thoracoscopic surgery justified to treat pulmonary metastasis from colorectal cancer? Interact Cardiovasc Thorac Surg 2008;7:212-6; discussion 216-7. [Crossref] [PubMed]
- Nakas A, Klimatsidas MN, Entwisle J, et al. Video-assisted versus open pulmonary metastasectomy: the surgeon's finger or the radiologist's eye? Eur J Cardiothorac Surg 2009;36:469-74. [Crossref] [PubMed]
- Gossot D, Radu C, Girard P, et al. Resection of pulmonary metastases from sarcoma: can some patients benefit from a less invasive approach? Ann Thorac Surg 2009;87:238-43. [Crossref] [PubMed]
- Carballo M, Maish MS, Jaroszewski DE, et al. Video-assisted thoracic surgery (VATS) as a safe alternative for the resection of pulmonary metastases: a retrospective cohort study. J Cardiothorac Surg 2009;4:13. [Crossref] [PubMed]
- Chao YK, Chang HC, Wu YC, et al. Management of lung metastases from colorectal cancer: video-assisted thoracoscopic surgery versus thoracotomy--a case-matched study. Thorac Cardiovasc Surg 2012;60:398-404. [Crossref] [PubMed]
- Hou Z, Zhang H, Gui L, et al. Video-assisted thoracoscopic surgery versus open resection of lung metastases from colorectal cancer. Int J Clin Exp Med 2015;8:13571-7. [PubMed]
- Murakawa T, Sato H, Okumura S, et al. Thoracoscopic surgery versus open surgery for lung metastases of colorectal cancer: a multi-institutional retrospective analysis using propensity score adjustmentdagger. Eur J Cardiothorac Surg 2017;51:1157-63. [Crossref] [PubMed]
- Dong S, Zhang L, Li W, et al. Evaluation of video-assisted thoracoscopic surgery for pulmonary metastases: a meta-analysis. PLoS One 2014;9:e85329 [Crossref] [PubMed]
- Cheang MY, Herle P, Pradhan N, et al. Video-assisted thoracoscopic surgery versus open thoracotomy for pulmonary metastasectomy: a systematic review. ANZ J Surg 2015;85:408-13. [Crossref] [PubMed]
- Gonzalez M, Ris HB, Krueger T, et al. Colorectal cancer and thoracic surgeons: close encounters of the third kind. Expert Rev Anticancer Ther 2012;12:495-503. [Crossref] [PubMed]
- Kondo R, Hamanaka K, Kawakami S, et al. Benefits of video-assisted thoracic surgery for repeated pulmonary metastasectomy. Gen Thorac Cardiovasc Surg 2010;58:516-23. [Crossref] [PubMed]
- Sauvain MO, Abdelnour-Berchtold E, Zellweger M, et al. Video showing a redo VATS metastasectomy after two previous multiple wedge metastasectomies by VATS in the left side. Asvide 2019;6:125. Available online: http://www.asvide.com/article/view/31401
- Pfannschmidt J, Klode J, Muley T, et al. Nodal involvement at the time of pulmonary metastasectomy: experiences in 245 patients. Ann Thorac Surg 2006;81:448-54. [Crossref] [PubMed]
- Hamaji M, Cassivi SD, Shen KR, et al. Is lymph node dissection required in pulmonary metastasectomy for colorectal adenocarcinoma? Ann Thorac Surg 2012;94:1796-800. [Crossref] [PubMed]
- Call S, Rami-Porta R, Embun R, et al. Impact of inappropriate lymphadenectomy on lung metastasectomy for patients with metastatic colorectal cancer. Surg Today 2016;46:471-8. [Crossref] [PubMed]
- Detterbeck FC, Grodzki T, Gleeson F, et al. Imaging requirements in the practice of pulmonary metastasectomy. J Thorac Oncol 2010;5:S134-9. [Crossref] [PubMed]
- Garcia-Yuste M, Cassivi S, Paleru C. Thoracic lymphatic involvement in patients having pulmonary metastasectomy: incidence and the effect on prognosis. J Thorac Oncol 2010;5:S166-9. [Crossref] [PubMed]
Cite this article as: Sauvain MO, Abdelnour-Berchtold E, Zellweger M, Perentes JY, Gonzalez M. Why choosing a video-assisted thoracic surgery approach for pulmonary metastasectomy? J Vis Surg 2019;5:46.


