Why should we prefer the single port access thoracic surgery?
Introduction
One of the greatest advances in thoracic surgery in our generation has been the advent of video assisted thoracic surgery (VATS). Compared to open thoracotomy, VATS has been demonstrated to significantly reduce pain, hasten recovery, minimize complications, and improve post-operative quality of life. The more recent advance in VATS is the increasing use of uniportal surgery. Single-port access VATS is an attractive surgical approach, because of its potential benefits and advantages. Uniportal VATS did not only cosmetically satisfy patients, but also led to improvement in parameters related with short-term operative outcomes. Therefore, single port access VATS is actually simply the next step in the evolution of minimally invasive thoracic surgery itself (1). The development of single port VATS has come a long way, from the beginning, when it was employed for performing simple procedures (such as sympathectomy and pleurodesis), to the rapid progression in the last years of complex major lung resections (2).
Basic techniques of single port access VATS
Preoperatively, a chest computed tomography scan should be interpreted by the operating surgeon in order to identify not only the location of the target lesion, but also the anatomical tips and pitfalls. In our experience, all surgical procedures were performed under general anaesthesia with double-lumen endotracheal tube placement for one-lung ventilation at the healthy side. The patients were placed in a lateral decubitus position on the unaffected side. The general rules of the single access VATS have been clearly described by Gaetano Rocco (one of the fathers of this approach). The scapular angle line (longitude) is considered the separation between anteriorly and posteriorly located incisions, to address posterior and anterior lesions, respectively. The intercostal space for the incision is selected at a level (latitude) based on ensuring sufficient space between the single port and target lesion to avoid mutual interference of the thoracoscope-operative instruments ensemble. Thereafter, the surgical incision (3.5−4.5 cm in length) was created in the fourth or fifth intercostal space at the anterior axillary line at the diseased side. Access to the intercostal plane is granted by a blunt technique similar to the chest drain placement. The incision protector was applied in the port, and no distraction device was employed to separate the ribs. The operator stood at the abdominal side of the patient, and operated using the endoscopic instruments only. A 30-degree 10-mm videothoracoscope was introduced in the superior side of incision and was used for visualization while articulating instruments help bring the operative fulcrum inside the chest (3). Through the same incision, several instruments can be introduced parallel to the videothoracoscope while their mutual position can be changed during the procedure as needed (4). The camera-holding assistant should stand at the ipsilateral footstool side of the operator to achieve a better coplanar point of view. The camera head was often located at one end of the incision, in particular the upper edge, to minimize its interference on the surgical instruments. Towel clip can be used to fix the camera body, to increase the stability of the camera and reduce the camera holding assistant’s fatigue (5). The surgical steps of single port VATS lobectomy were same as those of the standard three access VATS lobectomy (6). The bronchus, vein, and artery were divided anatomically, and dissected separately using endoscopic staplers or legated. The dissection order varied as per the fissure development and the tumour location. Usually, in cases of lower or middle lobe lesions, the dissection order was vein first, and then artery and bronchus last. In the cases of upper lobe lesions, the dissection order would be switched to artery, vein, and bronchus. The lobe was removed in a specimen bag. Conventionally, systematic mediastinal lymph node dissection was performed after the removal of the affected lobe. A 28 Fr chest tube was inserted at the end of the operation, and this would be removed in case of no air leakage and when the volume of drainage was <200 per day (7). Sometimes, during uniportal VATS, the operating surgeon may find some difficulties both in the visualization and dissection of structures, as well as in the identification of the correct angles for instrumentation and endostaplers deployment. Changing the order of the instruments along the single port incision can sometimes help facilitate these manoeuvres, without the need to enlarge the incision or exert force onto the ribs. To improve ergonomics and to avoid meddling between individual instruments placed through the small incision of single-port VATS, a rapid progress in the instrument design has taken place (2).
Single port access VATS versus three port access VATS
The concept of minimally invasive surgery is not only preferred for reduction in the size of the external wound, but also for reduction in inner trauma, including the extent of tumour resection and lymph node dissection (8). VATS has become very popular since it was introduced. Surgeons have developed less-invasive procedures, using fewer and smaller-sized ports to reduce postoperative pain and chest wall paraesthesia and to improve cosmetic outcomes. Conventional three port access VATS is an effective standard surgical modality in the general thoracic surgery setting. VATS offers many advantages compared with thoracotomy, including better postoperative pulmonary function, less pain, shorter hospital stay, less blood loss, and fewer lung complications (9). Even if we routinely use in the daily life the three-port VATS access, thoracoscopy was originally conceived to be performed through a single incision. The different surgical approach to VATS surgery, introduced by the uniportal technique, makes it feasible and (even preferred) for situations where the chest drain is already in place (i.e., spontaneous pneumothorax, pleural effusion) or for resection of a small, peripherally pulmonary lesion. Also, single port access VATS can be an important adjunctive procedure in planning a complex pulmonary resection. Among possible clinical advantages, pain control after uniportal VATS has been reported to be superior to conventional, three-port access VATS. On the contrary, uniportal VATS versus three port access VATS have no significant differences between surgical material costs (4).
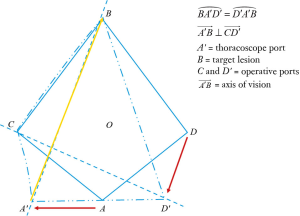
There are clear advantages of uniportal VATS. Only one intercostal space is involved with a decrease in postoperative pain when minor procedures are performed (10). The advantages of uniportal VATS technique could be related on a completely different geometric concept compared with conventional three port VATS (Figures 1-3). In fact, the approach to the target lesion in the lung is substantially similar to the approach that the surgeon would use in open surgery. A pure geometric explanation of the potential advantage of uniportal VATS compared with conventional three port access VATS lies in the projective plane of the sagittal approach to the target lesion, which preserves the depth of intraoperative visualization provided by the currently available two-dimensional flat video monitors. Conversely, the torsion plane created along the trapezoid space obtained with conventional VATS using the laterolateral approach gives a distinct visualization of the perspective, deep operative field (3). Nevertheless, the single incision should be placed on a direct line leading to the target area but at a distance sufficient to allow deploying of the articulating arms of endograsps and endostaplers. In fact, in the lateral decubitus position, articulating instruments, like robotic arms, clearly adapt to the fixed dome-shaped volumetry of the pleural cavity (12).

The success and adaptability of the single-port access technique in the treatment of various thoracic diseases have made them hugely popular around the world. Sometimes the surgeon may find a difficult visualization and dissection of structures, or the correct angles for endostaplers deployment. Angulated and narrow-shaft double-hinged instruments and flexible endostaplers have become part of the essential armamentarium for the single port access VATS. These instruments (derived from the thoracic surgeons’ requests) allow better instrument manipulation, reduce instrument fencing, decrease the need for torquing, and permit difficult stapling angles. Over the years, scopes have become thinner, and have more visual versatility and clarity to allow smaller surgical incisions and reduce interference with other instruments. A possible future development will be the use of wide-angle thoracoscope, or the three dimensional cameras. In the near future, multiple small remote wireless video cameras can be placed into the thoracic cavity, being stuck then against the inner chest cavity by magnetic anchoring and guidance systems camera. Although initially developed for single-incision laparoscopy, these cameras may be more suited for thoracic surgery because the rigidity of the chest wall provides more stability and less movement for magnetic anchorage when compared with the abdomen (13).
The combination of more specialized instruments and thoracoscope will be the key to facilitating the growth of single port VATS (14). It has been described that uniportal VATS have an effect on early postoperative pain, with a significant reduction in the pain scores in the first days postoperatively. However, all the published studies were small, non-randomized and unblended, and, therefore, susceptible to various forms of bias (15).
Therefore, uniportal VATS is becoming accepted worldwide for minor and major procedures to treat thoracic and mediastinal pathologies. To date, there are no results of randomized controlled trials to compare the role of minimally invasive techniques and open procedures. However, the non-randomized evidence has shown that minimally invasive techniques in thoracic surgery are feasible and associated with less postoperative morbidity and fast recovery allowing the early begin of adjuvant therapy when necessary. The one year survival and the three years survival of patients after VATS is at least equivalent to open procedures, with a trend towards better survival at 5 years with a VATS approach (16). On the other hand, most available literature focused on the feasibility and safety of single port access thoracoscopic lobectomy, without a comparison with three-port access VATS. Analysing the differences of clinical data between single port thoracoscopic lobectomy and triple port thoracoscopic lobectomy for non-small cell lung cancer, there were no significant differences in perioperative mortality and complications. Performing lymph node dissection through the single port access technique remains challenging. Not only in uniportal studies, but also in studies using multiport access or open techniques, large differences in overall performances and quality of lymph node dissection have been observed. Uniportal VATS lobectomy is technically safe to treat patients with lung cancer. Nevertheless, as far as lymph node dissection is concerned, there were no significant differences between accesses regarding also the mediastinal lymph node harvest. Fragmentation of lymph nodes is sometimes inevitable, being preferable to dissect the lymph nodes in an en-bloc fashion, particularly in the mediastinal area. The method used by pathologists to calculate the number of lymph nodes relies on counting the specimens: in pieces (counted as one if they were connected) or in an en-bloc style (dissection of the specimen and count of the lymph node numbers in each station). These methods used by pathologists have not changed with time with the transition from the three-port access to the uniportal technique. However, some tricks and tips are necessary to harvest more lymph nodes, including the use of modified instruments such as longer and curved suckers or thoracoscopic instruments to avoid clashing of instruments. For right-side lymph node dissection and left-side superior mediastinal lymph node dissection, the technique is similar to the three port access VATS. However, it is sometimes quite challenging to expose the left-side subcarinal area by the uniportal technique (17). Therefore, the lymph node dissection in uniportal VATS is at least equivalent to that by open surgery and in other words met the oncologic requires (18).
The application of VATS technique marked in thoracic surgery a milestone innovation. However, there is often a long learning curve for the conversion from the conventional open surgery to VATS surgery. While the triple-port VATS has been widely recognized, the adoption of the single-port VATS is perhaps more challenging. This kind of surgery requires close cooperation with the anaesthesiologist (to maintain good collapse of the lung on the operated side), and with the camera-holding assistant (6). In three-port access VATS, an upper lobectomy was usually challenging during the dissection along the truncus anterior branch of the pulmonary artery; on the other hand, in single port access VATS lobectomy, the mobilization of the apical branch was switched as the first step. Therefore, in that order, the identification and dissection were clear through the incision located at the fourth intercostal space, with an improved visualization. Meanwhile, for the safety of our patients, or if the operation ran into difficulty, additional ports would be favoured (7). The surgeon who want start to learn uniportal VATS, could feel uncomfortable placing the instruments through the same port, and, furthermore, having to share that port with a video-thoracoscope. During this time, it may be useful to use of curved or right-angled instruments to facilitate dissection. Uniportal VATS is a part of the evolution of VATS, so when we encountered difficulties, we can use the same solutions used in other forms of VATS.
In the early days of VATS, VATS lobectomies were nursed and rehabilitated the same as an open lobectomy. A fast track protocol should cover every aspect of nursing, physiotherapy, mobilization schedules, perioperative investigations, pain management, chest drain management, nutrition, communication with the family, and so on. On the other hand, the use of a digital chest drainage system connected to the patient’s chest tube may facilitate the task; the patient is not tied down and can freely mobilize even on the same day of surgery. Also, the negative pressure level is regulated very precisely, avoiding variations that may prolong post-operative air leaks (1). A limit in the uniportal VATS approach could be the mutual interference between instruments. Since the single-port VATS is performed via the sagittal plane, in a caudal-to-cranial direction, the eyes and hands are used at the same level during the operation; thus, a reverse observation plan should be avoided. The impact of the quality of camera holding on the VATS encompasses several aspect of the whole process, including ergonomic, accuracy, operative time and safety issues as well. A qualified assistant must have flexible camera-holding skills, be familiar with the detailed surgical procedures, understand and support the operational habits of the operator, and have complete, long lasting teamwork experiences (19,20). The single port VATS approach may further reduce access trauma and has brought about a new line of thought on the role of an awake non-intubated technique in fast-tracking patients postoperatively (2). Technologic advancements aimed at manufacturing custom-made instrumentation for thoracoscopic surgery will be equally decisive in facilitating the single-port technique under local or loco regional anaesthesia (12).
Conclusions
Uniportal VATS is not a Manichean law because there are many steps between open thoracotomy and Uniportal VATS. Since Uniportal VATS is another step in the evolutionary process, the same basic principles and techniques of conventional VATS are all applicable. This reassurance of familiarity should help guide the learning of the single port access VATS. In thoracic surgery, a skilled surgeon alone cannot master all the new approaches or techniques. In order to do so, training of the assistants, involvement of the multi-disciplinary team, introduction of appropriate complementary technology becomes of the foremost importance. Although the increasing application of single-port VATS has brought about new challenges both for the surgeon and for the industry that provides us the technology to push the boundaries of surgery, it has also created unique opportunities for collaboration. As visualization technology advances further, the case for VATS strengthens incrementally. Nevertheless, it is natural that minimally invasive thoracic surgery will keep on developing, since VATS is a never-ending story and Uniportal VATS is not the end of this history.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17.
- Ng CS. Single-port thoracic surgery: a new direction. Korean J Thorac Cardiovasc Surg 2014;47:327-32. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5:S214-6. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [Crossref] [PubMed]
- Zhu Y, Xu GB, Lei CG, et al. Thoracic surgery: single-port video-assisted thoracoscopic lobectomy. Ann Transl Med 2015;3:143. [Crossref] [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-i53. [Crossref] [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [Crossref] [PubMed]
- Son BS. Small Single-Incision Thoracoscopic Surgery Using an Anchoring Suture in Patients With Primary Spontaneous Pneumothorax: A Safe and Feasible Procedure. Ann Thorac Surg 2015;100:1224-9. [Crossref] [PubMed]
- Anile M, Diso D, Mantovani S, et al. Uniportal video assisted thoracoscopic lobectomy: going directly from open surgery to a single port approach. J Thorac Dis 2014;6:S641-3. [Crossref] [PubMed]
- Bertolaccini L, Terzi A, Viti A. Comparison of the three-port access VATS versus the uniportal VATS access. Asvide 2016;3:080. Available online: http://www.asvide.com/articles/833 [Crossref] [PubMed]
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Ng CS, Wong RH, Lau RW, et al. Single port video-assisted thoracic surgery: advancing scope technology. Eur J Cardiothorac Surg 2015;47:751. [Crossref] [PubMed]
- Ng CS, Wong RH, Lau RW, et al. Minimizing chest wall trauma in single-port video-assisted thoracic surgery. J Thorac Cardiovasc Surg 2014;147:1095-6. [Crossref] [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [Crossref] [PubMed]
- Ismail M, Helmig M, Swierzy M, et al. Uniportal VATS: the first German experience. J Thorac Dis 2014;6:S650-5. [Crossref] [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-i72. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [Crossref] [PubMed]
- Zhu Y, Xu G, Zheng B, et al. Single-port video-assisted thoracoscopic surgery lung resection: experiences in Fujian Medical University Union Hospital. J Thorac Dis 2015;7:1241-51. [Crossref] [PubMed]
- Sehgal R, Cahill RA. Advanced laparoscopic surgery for colorectal disease: NOTES/NOSE or single port? Best Pract Res Clin Gastroenterol 2014;28:81-96. [Crossref] [PubMed]
Cite this article as: Bertolaccini L, Terzi A, Viti A. Why should we prefer the single port access thoracic surgery? J Vis Surg 2016;2:43.


