
Robot-assisted bronchial sleeve left upper lobectomy for locally advanced bronchopulmonary squamous cell carcinoma after neoadjuvant chemotherapy: a case report
Introduction
Sleeve lobectomy is used in the treatment of patients with central bronchopulmonary malignancies. Traditionally, sleeve lobectomy has been performed mostly using an open approach rather than a minimally invasive approach. However, in recent years, robotic sleeve lobectomy has emerged as a safe and feasible surgical technique. Bronchial sleeve lobectomy, a variant of sleeve lobectomy, refers to the procedure without pulmonary vessel anastomosis. Jiao et al. shared their experience of applying this technique; however, its safety and feasibility have yet to be confirmed (1). Here, we introduce the case of a patient undergoing chemotherapy who received robotic bronchial sleeve lobectomy in our department and highlight the advantages of this technique for the preservation of pulmonary vessels. Further, we also describe our experience in handling tight adherence between a tumor and other normal structures. We present the following case in accordance with the CARE reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-19-182/rc).
Case presentation
The patient was a 53-year-old male smoker, who had experienced irritable cough for 6 months. The patient’s vital signs were stable and no abnormalities were noted during physical examination. Chest computed tomography (CT) scan revealed a central mass in the patient’s left lung, and successive bronchoscopy detected a neoplasm situated in his left principal bronchus. Squamous carcinoma was diagnosed by biopsy. Further evaluation showed that the patient had chronic obstructive pulmonary disease, but he had no family history of lung cancer. The disease was staged as T2bN0M0 according to the NCCN guidelines (2020 V1). Because of poor lung function, the patient underwent 4 cycles of neoadjuvant chemotherapy (cisplatin 75 mg/m2 day 1; docetaxel 75 mg/m2 day 1, every 21 days). CT imaging after four cycles of neoadjuvant chemotherapy showed the tumor to have shrunk significantly. The patient’s forced expiratory volume in the first second / forced vital capacity (FEV1/FVC) had improved to 0.72 after preoperative pulmonary rehabilitation, and surgery was recommended. No metastatic malignancies or other contraindications were found. After multidisciplinary discussion, radical sleeve left lobectomy was proposed, and the patient agreed to the operation. After conventional preoperative preparation, the patient received sleeve left lobectomy by robot-assisted approach. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images/video. A copy of the written consent is available for review by the editorial office of this journal.
Surgical technique
Under general anesthesia, the patient was placed in the right lateral decubitus position with double-lumen endotracheal intubation. The da Vinci SI Surgical System was then positioned over the patient’s head.
The first port was placed in the 8th intercostal space in the midaxillary line as the observing hole for the camera. Two operative ports were placed in the 5th intercostal space in the anterior axillary line and the 7th intercostal space in the subscapular line, respectively. Another incision was placed in the 7th intercostal space as the assistant port.
Firstly, we released the left inferior pulmonary ligament and removed the No.9 lymph nodes. The subcarinal space was carefully dissected to expose and remove the No.7 lymph nodes. The camera was then moved towards the superior anterior part of the lung. After the removal of the No. 10 and No. 5 lymph nodes, the left phrenic nerve was fully exposed. The left upper pulmonary vein was controlled, divided, and transected by applying a vessel loop. The pulmonary artery was also divided and controlled using a vessel loop at the proximal site. The oblique fissure was carefully separated to dissect and ligate the arteries and bronchia entering the upper lobe. Due to its proximity to the tumor, A4 + 5 was sutured, and A3 was also carefully dissected and ligated. The left upper lobe now was totally released and removed out of the thorax.
The tumor, along with the adjacent pulmonary artery, was exposed completely. The tumor was tightly adhered to the pulmonary artery. Due to the great risk in detaching the tumor from the vessel, bulldog clamps were applied at the proximal and distal sites of the pulmonary artery. Robotic scissors were used to separate the tumor sharply and to transect the bronchus along with the tumor. Then, the left principal bronchial stump and inferior lobar bronchial stump could be sutured together. The airtightness was confirmed by water and bronchial anastomosis. The tumor margins were verified as negative by fast frozen pathology during the procedure.
Postoperative care
After surgery, the patient was moved to the post anesthesia care unit (PACU) and later transferred to a ward. Enhanced recovery after surgery (ERAS), including early breath training, analgesia, and nutrition support, were used to assist rehabilitation. Postoperative X-ray showed that the lung had re-expanded well, and the chest tube was removed on day 3 after surgery. The patient recovered well, and at 3 months after surgery, he had reported no discomfort.
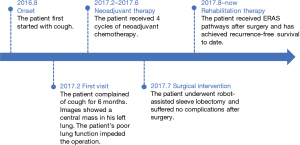
The whole process is showed as a timeline in Figure 1.
Discussion
Sleeve lobectomy is considered to be an alternative to pneumonectomy for patients with central bronchopulmonary malignancies. A propensity score–matched study suggested that sleeve lobectomy provided more benefit than pneumonectomy in early overall and disease-free survival (2). Traditionally, sleeve lobectomy was performed largely by open approach. In recent years, a minimally invasive approach has been widely applied in thoracic surgery, and attempts have been made to perform the operation by video-assisted thoracoscopic surgery (VATS) or robot-assisted thoracoscopic surgery (RATS). In 2016, Diego Gonzalez introduced the technique of uniportal VATS for sleeve procedures (3). However, due to the technical challenges and steep learning curve in using VATS for bronchial anastomosis, uniportal VATS for sleeve resection has not been applied generally (4).
Robot-assisted techniques have also been extensively applied in thoracic surgery. The articulated movements of robotic systems facilitate bronchial anastomosis by minimally invasive approach. Pan et al. reported their initial experience of using a robotic sleeve technique without intraoperative death (5). Jiao et al. introduced their technique of robotic sleeve resection and also noted that no patients died after surgery (1). Gu et al. concluded that robotic surgery is safe and feasible for bronchial sleeve resection and has similar oncological outcomes compared with open procedures (6). Cerfolio performed robot-assisted sleeve resection in 8 patients and reported no 30- or 90-day mortality. All the patients received postoperative chest computerized tomography and bronchoscope examination in 6 months. No significant stricture or recurrent cancer at the anastomosis was found (7). Sleeve resection with RATS has obtained encouraging results for perioperative mortality and short-term oncological outcomes.
Since 2015, our clinical center has employed the da Vinci System for thoracic surgery and accumulated abundant experience of applying robotic techniques. The patient in this case report was a 53-year-old male smoker who had been diagnosed with squamous carcinoma in his left principal bronchus. The surgery had to be postponed due to the patient having poor lung function. After starting chemotherapy and breath training, the patient was reassessed as a candidate for robotic surgery. The patient’s tumor had shrunk and his lung function had improved, so it was concluded that he could tolerate the lobectomy. The biggest problem we encountered was the close proximity of the tumor to the left pulmonary artery. The tumor was adhered tightly to the artery, leaving no space for dissection. Two bulldog clamps were applied (one each at the proximal and distal sites of the pulmonary artery) in case of unexpected bleeding. Carefully and precisely, the tumor was separated from the surface of the pulmonary artery using robotic scissors. Eventually, the tumor, along with the relevant bronchus, was removed, and the pulmonary artery was left intact. We re-evaluated the artery and confirmed that the tumor merely involved adventitia. However, had the arterial media been invaded, the artery would have needed to be resected and then reconstructed. The detailed vision and flexibility of the robotic surgical system made it more convenient and safer to preserve pulmonary vessels. The patient recovered quickly, and experienced no air leakage or bleeding after surgery.
Our experience showed that sleeve lobectomy assisted by a robotic system is safe and feasible for patients with pulmonary arterial adventitia involvement. In our patient, discreet separation could be applied to preserve the artery, because the invasion was limited to the superficial layer. Nevertheless, cases of robotic sleeve resection are still few and studies comparing VATS and RATs are lacking. In future, more studies should be conducted to confirm the effectiveness and safety of robot-assisted lung sleeve resection.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jean-Marc Baste) for the series “Robotic Assisted Thoracic Surgery: Advanced Procedures in Lung and Mediastinum: From Post-induction TTT (immunotherapy) to Sleeve Resection, Complex Segmentectomies and Extended Thymectomy for Myasthenia Gravis” published in Journal of Visualized Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-19-182/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-19-182/coif). The series “Robotic Assisted Thoracic Surgery: Advanced Procedures in Lung and Mediastinum: From Post-induction TTT (immunotherapy) to Sleeve Resection, Complex Segmentectomies and Extended Thymectomy for Myasthenia Gravis” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying image. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jiao W, Zhao Y, Qiu T, et al. Robotic Bronchial Sleeve Lobectomy for Central Lung Tumors: Technique and Outcome. Ann Thorac Surg 2019;108:211-8. [Crossref] [PubMed]
- Pagès PB, Mordant P, Renaud S, et al. Sleeve lobectomy may provide better outcomes than pneumonectomy for non-small cell lung cancer. A decade in a nationwide study. J Thorac Cardiovasc Surg 2017;153:184-95.e3. [Crossref] [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Uniportal video-assisted thoracoscopic bronchoplastic and carinal sleeve procedures. J Thorac Dis 2016;8:S210-22. [PubMed]
- Shanahan B, O'Sullivan KE, Redmond KC. Robotic sleeve lobectomy-recent advances. J Thorac Dis 2019;11:1074-5. [Crossref] [PubMed]
- Pan X, Gu C, Wang R, et al. Initial Experience of Robotic Sleeve Resection for Lung Cancer Patients. Ann Thorac Surg 2016;102:1892-7. [Crossref] [PubMed]
- Gu C, Pan X, Chen Y, et al. Short-term and mid-term survival in bronchial sleeve resection by robotic system versus thoracotomy for centrally located lung cancer. Eur J Cardiothorac Surg 2018;53:648-55. [Crossref] [PubMed]
- Cerfolio RJ. Robotic sleeve lobectomy: technical details and early results. J Thorac Dis 2016;8:S223-6. [PubMed]
(English Language Editor: J. Reynolds)
Cite this article as: Zhang X, Han D, Xiang J, Chen K, Li H. Robot-assisted bronchial sleeve left upper lobectomy for locally advanced bronchopulmonary squamous cell carcinoma after neoadjuvant chemotherapy: a case report. J Vis Surg 2022;8:6.


