How to deal with benign hilar or interlobar lymphadenopathy during video-assisted thoracoscopic surgery lobectomy—firing the bronchus and pulmonary artery together
Introduction
Since introduced in early 1990s, anatomic lung resection for lung cancer by video-assisted thoracoscopic surgery (VATS) has become a standard surgical modality for early-stage lung cancer and has been gradually applied to more advanced diseases (1). Although major advances have been achieved in both equipment and technique in VATS, the adoption of VATS has been variable for lung surgery due to perceived technical challenges and the concern for intraoperative complications and conversion to thoracotomy (2). Intraoperative complications should not be ignored. In particular the need for intraoperative conversion to open thoracotomy might lead to potential adverse consequences (3). The conversion rates have been reported to range from 2% to as high as 23% in different centers (2). Sporadic literatures focused on the detailed accounts of intraoperative complications and causes of conversion (2-5). Overall, theses causes can generally be classified into the following categories: technical problems (e.g., technical challenges, equipment malfunction), anatomical problems (e.g., absent or fused fissure, diffuse or complete pleural adhesions, large tumor size, tumor location/invasion, lymph node issues), and some intraoperative complications (e.g., massive bleeding from vascular injury, bronchus injury, and other serious accident injuries). Among these, lymph node issues are very common and sometimes tough to manage. For cases with severe hilar or interlobar lymphadenopathy, it’s difficult to dissect the target bronchus or pulmonary artery separately during VATS lobectomy. In this video, we’d like to introduce the method of “firing the bronchus and pulmonary artery together” to troubleshoot situations with severe inflammatory or calcified peri-arterial/peri-bronchial lymphadenopathy.
Case presentation
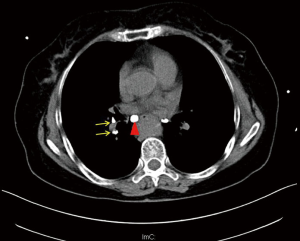
This video shows a complex case of right lower lobectomy using the technique of “firing the bronchus and pulmonary artery together” (Figure 1). This operation was performed via triportal VATS (observation port: 1.0 cm, in the 7th intercostal space at the midaxillary line; two utility incisions: a 3-cm main utility incision at the anterior axillary line in the 4th intercostal space and a 2-cm assistant utility incision in the 7th intercostal space between the posterior axillary line and subscapular line. After thoracic exploration, the inferior pulmonary vein was first dissected. As manifested by preoperative computed tomography scans (Figure 2), there was a big calcified node adhering close to the intermediate bronchus. It was dissected via sharp dissection using scissors. When we proceeded to the inferior bronchus, more calcified lymph nodes were identified (Figure 2). Only through sharp dissecting using scissors could we dissect the inferior and posterior inflammatory/calcified nodes from the bronchus laboriously. There were also interlobar inflammatory nodes. After we completed the fissures we found that there was no clearance between the inferior pulmonary artery and bronchus, which were frozen together by calcified nodes. Then we decided to divide the inferior pulmonary and bronchus together using endoscopic stapler. The operation finally went through smoothly and the postoperative course was uneventful.
Discussion
Most thoracic surgeons opt to convert thoracoscopic approach to thoracotomy when there is a high risk of massive bleeding because of severe adhesions between the pulmonary artery and lymphadenopathy surrounding it. Some experts developed the technique of “controlling the main pulmonary artery in advance”, with which the surgeon can dissect the artery from surrounding tissues without worrying about massive vascular bleeding (7-9). However, in some cases the peri-arterial/peri-bronchial lymph nodes fuse together and it’s hard to separate the target artery or bronchus even with sharp dissecting using scissors. Therefore, firing the bronchus and pulmonary artery is a good method of choice. However, during this process, several technical skills should be noted: (I) carefully dissect the target artery and bronchus as much as possible to make sure enough distance and space for placement of the endoscopic stapler; (II) clamp the target at the thinnest part using the endoscopic stapler to make sure a safe firing; (III) use a thickest stapler; (IV) complementary cross mattress suture was important to shorten the stumps and reinforce the stumps to avoid postoperative bronchopleural fistula or bleeding.
Conclusions
In conclusion, for cases with severe benign hilar or interlobar lymphadenopathy, the method of “firing the bronchus and pulmonary artery together” is an optimal option. However, if the surgeon is not so confident to deal with that kind of tough situations under thoracoscopy, conversion to thoracotomy should never be forgotten.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee. Written informed consent was obtained from the patient for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Yan TD, Cao C, D'Amico TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg 2014;45:633-9. [PubMed]
- Hanna JM, Berry MF, D'Amico TA. Contraindications of video-assisted thoracoscopic surgical lobectomy and determinants of conversion to open. J Thorac Dis 2013;5 Suppl 3:S182-9. [PubMed]
- Puri V, Patel A, Majumder K, et al. Intraoperative conversion from video-assisted thoracoscopic surgery lobectomy to open thoracotomy: a study of causes and implications. J Thorac Cardiovasc Surg 2015;149:55-61, 62.e1.
- Byun CS, Lee S, Kim DJ, et al. Analysis of Unexpected Conversion to Thoracotomy During Thoracoscopic Lobectomy in Lung Cancer. Ann Thorac Surg 2015;100:968-73. [PubMed]
- Samson P, Guitron J, Reed MF, et al. Predictors of conversion to thoracotomy for video-assisted thoracoscopic lobectomy: a retrospective analysis and the influence of computed tomography-based calcification assessment. J Thorac Cardiovasc Surg 2013;145:1512-8. [PubMed]
- Liu C, Ma L, Pu Q, et al. Three portal VATS lobectomy complicated with sever hilar and interlobar inflammatory and calcified lymph nodes. Asvide 2016;3:060. Available online: http://www.asvide.com/articles/812
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [PubMed]
- Kamiyoshihara M, Nagashima T, Ibe T, et al. A tip for controlling the main pulmonary artery during video-assisted thoracic major pulmonary resection: the outside-field vascular clamping technique. Interact Cardiovasc Thorac Surg 2010;11:693-5. [PubMed]
- Watanabe A, Koyanagi T, Nakashima S, et al. How to clamp the main pulmonary artery during video-assisted thoracoscopic surgery lobectomy. Eur J Cardiothorac Surg 2007;31:129-31. [PubMed]
Cite this article as: Liu C, Ma L, Pu Q, Liao H, Liu L. How to deal with benign hilar or interlobar lymphadenopathy during video-assisted thoracoscopic surgery lobectomy—firing the bronchus and pulmonary artery together. J Vis Surg 2016;2:26.


