Multimodality dissection in dealing with benign hilar or interlobar lymphadenopathy during video-assisted thoracoscopic surgery lobectomy
Introduction
Since introduced in early 1990s, anatomic lung resection by video-assisted thoracoscopic surgery (VATS) has become more and more popular for both malignant and benign pulmonary diseases (1). Although major advances have been achieved, it’s still difficult and risky for surgeons to troubleshooting complicated hilum with severe hilar or interlobar lymphadenopathy. It’s a technique demanding work to dissect the target bronchus or pulmonary artery from the surrounding lymphadenopathy during VATS lobectomy. Worrying about injury to blood vessels and massive bleeding most thoracic surgeons opt to convert thoracoscopic approach to thoracotomy. In this paper, we’d like to present a case of VATS lobectomy with severe lymphadenopathy.
Case presentation
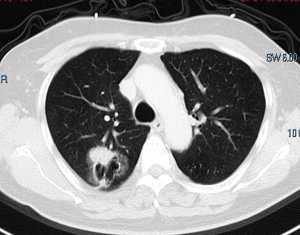
A 77-year-old male presented with a cystic mass in the right upper lobe for about 11 years (Figure 1). The lesion began to enlarge 2 months before admission while it was stable during the past 11 years. Suspected to be with lung cancer, he was advised to receive right upper lobectomy. Preoperative assessments were negative. VATS right upper lobectomy was scheduled.
Detailed procedures of the lobectomy were shown in this video (Figure 2). Complicated hilar lymphadenopathy was identified. The peri-arterial/peri-bronchial lymph nodes fused together and they were separated from the target vessels and bronchus using multimodality, such as electrocoagulation hook, harmonic scalpel, and sharp dissecting using scissors. After the lobectomy, intraoperative frozen section pathological examination confirmed an adenocarcinoma and mediastinal lymphadenectomy was performed. The operation finally went through smoothly and the patient recovered well as expected.
Discussion
Lymphadenopathy is a very common and sometimes tough situation to manage during VATS lobectomy. For cases with severe hilar or interlobar lymphadenopathy, it’s always difficult to dissect the target bronchus or pulmonary artery. Methods for troubleshooting lymphadenopathy are varied according to different location and severity. This video just shows one kind of situation that could be handled via routine means. There should be more methods for choice, such as firing the target structures together, controlling the main pulmonary artery in advance, and so on.
Conclusions
In conclusion, for cases with severe benign hilar or interlobar lymphadenopathy, skilled operation and multimodality are required. If the surgeon is not so confident to troubleshoot the lymphadenopathy under thoracoscopy, conversion to thoracotomy should never be deserted.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee. Written informed consent was obtained from the patient for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Yan TD, Cao C, D'Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2014;45:633-9. [PubMed]
- Liu C, Ma L, Mei H, et al. Three portal VATS lobectomy involved with complicated hilar lymphadenopathy. Asvide 2016;3:059. Available online: http://www.asvide.com/articles/810
Cite this article as: Liu C, Ma L, Mei H, Xu C, Che G. Multimodality dissection in dealing with benign hilar or interlobar lymphadenopathy during video-assisted thoracoscopic surgery lobectomy. J Vis Surg 2016;2:25.