Laparoscopic-assisted radical left hemicolectomy
Introduction
Laparoscopic-assisted radical resection of colonic neoplasm was proved to be efficient in the past few years (1). More and more colonic surgeries are done by laparoscopy nowadays while laparoscopic-assisted radical left hemicolectomy (LRLH) is still uncommon. One of the real reasons is that the incidence of descending colonic neoplasm is very low, which was reported about 2.5% of all the colonic neoplasms (2). It can easily cause obstruction so it is not fit for laparoscopic surgery. Another is for its technical difficulties, such as complicated surgical anatomy, both superior mesenteric artery and inferior mesenteric artery lymph nodes dissection, splenic flexure mobilization etc. that needs a long term practice. To perform a LRLH, rich knowledge about anatomy, good surgical techniques and well teamwork are required. In this article and video (Figure 1), we would like to share the surgical techniques with you via a case of descending colonic neoplasm who underwent the LRLH. Moreover, electrocautery was used in most of the operating procedures, which might increase difficulty unless skilled enough.

Methods
Surgical indications
LRLH is suitable for the tumors locate in distal 1/3 of the transverse colon, splenic flexure, descending colon and upper sigmoid colon. Patient with severe cardiopulmonary insufficiency, obstruction or tumor bigger than 6 cm should be excluded.
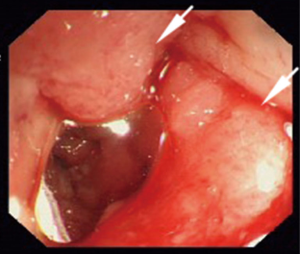
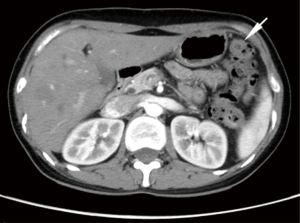
In the present video, the patient is a 34 years old woman who was diagnosed moderately differentiated adenocarcinoma of splenic flexure by coloscope and histological test (Figure 2). The tumor stage was assessed to be cT3N1M0 by CT scan preoperation (Figure 3).
Surgical position
The patient is placed in a supine position after general anesthesia, with both legs split and arms folded. There are three monitors in our operation room that one is positioned above the head and others positioned behind each legs respectively. The operator stands on the right side of the patient while the fist assistance on the other side. Firstly, place the patient at a head-down right side tilt position with the camera assistance at the upper right side of the patient. And then place the patient at a feet-down right side tilt position with the camera assistance between the patient’s legs.
Surgical procedures
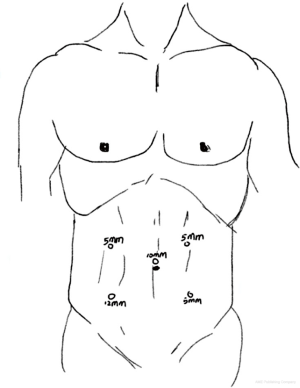
Pneumoperitoneum was built via the Veress needle that should be maintained not to higher than 12 mmHg. In this operation, five trocars, a 12-mm, a 10-mm and three 5-mm trocars, are required. The 10-mm trocar was installed above the umbilicus firstly and a 30-degree laparoscope was inserted. Then other four trocars were installed under direct vision according to the previous position (Figure 4).
The first step of the operation is abdominal exploration to know whether there has any metastasis or invasion to adjacent organs. And then we cut the descending mesocolon from the inferior mesenteric artery, where we can enter the Toldt’s fascia and extend it. If we enter the correct space, we can separate the descending colon from retroperitoneum up to the splenic flexure easily and even without bleeding. At the same time, lymph nodes alone inferior mesenteric artery, vein and their branch should be dissected and the vessels for descending colon should be ligated. In this process, we must careful enough to protect the vessels for sigmoid colon and the rectum. For the tumor locate in the middle of descending colon in this case, we just dissected the lymph nodes alone left branch of middle colic artery and didn’t ligated it. After handle with the vessels and freeing the descending colon, we can start resecting most of the great omentum of the transverse colon. The last step of laparoscopy is to divide the lienocolic ligament and the gastrocolic ligament so that we can mobilize the splenic flexure completely.
We made a left side paramedian about 5 cm in size to take out the tumor and use the anastomosis staplers the make a side-to-side anastomosis (Figure 5). At the end of the operation, we use the vicryl to seam the incision and the trocars holes.
Results
It took about 80 min to finish the whole operation with bleeding of about 30 mL. The pathology outcome after the surgery show it the moderately differentiated adenocarcinoma staging T3N1M0 (IIIB) with 1/12 lymph nodes positive. The patient recovers well postoperation without any significant complication and discharged from hospital on the 5th day.
Discussion
Laparoscopic-assisted radical colectomy has been proved to be safe and effective by many clinical trials (4,5). It has so many advantages like less blood loss, fast recover, shortened hospital stay, etc. that has been accepted gradually and become the standard surgical for colorectal cancer. However, for lack of patients with left colonic carcinoma and less practice, surgeons are unfamiliar with LRLH. What more, carcinoma in descending colon is easy to cause obstruction that make it unfit for laparoscopy surgery (6). In addition, left hemicolectomy requires to dissect the lymph nodes alone the superior mesenteric artery and the inferior mesenteric artery, which make the operation more difficult. The region of lymph nodes dissection should be decided according to the position of the tumor. Tumor locates in the descending colon or sigmoid colon can preserve the middle colic artery with lymph nodes dissection, while in splenic flexure or transverse colon should cut off the middle colic artery.
LRLH is really difficult for many surgeons, especially for young doctors. First attempt should be on the base of rich experiences of laparoscopy surgical techniques. It had better be under guidance of the experienced surgeon. When laparoscopy is hard to go on, we should convert to laparotomy as soon as possible.
Conclusions
LRLH is safe and efficient for the tumor locates in the left hemicolon. Whereas, this operation is rare difficult that should be done in the experienced center.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee. Written informed consent was obtained from the patient. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718-26. [PubMed]
- Larsen IK, Bray F. Trends in colorectal cancer incidence in Norway 1962-2006: an interpretation of the temporal patterns by anatomic subsite. Int J Cancer 2010;126:721-32. [PubMed]
- Li Y, Zheng J, Wu D. Laparoscopic-assisted radical left hemicolectomy. Asvide 2015;2:133. Available online: http://www.asvide.com/articles/709
- Jayne DG, Guillou PJ, Thorpe H, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 2007;25:3061-8. [PubMed]
- Bonjer HJ, Deijen CL, Abis GA, et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 2015;372:1324-32. [PubMed]
- Aslar AK, Ozdemir S, Mahmoudi H, et al. Analysis of 230 cases of emergent surgery for obstructing colon cancer--lessons learned. J Gastrointest Surg 2011;15:110-9. [PubMed]
Cite this article as: Li Y, Zheng J, Wu D. Laparoscopic-assisted radical left hemicolectomy. J Vis Surg 2015;1:15.