Uniportal video-assisted thoracoscopic combined subsegmentectomy: a case report of left S3b + S4b
Introduction
With the advancement of computed tomography (CT) technology, more and more small lung nodules have been encountered clinically. However, it is often difficult to plan a resection for a tiny nodule located deeply between two pulmonary segments, especially when the tumor is located between the left upper-division segments and lingular segments. Whether to perform an extended upper division trisegmentectomy or extended lingulectomy, there are concerns about excessive resection volume or inadequate surgical margin. A combined segmentectomy or combined subsegmentectomy of S3 + S4 could be a feasible solution (1), but they are technically challenging in uniportal video-thoracoscopic surgery (u-VATS). Herein, we report the case of a patient who underwent u-VATS S3b + S4b combined subsegmentectomy and introduce our “open the side door” technique in u-VATS complex subsegmentectomy. We present the following case in accordance with the CARE reporting checklist (available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-29/rc).
Case presentation
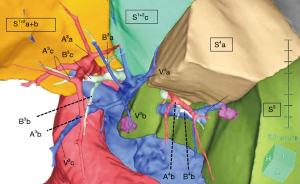
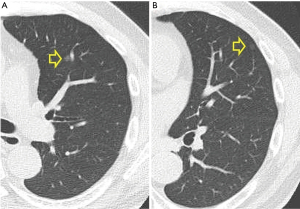
The patient was a 58-year-old man who is a current smoker, and with history of thyroid medullary carcinoma (stage IVA). He had undergone total thyroidectomy and pretracheal and right radical neck lymph node dissection 12 years ago, and was in complete remission status on presentation. Two tiny pure ground-glass opacity nodules (GGNs), 0.6 cm (Figure 1A) and 0.4 cm (Figure 1B) in the left upper lobe were noted on chest CT performed during a health check in 2019. These two nodules were still found in the CT performed 1 year later. Because of the possibility of early primary lung cancer, he decided to undergo surgical resection both for diagnosis and treatment. The 0.6-cm GGN was located between the left S3b and S4b, and the other 0.4-cm GGN was at the surface of the S4b. Therefore, S3b plus S4b combined subsegmentectomy was planned. Three-dimensional CT reconstruction (Synapse Vincent®, Fujifilm Medical Co., Tokyo, Japan) was performed preoperatively to reveal the branching pattern of the associated sub-segmental bronchi and pulmonary vessels (Figure 2).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and the accompany images and video. A copy of the written consent is available for review by the editorial office of this journal.
Surgical technique
General anesthesia was induced, with selective one-lung ventilation using a double-lumen endotracheal tube. The patient was placed on the full right lateral decubitus position, and the operator stood at the ventral site of the patient. The assistant always stood at the other side of the table with a thoracoscope in one hand and Wolf suction in the other hand to assist in exposing the surgical field.
A 3-cm utility port was created at the 4th intercostal space posterior to the anterior axillary line. A 2–4 cm SurgiSleeve wound protector (Medtronic, Minneapolis, MN, USA) was applied at the utility port. A 30° 10-mm thoracoscope was used for vision.
We applied an “open sequential doors” concept in the process of segmentectomy or subsegmentectomy (Video 1). First, we open the “front door” of the target sub-segments; we incise the hilar pleura to expose and identify the upper border (V3c), lower border (V4+5), and intersegmental veins (V3b), which need to be divided. Then, we dissected along the V3c to find the A3b and B3b (the “inner door” of S3b) which was divided by using harmonic scalpel and Echelon Flex Powered Vascular Stapler (Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA), respectively. For subsegmental pulmonary arteries, we usually ligated both the distal and proximal parts of dissected target vessels and then transected them in scissor or harmonic scalpel. For subsegmental bronchi, mostly we transected them by using linear staplers.
At this time, a modified inflation-deflation method (2) was used to identify the boundary of S3b. Then, the “left side door” was opened as we divided the upper border of the S3b by using Echelon Flex 45 articulating endoscopic linear cutter (Ethicon Endo-Surgery Inc., Cincinnati, OH, USA) and harmonic scalpel toward the stumps of B3b and A3b. As a result, we were able to lift the corner of the S3b right ward and the inner door of the S4b, the A4b and B4b was fully exposed. We call this procedure the “open the side door” technique. Subsequently, dissection of the A4b and B4b was much easier.
After division of the A4b and B4b, the modified inflation-deflation method was performed once again to expose the boundary of S4b. The remaining border of the target sub-segments was closed by staplers. Finally, we applied Neoveil absorbable polyglycolic acid (Gunze Limited, Kyoto, Japan) on the raw surface of the remaining upper lobe to minimize the possibility of air-leakage. Operation time was 225 minutes, and the total blood loss was 300 mL.
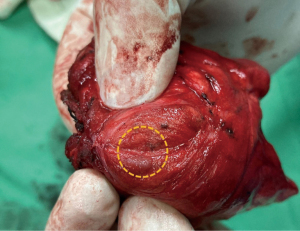
In the target segment specimen, a 0.6 cm grayish nodule was found at the junction of S3b of S4b (Figure 3), and the other tiny nodule was visible at S4b. In the pathology report, the larger nodule was identified as an adenocarcinoma in situ and the smaller one an atypical adenomatoid hyperplasia.
The postoperative course was uneventful. The chest tube was removed on postoperative day 2, and the patient was discharged on postoperative day 3.
Discussion
Herein, we describe our “open the side door” technique and successfully removed two tiny lung nodules located between the left S3b and S4b and beneath the surface of S4b with u-VATS S3b + S4b combined subsegmentectomy.
Our strategy for nodule removal using combined segmentectomy or subsegmentectomy was based on the “open sequential doors” concept. The target segment can be regarded as a room. To enter the room, first, we have to enter the front door. Then, to reach the next or posterior room, we must go through the inner door. Sometimes, the room could be easily entered through the side door. For example, in the upper lobe, the front door is the space between bilateral inter-/intra-segmental veins. For the middle or lower lobe, the front door is the segmental arteries of the target segment, the inner door is the bronchi of the target segment, and the side door is the intra-segmental plane. The procedure for segmentectomy is similar to the process of opening these doors sequentially.
In the common practice of segmentectomy, the front and inner doors are usually opened first (i.e., to open the hilum pleura and ligate the segmental bronchi and arteries). Then, the intersegmental plane is identified by certain methods, and the side doors are opened in last by dividing the lung parenchyma along the intersegmental veins (3). The segmentectomy is complete as the intersegmental planes are all divided.
However, the sub-segmental bronchi and pulmonary vessels can be located deep inside the lung parenchyma and may be difficult to approach through the front and inner doors. Especially, in a u-VATS setting, achieving good exposure of the sub-segmental hilum with only one or two instruments is challenging. Under these circumstances, we recommend this “open the side door” technique. As one of the side doors is opened, the target segment can be moved diagonally, similar to lifting a corner of a bed cover, and the target bronchi and arteries can be well exposed at the center of the operation field, making dissection or ligation of the bronchovascular bundles much easier. This “open the side door” technique is useful especially when performing combined segmentectomy or subsegmentectomy, such as S8a + 9a, 9a + 10a subsegmentectomy in the lower lobe or as in the present case.
Our technique has some limitations. If neither the sub-segmental bronchus nor the pulmonary artery can be dissected and the intersegmental vein is not on the surface of the parenchyma, the side door would have to be opened according to a less accurate, imaginary margin. Fortunately, in most cases, at least part of the target sub-segmental arteries will be transected when proceeding from the front door to the inner door. A reliable margin for the open side door can still be obtained by using indocyanine green and near-infrared thoracoscopy.
In conclusion, S3 and S4 combined subsegmentectomy is a feasible surgical method for tiny nodules located between the upper-division and lingular segments. The “open the side door” technique can help overcome inadequate exposure under u-VATS.
Acknowledgments
The authors thank Enago Academy (www.enago.tw) for providing professional English editing service.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Michel Gonzalez) for the series “VATS Segmentectomy” published in Journal of Visualized Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-29/rc
Peer Review File: Available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-29/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jovs.amegroups.com/article/view/10.21037/jovs-21-29/coif). The series “VATS Segmentectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and the accompany images and video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamashita SI, Yoshida Y, Hamatake D, et al. How to manage tumor located between upper division and lingular segment "S3+S4 segmentectomy and S3b+S4 segmentectomy". J Thorac Dis 2017;9:3277-9. [Crossref] [PubMed]
- Wang J, Xu X, Wen W, et al. Modified method for distinguishing the intersegmental border for lung segmentectomy. Thorac Cancer 2018;9:330-3. [Crossref] [PubMed]
- Wang J, Xu X, Wen W, et al. Technique for tailoring complex demarcation in lung segmentectomy. Thorac Cancer 2018;9:1562-4. [Crossref] [PubMed]
Cite this article as: Chen YY, Lin MC, Tseng YL. Uniportal video-assisted thoracoscopic combined subsegmentectomy: a case report of left S3b + S4b. J Vis Surg 2023;9:16.