Da Vinci Robotic System in the surgery for mediastinal bronchogenic cyst: a report on five patients
Introduction
Bronchogenic cysts are congenital lesions originating from the primitive ventral foregut. Nearly two-thirds are within the mediastinum, and one-third are intraparenchymal. They account for 40-50% of all congenital mediastinal cysts. Once a bronchogenic cyst has been diagnosed radiologically, it should be excised to establish the histopathological diagnosis, in order to prevent complications such as infection, hemoptysis, rupture, or fear of malignancy (1).
The traditional surgical approach is an open approach, either a posterolateral thoracotomy or median sternotomy, depending on the localization of the cyst in the mediastinum. Total enucleation is the procedure of choice, and complete excision is possible in nearly all cases, whether the cyst is complicated or not (2). In the last decade, several reports on thoracoscopic resection of mediastinal bronchogenic cysts have been published encouraging minimally invasive approach (3-5).
The use of robotic system in the surgery of mediastinal pathologies has been increasing worldwide. Many studies have already demonstrated the safety of robotic thymectomy as well as removal of other mediastinal masses (6-10). Mediastinal bronchogenic cyst resection have already been performed by using robotic system. To our knowledge, Yoshino et al. (11) reported the first resection of a mediastinal bronchogenic cyst using robotic system in 2002. Since then, only 12 cases have been added to the English literature (10, 12-15).
The da Vinci Robotic System (Intuitive Surgical, Inc., Mountain View, California, USA) has been adopted in our instutition on October 2011. Our previous reports on robotic pulmonary resections have been published elsewhere (16-18). Here in this paper we aimed to present the results of the patients with mediastinal bronchogenic cysts that underwent robotic surgery using da Vinci Robotic System.
Patients and methods
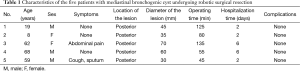
Since the set-up of the program, 200 patients underwent robotic thoracic surgery between October 2011 and September 2015, of which 17 patients (8.5%) had mediastinal pathologies. Five of them (29%) had pathologically proven mediastinal bronchogenic cyst, and they were enrolled into the study. The decision to offer robotic approach was made according to the healthcare insurance systems, and the patients’ willingness. Their medical files were retrospectively investigated, and the symptoms at diagnosis, radiologic findings, and locations of the lesions were evaluated retrospectively.
All patients had chest X-rays and computed tomography of the chest. Additional studies included standard hematology and chemistry panel studies, cardiac evaluation, arterial blood gases, and pulmonary function testing. No perioperative invasive diagnostic methods have been used, since the lesions were cystic in nature.
A single thoracic surgeon (AT) performed cystectomy to all patients. A dedicated team of surgeons (including table surgeon and first surgical assistant), nurses, and anesthetists involved during the procedures. The operating time, including the docking and console times, post-operative hospitalization, and peri- and post-operative complications were recorded. The definitions of docking and console times have been previously given (18).
The patient was positioned on lateral decubitus position after single-lung ventilation was established and confirmed with the fiberoptic bronchoscope. The table was tilted either anteriorly or posteriorly depending on the type of the operation to be performed before the robotic arms were docked. Three ports have been used, and were placed as previously described (14,18).
This video shows a case of a mediastinal bronchogenic cyst excision using da Vinci Robotic System (Figure 1). After the visualization of the lesion, the mediastinal pleura was opened, and the tissues alongside the lesion capsule were dissected using the Electrocautery (EndoWrist, Intuitive Surgical). The cysts were removed after the aspiration of the cystic fluid without any bleeding or harm to the adjacent tissues, and were extracted through the service port covered with ALEXIS® soft tissue skin retractor (Applied Medical, Rancho Santa Margarita, CA) using a plastic endobag.

One chest tube was used for each patient and was removed during the hospital stay as soon as the drainage was less than 200 mL/day or no air leak was present. One patient required decortication due to infection of the cyst and pleura. He was on hemodialysis for the past 6 years due to chronic renal failure. The study received institutional review board approval, with individual patient consent being waived.
Results
There were five patients (male/female: 3/2) in this study, with a mean age of 43±28 years (Table 1). All the lesions were located at the posterior mediastinum. The cysts averaged 48 mm in their largest diameter (range 30-70 mm). Three patients were asymptomatic. The lesions had been detected in the remaining two patients during the investigation of cough and abdominal pain. Complete cyst excision was performed in all patients. There were no operative deaths and no intra-operative complications. There was no need for conversion to thoracotomy or video-assisted thoracic surgery (VATS). The mean docking time was 20±12 min, the mean console time was 63±32 min, and the mean operating time was 88±41 min. Postoperative course was uneventful in all cases. The mean chest tube duration time was 2.4±1.7 days, and the mean length of stay was 3.6±2.2 days. Histologic examination was performed in all cases, and confirmed the diagnosis of bronchogenic cyst with the typical feature of a ciliated pseudostratified columnar epithelial lining with smooth muscle present in the cyst wall and mucous glands present in the lamina propria. During follow-up, which ranged from 6 months to 3 years, no patients presented with late-onset or recurrent complications.
Full table
Discussion
Bronchogenic cysts are relatively uncommon, and usually asymptomatic if they are of the intrapulmonary type. If they are of the mediastinal type, they can cause compression to the neighbouring organs, and symptoms such as wheezing, coughing, dyspnea, atelectasis and dysphagia may develop. Besides, severe symptoms including bloody expectoration, bloody sputum, hemoptysis, fever and pyothorax may occur in some patients when the condition is complicated by an infection (1). One of our patients developed empyema, he was on hemodialysis for chronic renal failure. However, most bronchogenic cysts are found incidentally when imaging is performed for other reasons (1,5). Three patients in our study (60%) were asymptomatic.
Regarding therapeutic approach, a bronchogenic cyst should be excised to establish the definitive diagnosis, as well as to prevent possible complications and fear of malignancy. Routine surgical procedure has traditionally been complete cyst removal by open approaches (1,2,9). Accumulated experience with minimally invasive surgery has enabled a less traumatic approach in the treatment of mediastinal lesions. Several reports on thoracoscopic resection of mediastinal bronchogenic cysts have been published encouraging minimally invasive approach (3-5). The main advantage of thoracoscopy is less trauma and discomfort for the patient. Since the lack of intercostal muscle incision and the lower risk of rib fracture reduce the postoperative pain compared to thoracotomy, it is claimed that thoracoscopy reduces the chest tube duration and length of hospital stay (3).
Although thoracoscopy is less invasive than an open approach, it carries the problem of difficulty of manipulation in narrow spaces, such as the upper and lower thoracic spaces (near the apex or diaphragm) and immediately adjacent to the vertebrae and the aorta. Nowadays, several reports on the feasibility and safety of the robotic system in the surgery of mediastinal lesions located at anterior or middle mediastinum (12,20), and posterior, upper and inferior mediastinum (10,13) have been reported with encouraging results.
Bronchogenic cysts in the mediastinum are mostly adherent to adjacent vital structures such as trachea, aorta and main bronchii, and thus, this makes a complete resection by conventional thoracoscopy difficult. In case of dense adhesions, surgical appraoch via thoracotomy should be always kept in mind. But the three-dimensional visualization, greater instrument manoeuvrability and more accurate dissection of robotic systems may overcome this difficulty, and avoid the incomplete resection of mediastinal bronchogenic cysts. The articulating instruments may be particularly helpful for dissecting around a mediastinal mass within the vital tissues in the thoracic cavity (9,10,14).
To our knowledge, Yoshino et al. (11) reported the first resection of a mediastinal bronchogenic cyst using robotic system in January 2001, and published their report in 2002. They resected a 2.0 cm bronchogenic cyst located at the left posterior mediastinum. Since that date, only 11 cases have been added to the English literature (10,12,13,15). Although robotic resection of mediastinal bronchogenic cysts in teenagers have been reported in some of the abovementioned studies, our previous report on a 8-year-old female patient is the first report concerning of patients in the first decade of life (14). In that report, we recommended minimally invasive resection of mediastinal bronchogenic cysts to avoid the risk of scoliosis development in childhood following thoracotomy. This study consisted of the patient presented before and four additional patients with posterior mediastinal bronchogenic cyst, all of whom underwent resection by robotic surgery using the da Vinci System. There was no mortality or morbidity in our study, similar to the previous reports.
In conclusion, we believe that mediastinal bronchogenic cysts should be treated surgically. The robotic system has been confirmed to be a safe, accurate and minimally invasive approach with promising clinical value. Small trauma, mild pain, quick recovery and good cosmesis are among its features. Also, it can thoroughly remove the lesions in the mediastinum with high safety and success rate.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study received institutional review board approval, with individual patient consent being waived.
References
- St-Georges R, Deslauriers J, Duranceau A, et al. Clinical spectrum of bronchogenic cysts of the mediastinum and lung in the adult. Ann Thorac Surg 1991;52:6-13. [PubMed]
- Sirivella S, Ford WB, Zikria EA, et al. Foregut cysts of the mediastinum. Results in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg 1985;90:776-82. [PubMed]
- Tölg C, Abelin K, Laudenbach V, et al. Open vs thorascopic surgical management of bronchogenic cysts. Surg Endosc 2005;19:77-80. [PubMed]
- Weber T, Roth TC, Beshay M, et al. Video-assisted thoracoscopic surgery of mediastinal bronchogenic cysts in adults: a single-center experience. Ann Thorac Surg 2004;78:987-91. [PubMed]
- De Giacomo T, Diso D, Anile M, et al. Thoracoscopic resection of mediastinal bronchogenic cysts in adults. Eur J Cardiothorac Surg 2009;36:357-9. [PubMed]
- Bodner J, Wykypiel H, Greiner A, et al. Early experience with robot-assisted surgery for mediastinal masses. Ann Thorac Surg 2004;78:259-65; discussion 265-6. [PubMed]
- Rea F, Marulli G, Bortolotti L, et al. Experience with the “da Vinci” robotic system for thymectomy in patients with myasthenia gravis: report of 33 cases. Ann Thorac Surg 2006;81:455-9. [PubMed]
- Weissenbacher A, Bodner J. Robotic surgery of the mediastinum. Thorac Surg Clin 2010;20:331-9. [PubMed]
- Augustin F, Schmid T, Bodner J. The robotic approach for mediastinal lesions. Int J Med Robot 2006;2:262-70. [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Operative techniques in robotic thoracic surgery for inferior or posterior mediastinal pathology. J Thorac Cardiovasc Surg 2012;143:1138-43. [PubMed]
- Yoshino I, Hashizume M, Shimada M, et al. Video-assisted thoracoscopic extirpation of a posterior mediastinal mass using the da Vinci computer enhanced surgical system. Ann Thorac Surg 2002;74:1235-7. [PubMed]
- Kajiwara N, Kakihana M, Kawate N, et al. Appropriate set-up of the da Vinci Surgical System in relation to the location of anterior and middle mediastinal tumors. Interact Cardiovasc Thorac Surg 2011;12:112-6. [PubMed]
- Kajiwara N, Kakihana M, Usuda J, et al. Extended indications for robotic surgery for posterior mediastinal tumors. Asian Cardiovasc Thorac Ann 2012;20:308-13. [PubMed]
- Toker A, Ayalp K, Grusina-Ujumaza J, et al. Resection of a bronchogenic cyst in the first decade of life with robotic surgery. Interact Cardiovasc Thorac Surg 2014;19:321-3. [PubMed]
- Xu S, Liu B, Wang X, et al. Robotic thoracic surgery of the anterior superior mediastinal bronchogenic cyst. Ann Transl Med 2015;3:57. [PubMed]
- Toker A, Ayalp K, Uyumaz E, et al. Robotic lung segmentectomy for malignant and benign lesions. J Thorac Dis 2014;6:937-42. [PubMed]
- Demir A, Ayalp K, Ozkan B, et al. Robotic and video-assisted thoracic surgery lung segmentectomy for malignant and benign lesions. Interact Cardiovasc Thorac Surg 2015;20:304-9. [PubMed]
- Toker A, Özyurtkan MO, Kaba E, et al. Robotic anatomic lung resections: the initial experience and description of learning in 102 cases. Surg Endosc 2015. [Epub ahead of print]. [PubMed]
- Toker A, Özyurtkan MO, Kaba E, et al. Perioperative video of the patient no. 5. Asvide 2015;2:153. Available online: http://www.asvide.com/articles/730
- Kajiwara N, Taira M, Yoshida K, et al. Early experience using the da Vinci Surgical System for the treatment of mediastinal tumors. Gen Thorac Cardiovasc Surg 2011;59:693-8. [PubMed]
Cite this article as: Toker A, Özyurtkan MO, Kaba E, Nova G. Da Vinci Robotic System in the surgery for mediastinal bronchogenic cyst: a report on five patients. J Vis Surg 2015;1:23.


