Single-incision thoracoscopic right pneumonectomy with primary division of the pulmonary artery
Introduction
When the central hilar structures or all lobes on one side are invaded by the tumor and sleeve-resection is not technically feasible, pneumonectomy is the only option for a curative surgical approach. While open surgery was the gold-standard approach for pneumonectomy until recently, video-assisted thoracoscopic surgery (VATS) techniques are gaining popularity also for major lung resections recently (1). So far only a few case reports including one larger series with 10 patients on single-incision thoracoscopic pneumonectomy have been reported in the international literature (2). Herein we describe and illustrate our single incision thoracoscopic approach without rib-spreading for right pneumonectomy. Unlike other authors (2) we prefer to divide the pulmonary artery (PA) as one of the first steps of the procedure in order to obtain a clear field of vision on one hand and optimal control of bleeding and total blood loss on the other hand.
Surgical technique
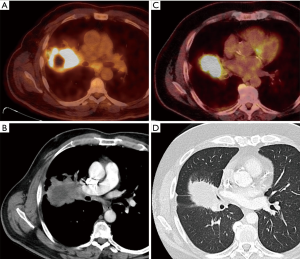
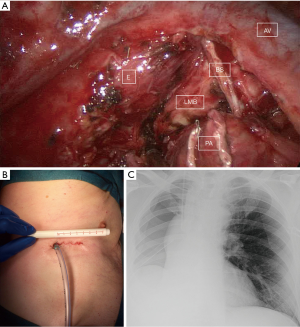
For the procedure the patient is intubated with a disposable left-sided double-lumen tube and placed in a lateral decubitus position. A camera-port is placed in the 6th intercostal space in the anterior axillary line and a 5 mm, 30° angled, rigid thoracoscope is introduced. After thoracoscopic assessment of tumor resectability as well as the need for pneumonectomy, an intercostal nerve block of the intercostal spaces 5 to 7 is performed using 30 mL of 0.75% ropivacaine. Then the incision is enlarged to about 4−6 cm length and an elastic wound-protector (SurgisleeveTM, Size M, by Covidien) is installed. With the goal of optimal bleeding control and avoidance of venous congestion of the lung, we first concentrate on the PA. In case of central tumor invasion of the PA (Figure 1A,B), the vessel needs to be centrally divided in one single step. As shown in the video, caudal retraction of the upper lobe vein eases access to the main PA. Another possibility to approach the PA is shown in example 2 (Figure 1C,D), where first the truncus anterior (Boyden trunk) was stapled and then the remaining right PA was divided (Figure 2). After division of the veins, the right main stem bronchus is dissected and stapled at its origin at carinal level under bronchoscopic control. The specimen is removed in an endobag and after systematic mediastinal lymph node dissection the bronchial stump (BS) is covered with an in situ azygos vein (AV) flap (Figure 3). A single 24 French chest tube is placed and the incision is closed (Figure 4).


Comments
Recently thoracoscopic lobectomy has become the new standard of care for early stage lung cancer. Furthermore the feasibility and usefulness of a uniportal approach has been reported even for advanced stages of non-small cell lung cancer (5). In most thoracoscopic resections the venous drainage of the lung is divided first, since it is the first structure that is presenting on the anterior side of the hilum and after its division subsequent access to the remaining structures behind the vein is easier. Whether the artery or the vein should be divided first is still under debate from an oncological point of view.
We have introduced the single-incision technique for major lung resections in November 2014 and have performed a total of five right pneumonectomies using this “artery first” approach to date. Informed consent was obtained from all patients before study inclusion. Mean patient age was 68 years (range, 58–76 years) with a mean surgery time of 154 minutes (range, 130–180 minutes) and a mean blood loss of 230 mL (range, 100–400 mL). Mean tumor size was 6.4 cm (range, 5–8 cm), and the length of the incision used for surgery was between 4.5 and 7 cm. All patients were postoperatively monitored for 12 hours on our intermediate care unit and showed an uneventful course without the need for neither vasopressor drugs nor patient controlled analgesia. With a stable hemoglobin level on the first postoperative day and no signs of bleeding, the chest tube was removed the same day and patients were discharged home on postoperative day 4–6 (mean: 5.2) with no complications. Final histopathologic stage was pT2b pN1 in three and pT3 pN1 in the other two patients. Coverage of the BS is still an issue under debate without any clear answer yet (6), but since ‘right pneumonectomy’ is already a risk factor for bronchopleural fistula, the BS was covered with an AV flap in all of our patients.
In our opinion early division of the PA has some major advantages. First of all, bleeding from the lung is less severe if the lung is injured during maneuvers of exposure or handling. Second, with division of the artery before the vein, there is no venous congestion and less excessive bleeding from an accidentally injured lung parenchyma, which both may hamper a video-assisted approach. Last but not least, there is a not negligible amount of circulating blood, which is captured in the lung specimen and removed from the circulation during surgery, which might be reduced by primary ligation of the arterial inflow before ligating the outflow from the lung. From an oncological point of view, thoracoscopic pneumonectomy is comparable to open surgery, with equivalent survival rates (7). Furthermore the uniportal approach seems to result in less pain and a faster recovery compared to VATS with multiple access ports (8) and also allows easy coverage of the BS if deemed necessary. In our experience division of the main PA as a first step might be another important detail, which may not only ease the course of the whole procedure, but also improve patient recovery after surgery due to a minimization of total blood loss.
In our opinion, single-port thoracoscopic pneumonectomy is a feasible procedure in selected cases and experienced centers and patients benefit from less pain and thus faster recovery compared to open surgery. Furthermore early division of the PA eases the further course of the operation and seems to reduce total blood loss, which might again contribute to a better recovery of these patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Battoo A, Jahan A, Yang Z, et al. Thoracoscopic pneumonectomy: an 11-year experience. Chest 2014;146:1300-9. [Crossref]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Uniportal video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2013;5 Suppl 3:S246-52. [PubMed]
- Kocher GJ, Hoksch B, Lutz J, et al. In this video the dissection and division of the right pulmonary artery in one single step and in two steps is demonstrated (example 1 and 2). Asvide 2016;3:076. Available online: http://www.asvide.com/articles/829
- Kocher GJ, Hoksch B, Lutz J, et al. Shows the division of the veins as well as bronchial division, mediastinal lymphadenectomy and covering of the bronchial stump with an in situ azygos vein flap. Asvide 2016;3:077. Available online: http://www.asvide.com/articles/830
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Di Maio M, Perrone F, Deschamps C, et al. A meta-analysis of the impact of bronchial stump coverage on the risk of bronchopleural fistula after pneumonectomy. Eur J Cardiothorac Surg 2015;48:196-200. [Crossref] [PubMed]
- Nwogu CE, Yendamuri S, Demmy TL. Does thoracoscopic pneumonectomy for lung cancer affect survival? Ann Thorac Surg 2010;89:S2102-6. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
Cite this article as: Kocher GJ, Hoksch B, Lutz J, Schmid RA. Single-incision thoracoscopic right pneumonectomy with primary division of the pulmonary artery. J Vis Surg 2016;2:41.


