Pyloric drainage: techniques and controversies
Introduction
Although there are several methods for reconstruction following esophagectomy for malignancy, gastrointestinal continuity is most commonly achieved by pulling the entire or tubularized stomach into the chest or neck by way of the posterior mediastinum. Lymph node dissection and transection of the stomach inherently are associated with bilateral vagotomies, leading to a degeneration of the myenteric plexus. This results in the inability to relax the pyloric sphincter leading to delayed gastric emptying (DGE) and gastric outlet obstruction (GOO) (1,2).
DGE and GOO occur in 10–50% of patients after esophageal resection for malignancy (3). Symptoms include early satiety, postprandial discomfort, dysphagia, aspiration, and regurgitation. This leads to decreased patient satisfaction, increased risk of aspiration and prolonged hospital stay (2). Indeed, the most-feared complication is that gastric emptying disorders lead to an aspiration pneumonia, which can significantly affect a patient’s mortality (4).
The symptoms of DGE have classically been managed conservatively. Dietary changes including small, frequent meals low in fat and fiber are often recommended. Erythromycin, which works as an agonist to motilin receptors in the pylorus, has been shown to be effective at increasing the amplitude of antropyloric contractions. If symptoms persist despite dietary changes or medications, endoscopic dilation can be considered and is effective in 70–97% of patients. However, the only “intervention” that has been proven to reliably and consistently improve symptoms of DGE and GOO in this population is time (1).
Controversy of pyloric drainage
The decision to routinely perform prophylactic pyloroplasty on these patients remains controversial as the results of studies are mixed. Advocates cite reduced incidence of DGE, GOO, anastomotic leak, and aspiration. Opponents argue an increased incidence of dumping syndrome and bile reflux (3). Pyloroplasty with esophagectomy was initially presumed to be necessary based on prior experience with truncal vagotomies after ulcer surgeries in which a denervated stomach was thought to result in GOO unless pyloric drainage was performed concomitantly (5).
The trend toward using pyloroplasty routinely during esophagectomies came after the landmark study by Fok et al. which prospectively randomized 100 patients to esophagectomy with pyloroplasty and 100 patients to no pyloroplasty. They concluded that there was a statistically significant increase incidence of DGE in the pyloroplasty group with no increase in complications (6). This was further corroborated by a meta-analysis in 2002 by Urschel et al., which included 9 randomized controlled trials (RCTs) with a total of 553 patients. This analysis showed a statistically significant reduction in the occurrence of early GOO, but no difference in respiratory complications, failure to thrive, or long-term GOO with the performance of a pyloroplasty or which pyloric drainage procedure (7). Similarly, another meta-analysis in 2007 by Khan et al. added 6 RCTs to the previously mentioned 2002 meta-analysis. This, again, demonstrated that pyloroplasty reduces the incidence of early postoperative GOO, but showed no difference in pulmonary complications, anastomotic leaks, or operative mortality (8).
More recent analyses of retrospective studies have failed to demonstrate a similar benefit of pyloroplasty. A 2014 systematic review by Gaur et al. examined four retrospective studies published between 2007 and 2011, including a total of 668 patients. This study demonstrated a non-significant trend for DGE and biliary reflux without a demonstrable effect on the incidence of dumping syndrome and no correlation with anastomotic leak, pulmonary complications, length of stay, or mortality. Overall, the authors were unable to provide evidence that there is any benefit to prophylactic pyloroplasty (5). Another retrospective study looked at 198 patients and divided them into three groups: those without pyloric drainage, those with pyloromyotomy, and those with pyloroplasty. It showed no difference in mortality, leak, hospital stay. or antegrade flow of contrast by gastrografin swallow. However, the group that underwent pyloric drainage suffered significantly more reflux esophagitis and bile reflux than those who had no pyloric drainage procedure (4).
Much of the controversy that exists today stems from the fact that the earlier studies strongly favored use of the whole stomach as the neoesophagus as opposed to the use of a tubularized stomach for reconstruction following esophagectomy. There remains no consensus on the use of pyloroplasty when a tubularized stomach is used as the neoesophagus. As such, it has been hypothesized that modern use of a tubularized gastric conduit as the neoesophagus has made the pyloroplasty obsolete (2). Further randomized control studies are necessary to make a definitive recommendation.
Techniques in pyloric drainage
The overarching goal of pyloric drainage procedures is to reduce the incidence of GOO and DGE and the risk of aspiration pneumonia. The standard of pyloric drainage procedure is the Heineke-Mikulicz pyloroplasty. However, multiple alternative procedures have been described in literature. These include the Finney pyloroplasty, Jaboulay antroduodenostomy, intraluminal and extraluminal circular stapled pyloroplasties, pyloromyotomy, botulinum toxin (BoTox) injection, and intraoperative pyloric stretch.
Heineke-Mikulicz pyloroplasty
We demonstrate a laparoscopic and robotically assisted modified Heineke-Mikulicz pyloroplasty. It can also be done open. For the laparoscopic video (see Figure 1), a longitudinal seromuscular incision is made centered at the pyloric ring using electrocautery. Once the myotomy is completed, stay sutures are placed to keep the pylorus open. A single-layer closure is performed to close the pylorus transversely. While this can be done using interrupted sutures, a running barbed suture (V-Loc; Medtronic/Covidien, New Haven, CT, USA) works as well. The pyloroplasty is then covered with a tongue of omentum with 2 or 3 holding stitches to cover the pylorus, much like a Graham patch.

The robotically assisted Heineke-Mikulicz pyloroplasty (see Figure 2) uses a longitudinal seromuscular incision through the center of the pyloric ring using electrocautery. Once the myotomy is completed, stay sutures are placed to keep the pylorus open. A single-layer closure is performed to close the pylorus transversely. In this it is done using braided interrupted sutures and there is no modified Graham patch.

Although not see in this video, the pyloroplasty can be covered with a tongue of omentum with 2 or 3 holding stitches to cover the pylorus, much like a Graham patch. A modified version of this technique using a linear stapler for closure has also been described.
Finney and Jaboulay pyloroplasties
Though less common than the Heineke-Mikulicz pyloroplasty, the Finney or Jaboulay techniques are also options for pyloric drainage. The Finney pyloroplasty is a side-to-side gastroduodenostomy which includes the pylorus. This technique is useful in a J-shaped stomach whose pylorus is retracted and fixed. The procedure begins with Kocherization of the duodenum. Traction sutures are placed at superior aspect of the pylorus, as well as 10 cm distally and proximally along the duodenum and greater curvature of the stomach. A running seromuscular (Cushing) suture connecting the stomach to the duodenum is then undertaken to form the outermost layer in the two-layer closure of the back wall. An incision is made 5 cm from the pylorus in either the stomach or duodenum and extended equidistant beyond to the opposite side of the sphincter. A running transmural (Connell) suture completes the two-layer closure of the back wall and is continued anteriorly to form the innermost layer of the double layer closure of the front wall. The seromuscular suture is then continued in an interrupted (Lembert) fashion to reinforce the front wall and complete the two-layer closure (11).
The Jaboulay technique is used when the pylorus is too scarred or inflamed. The procedure is similar to the Finney pyloroplasty except that the pylorus is preserved. A version of this procedure can be undertaken using linear staplers. A side-to-side antroduodenostomy can be created by introducing arms of a linear stapler through an antrotomy and duodenotomy site. The remaining enterotomy is then subsequently closed using a linear stapler as well (11).
Circular stapler pyloroplasties
Pyloroplasties performed using a circular stapler have been shown to be safe, efficient, and equally efficacious alternatives to the H-M pyloroplasty (12). Three methods have been described using the using the circular stapler: the trans-oral intraluminal, the trans-gastric intraluminal, and extraluminal approaches, with the latter two being able to be performed laparoscopically or open.
In the intraluminal approach, a partially opened 21-mm circular stapler is introduced into the stomach transorally or via gastrostomy made in the lesser curve of the stomach made during laparoscopic or open surgery. The circular stapler is then passed into the pyloric canal. Once the anvil has passed through the pylorus, the stapler is raised anteriorly to capture the anterior wall as it is closed. A 2-0 silk suture may be used to assist pulling the anterior wall into the stapler. A partial thickness bite is then taken to disrupt the muscularis externa leaving behind an intact serosa. This may be confirmed by endoscopy which will reveal keyhole-like deformity of the pylorus (12,13). In the transgastric approach, the gastrostomy site is typically excised with tubularization of the stomach (12).
The extraluminal approach begins by running a 2-0 suture in a perpendicular fashion through the anterior muscular layer of the pylorus. A 28-mm circular stapler is introduced through a trocar site in the left upper quadrant. The suture is then pulled up or fastened to the purse-string notch of the anvil bringing the anterior pyloric wall into the stapler which is subsequently closed and fired excising a longitudinal segment of the pylorus. An endoscope may be used during the procedure to ensure the inner mucosa remains intact (14).
Linear stapler pyloroplasty
A linear stapler may be used in the extraluminal approach as well. Described by Wu and Wu, two 1 cm traction sutures are placed midway along the anterior pylorus. This tissue is then brought up into a 4.8-mm linear stapler and resected in a perpendicular fashion (15).
Pyloromyotomy
Pyloromyotomy has been found to be an equally efficacious alternative to pyloroplasty for gastric drainage following esophagectomy (16). In the open approach, the pylorus is held between the thumb and index finger. Using a scalpel, a 1–2 cm longitudinal incision is made down to level of the mucosa, leaving it intact. A hemostat is then use to spread the muscle apart until the free edges move independently from one another. In the laparoscopic approach, monopolar cautery is used to dissect through the serosa and muscular layers of the viscera. Further release of the muscle fibers is achieved by twisting the Bovie side-to-side to the same conclusion (17). In the literature, endoscopic pyloromyotomies appear to be reserved for patients who develop GOO or DGE postoperatively as these procedures have not been described at the time of initial resection.
Injection of BoTox
Botulinum toxin (BoTox) injection has emerged as a nonsurgical means for pyloric drainage. This temporary measure (lasting up to 90–120 days) can be performed during endoscopic, laparoscopic, or open procedures. A small gauge needle is used to inject the toxin (20–25 U/mL) into all four quadrants of the pylorus leading to decreased acetylcholine release and smooth muscle relaxation (18,19).
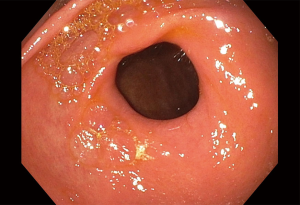
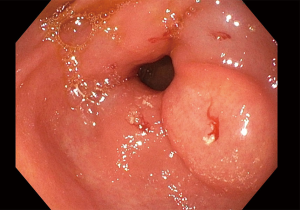
The procedure is performed by obtaining 200 units of botulinum toxin (normally comes in 100 unit aliquots) and diluting it to a total volume of 5 mL with normal saline. After completing a diagnostic endoscopy, the endoscope is positioned in the antrum such that the pylorus is within a direct view and as close to perpendicular to the endoscope as possible. Attach the syringe to an injection needle and prime outside the patient. Make note of how much volume is left in the syringe. Advance the injection needle through the working channel of the endoscope. Once it is in endoscopic view, select a first site of injection around the pylorus, approximately 1 cm from the aperture. Have the nurse or technician expose the needle, then advance the needle into the tissue with a swift jabbing motion. Once it is in place, inject 1 mL by pressing on the plunger and monitoring the volume using the marks on the syringe. After the volume is injected, retract the needle and move repeat this process a total of five times to inject the entire volume. This often requires replacement of the syringe with a second syringe full of sterile saline, as there will be 1–2 mL of injectate left within the tubing of the injection device (Figures 3,4).
Endoscopic dilation
A more durable endoscopic option than BoTox for patients who develop symptoms of GOO postoperatively is endoscopic dilation. This can either be performed with a balloon under direct bronchoscopy or savory dilator with fluoroscopy. EndoFLIP (Medtronic, Dublin, Ireland) can also be used prior to dilation to test pyloric distensibility to help determine if intervention will help. Savory dilation requires the endoscope to be passed into the duodenum and a guidewire placed under endoscopic guidance. The endoscope is then removed from the stomach, making sure to keep the wire in place via direct visualization fluoroscopically. Bougie dilators are then passed over the wire under fluoroscopy, again, making sure not to change the position of the wire. Selection of dilator type and size depends on operator preference and degree of stenosis. The rule of 3s states that after moderate resistance is met, no more than 3 dilators of progressively increasing diameter should be used in that session (20). Balloon dilation can be of varying sizes up to 15 mm. A more recent development is G-POEM or gastric per oral endoscopic myotomy which is more commonly used in gastroparesis but interest is growing in GOO after esophagectomy.
Comparison of techniques of pyloric drainage
As expected, there is just as much controversy regarding which pyloric drainage procedure is most efficacious considering the data to even perform it is equivocal.
Fok et al. recommended Heineke-Mikulicz pyloroplasty for pyloric drainage after esophagectomy (6). However, as previously discussed, there are many different methods for achieving pyloric drainage and a true “gold standard” has not been identified.
A retrospective, single-center, single-surgeon study by Cerfolio et al. looked at 221 patients who underwent Ivor-Lewis esophagectomy over a five-year period. DGE was assessed on postoperative day 4. Of this population, DGE was seen in 93% of patients who had pyloromyotomy, 96% of patients who had no intervention, 96% of patients who had pyloroplasty and 59% of patients who had botulinum toxin injection. This study demonstrated a statistically significant decrease in length of stay and operative time in patients who had BoTox injections. Botox injection had the advantage of promoting gastric emptying in the first few months after surgery. However, its effects dissipated within a few months and did not predispose the patients to long-term bile reflux (18).
Another retrospective review by Eldaif et al. evaluated 322 patients who underwent esophageal resection with botulin injection, pyloromyotomy or pyloroplasty. This study concluded that botulinum injection, while associated with decreased operative time, also increased postoperative reflux symptoms. Patients who underwent botulinum injection were more likely to require pro-motility agents or endoscopic dilation. In stark contrast to the results obtained by Cerfolio et al., these authors strongly recommended against botulinum injection as an alternative to standard drainage procedures (21).
Palmes et al. compared pyloromyotomy, pyloroplasty and no drainage procedure and concluded that no procedure should be done as there was no effect on rate of DGE postoperatively (4).
A randomized, multi-institutional study is needed to answer the question as to which pyloric drainage procedure is best.
Conclusions
Pyloric drainage after esophagectomy remains a subject of contentious debate in the literature. There is no strong recommendation as to whether pyloric drainage should be performed routinely as the literature is conflicting. If a surgeon would like to proceed with pyloric drainage, there are a variety of options including pyloroplasty, pyloromyotomy and injection of botulinum toxin. These techniques can be performed minimally invasively as well. Further studies are necessary to determine what procedure(s), if any, are necessary for patients undergoing esophagectomy for malignancy to prevent DGE.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Abbas E. Abbas) for the series “Robotic Surgery for Esophageal Cancer” published in Journal of Visualized Surgery. The article has undergone external peer review.
Conflicts of Interest: The series “Robotic Surgery for Esophageal Cancer” was commissioned by the editorial office without any funding or sponsorship. JFL reports paid consultant for Intuitive and Auris. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Poghosyan T, Gaujoux S, Chirica M, et al. Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J Visc Surg 2011;148:e327-35. [Crossref] [PubMed]
- Antonoff MB, Puri V, Meyers BF, et al. Comparison of pyloric intervention strategies at the time of esophagectomy: is more better? Ann Thorac Surg 2014;97:1950-7; discussion 1657-8.
- Fritz S, Feilhauer K, Schaudt A, et al. Pylorus drainage procedures in thoracoabdominal esophagectomy - a single-center experience and review of the literature. BMC Surg 2018;18:13. [Crossref] [PubMed]
- Palmes D, Weilinghoff M, Colombo-Benkmann M, et al. Effect of pyloric drainage procedures on gastric passage and bile reflux after esophagectomy with gastric conduit reconstruction. Langenbecks Arch Surg 2007;392:135-41. [Crossref] [PubMed]
- Gaur P, Swanson SJ. Should we continue to drain the pylorus in patients undergoing an esophagectomy? Dis Esophagus 2014;27:568-73. [Crossref] [PubMed]
- Fok M, Cheng SW, Wong J. Pyloroplasty versus no drainage in gastric replacement of the esophagus. Am J Surg 1991;162:447-52. [Crossref] [PubMed]
- Urschel JD, Blewett CJ, Young JE, et al. Pyloric drainage (pyloroplasty) or no drainage in gastric reconstruction after esophagectomy: a meta-analysis of randomized controlled trials. Dig Surg 2002;19:160-4. [Crossref] [PubMed]
- Khan OA, Manners J, Rengarajan A, et al. Does pyloroplasty following esophagectomy improve early clinical outcomes? Interact Cardiovasc Thorac Surg 2007;6:247-50. [Crossref] [PubMed]
- Himmler A, Holliday T, Khaitan PG, et al. Laparoscopic pyloromyotomy. Asvide 2019;6:194. Available online: http://www.asvide.com/article/view/32804
- Himmler A, Holliday T, Khaitan PG, et al. Robotically assisted pyloromyotomy. Asvide 2019;6:195. Available online: http://www.asvide.com/article/view/32805
- Søreide K, Sarr MG, Søreide JA. Pyloroplasty for benign gastric outlet obstruction--indications and techniques. Scand J Surg 2006;95:11-6. [Crossref] [PubMed]
- Oezcelik A, DeMeester SR, Hindoyan K, et al. Circular stapled pyloroplasty: a fast and effective technique for pyloric disruption during esophagectomy with gastric pull-up. Dis Esophagus 2011;24:423-9. [Crossref] [PubMed]
- Hibbard ML, Dunst CM, Swanström LL. Laparoscopic and endoscopic pyloroplasty for gastroparesis results in sustained symptom improvement. J Gastrointest Surg 2011;15:1513-9. [Crossref] [PubMed]
- Bugiantella W, Rondelli F, Mariani L, et al. Laparoscopic circular stapled longitudinal extramucosal pyloroplasty: an alternative technique for pyloric disruption. Interact Cardiovasc Thorac Surg 2015;21:143-6. [Crossref] [PubMed]
- Wu MH, Wu HH. Simple pyloroplasty using a linear stapler in surgery for esophageal cancer. Surg Today 2013;43:583-5. [Crossref] [PubMed]
- Law S, Cheung MC, Fok M, et al. Pyloroplasty and pyloromyotomy in gastric replacement of the esophagus after esophagectomy: a randomized controlled trial. J Am Coll Surg 1997;184:630-6. [PubMed]
- Lee JW, Sung SW, Park JK, et al. Laparoscopic gastric tube formation with pyloromyotomy for reconstruction in patients with esophageal cancer. Ann Surg Treat Res 2015;89:117-23. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Canon CL, et al. Is botulinum toxin injection of the pylorus during Ivor Lewis [corrected] esophagogastrectomy the optimal drainage strategy? J Thorac Cardiovasc Surg 2009;137:565-72. [Crossref] [PubMed]
- Fuchs HF, Broderick RC, Harnsberger CR, et al. Intraoperative Endoscopic Botox Injection During Total Esophagectomy Prevents the Need for Pyloromyotomy or Dilatation. J Laparoendosc Adv Surg Tech A 2016;26:433-8. [Crossref] [PubMed]
- ASGE Technology Committee. Tools for endoscopic stricture dilation. Gastrointest Endosc 2013;78:391-404. [Crossref] [PubMed]
- Eldaif SM, Lee R, Adams KN, et al. Intrapyloric botulinum injection increases postoperative esophagectomy complications. Ann Thorac Surg 2014;97:1959-64; discussion 1964-5.
Cite this article as: Himmler A, Holliday T, Khaitan PG, Watson TJ, Lazar JF. Pyloric drainage: techniques and controversies. J Vis Surg 2019;5:61.