Port-access thoracoscopic anatomical right anterior segmentectomy
Introduction
Segmentectomy is increasingly being used for the treatment of small-sized lung cancers. However, segmentectomy using a thoracoscopic approach is controversial as this procedure is complicated and it is difficult to secure adequate working space (1). Using intraoperative three-dimensional contrast-enhanced computed tomography simulation (2), slip knot method for creating the inflation-deflation line (3), and a vessel sealing system to cut the vessels and dissect the parenchyma can make this complicated surgery easier to perform and practically applicable. Herein we report the use of this method for thoracoscopic segment 3 (S3) segmentectomy in a patient with stage IA non-small cell lung cancer (NSCLC).
Case presentation
An 84-year-old woman who was diagnosed with a lung tumor was admitted to our hospital. Chest computed tomography showed a 7-mm-diameter pulmonary nodule in S3 of the right upper lobe; which showed accumulation of fluorodeoxyglucose (FDG) in the positron emission tomography (PET) scan (Figure 1A).
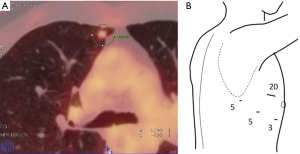
Generally, the procedure is performed under general anesthesia with differential ventilation. Patients are positioned in left lateral decubitus. After single lung ventilation has been initiated, four trocars are inserted. The surgeon stands facing the patient as the video perspective is more natural from the front and the intercostal space is wider than the posterior intercostal space. In our patient, two 5-mm trocars were placed in the 5th intercostal space at the posterior and middle axillary line; a 3-mm trocar was placed in the 5th intercostal space at the anterior axillary line; and a 20-mm soft trocar was placed in the 3rd intercostal space at the anterior axillary line. A 5-mm 30-degree scope was used (Figure 1B).
Using three-dimensional volume rendering, a solid image was constructed from 1-mm data slices of the contrast-enhanced computed tomographic images. The three-dimensional rendered image angiography was focused just within the upper lobe and was magnified, rotated, and set as the surgeon’s view in the operation room (Figures 2,3).
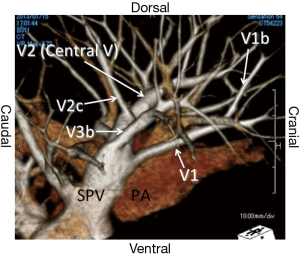
First, the root of the upper pulmonary vein was exposed and the intersegmental vein (V3b) was isolated. The intersegmental vein (V1b) between S1 and S3 was identified and the parenchyma was dissected along the intersubsegmental vein. The key to this procedure is to release the vascular sheath using forceps and dissect the parenchyma using a sealing device. The anterior pulmonary artery (PA) (A3) was identified and dissected beside the V1b. After opening the fissure, the posterior vein (V2) was exposed and the intersegmental vein (V3b) was encircled. The anterior PA (A3) was ligated using 2-0 silk. The key to this procedure is to divide this artery proximal to the V1b that enables the adequate dissection of the bronchus. The V3b was clipped and divided using a sealing device. The parenchyma was again dissected along the intersegmental vein (V1b) and the subsegmental arterial branches (A3a, A3b) of the A3 were divided using the vessel-sealing device. The lymph nodes of the hilum (#12u) were dissected and the frozen section revealed no signs of metastasis.
The branch of the posterior vein (V2) was exposed and the intersegmental vein between S2 and S3 (V2c) was identified. The parenchyma was dissected along the proximal V2c. Such dissection and isolation of the veins as well as the arteries facilitates the best anatomical exposure of the bronchus.
The anterior bronchus (B3) was then encircled using a monofilament polypropylene thread, and a modified Roeder knot was created extracorporeally. Both lungs were inflated and the slip knot was pulled to ligate the bronchus with full expansion of the lung. The right lung was again collapsed and the B3 was stapled and divided using an endoscopic stapler (3). Thereafter, the S3 remained inflated while the other segments collapsed. The intersegmental plane of the parenchyma was divided by electrocautery or by using sealing device as described previously. After parenchymal dissection in the hilum, even the main branch of V2 (so called central vein) besides V1b or V2c became apparent. Finally, the peripheral lung parenchyma was divided using staplers and the S3 was removed using a retrieval bag. Fibrin glue was sprayed to the intersegmental plane (Figure 4).
The operative time was 145 min, and blood loss was 80 mL. The chest drainage tube was removed on postoperative day 1.
Discussion
The number of reports of anatomical segmentectomy or subsegmentectomy is increasing owing to the growing number of patients diagnosed with peripheral smaller NSCLCs, such as ground glass opacity nodules (1,6). However, reports of these procedures performed using a thoracoscopic approach are limited (1,2,7). Majority of the resected segments are related to the easier and larger segments such as lingular segment, superior segments of bilateral lower lobe, left upper division, or bilateral basilar segments.
We introduced three-dimensional computed tomography simulation to comprehend the precise anatomy of the complicated vessels and the bronchi. This enabled us to resect even the most difficult segments such as the posterior basal segment of the lower lobe by using electrical devices and staplers (2). Moreover, the slip knot method made it possible to resect the smaller subsegments with sufficient surgical margin (3). S3 is classified as a fairly difficult to resection via the total thoracoscopic approach. A considerable number of knacks or tips exist that may help perform anatomical thoracoscopic segmentectomies precisely.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee. Written informed consent was obtained from the patient for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Oizumi H, Kanauchi N, Kato H, et al. Total thoracoscopic pulmonary segmentectomy. Eur J Cardiothorac Surg 2009;36:374-7; discussion 377. [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Set up of three-dimensional computed tomography angiography image. Asvide 2015;2:134. Available online: http://www.asvide.com/articles/710
- Oizumi H, Kato H, Endoh M, et al. Port-access thoracoscopic anatomical segmentectomy procedure (S3). Asvide 2015;2:135. Available online: http://www.asvide.com/articles/711
- Kato H, Oizumi H, Inoue T, et al. Port-access thoracoscopic anatomical lung subsegmentectomy. Interact Cardiovasc Thorac Surg 2013;16:824-9. [PubMed]
- Gossot D, Ramos R, Brian E, et al. A totally thoracoscopic approach for pulmonary anatomic segmentectomies. Interact Cardiovasc Thorac Surg 2011;12:529-32. [PubMed]
Cite this article as: Oizumi H, Kato H, Endoh M, Suzuki J, Watarai H, Suzuki K, Sadahiro M. Port-access thoracoscopic anatomical right anterior segmentectomy. J Vis Surg 2015;1:16.


