Robot-assisted approach to a retrorectal lesion in an obese female
Introduction
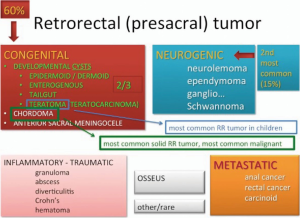
Presacral or retrorectal tumors are rare, corresponding to an incidence of 1 in 40,000 admissions in major metropolitan medical centers per year (1). Often times found incidentally, retrorectal masses, such as cystic lesions, can be asymptomatic in up to 50% of cases (2). Categorized broadly into congenital, neurogenic, inflammatory, osseous and miscellaneous, 45–50% are malignant or contain malignant degeneration (Figure 1). Once diagnosed, surgery is often required for the treatment of a retrorectal lesion secondary to the possibility of a false negative benign lesion, malignant degeneration, and risk of symptom or disease progression (3). Resection of presacral tumors can be done via an abdominal, posterior, or combined approach depending on the size, location of the tumor relative to S3, and relationship to the pelvic sidewall. Generally, an anterior abdominal approach for resection is undertaken for tumors above the mid level of S3 or with involvement of the pelvic sidewall; and a posterior approach for resection of tumors below the mid-level of S3 (1). The laparoscopic approach to retrorectal tumors has shown safety, efficacy, shorter length of hospital stay, and no increase in intraoperative complications (4-6). However, laparoscopy in the pelvis has lower threshold for conversion to open procedures compared to robotic approach as seen in the total mesorectal excision (TME) literature (7-9). Risk factors for conversion to an open procedure with laparoscopic approach to retrorectal tumors include large tumor size, obesity and high American Society of Anesthesiologist Physical Status (ASA) (1,10). Limited ergonomics of laparoscopic equipment, augmented by a narrow pelvis and obesity could exacerbate technical difficulty and lead to conversion. The stability of the robotic platform, enhanced optics, and improved dexterity with wristed instrumentation has led to the application of the robot to retrorectal mass excision. A recent case series of five patients indicated that a robotic approach to presacral tumors has decreased intraoperative blood loss and length of hospitalization as compared to an open approach (11). In that series patients’ body mass index (BMI) was not known. We present an emerging technique of a minimally invasive robotic approach to a retrorectal cystic lesion in an obese 35-year-old female.
Methods
Patient selection and workup
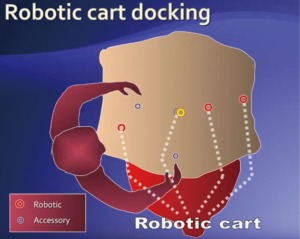
A 35-year-old obese female (BMI 41 kg/m2) was found to have a retrorectal mass identified incidentally on CT of the abdomen/pelvis for abdominal pain. The etiology of the abdominal pain was calculous cholecystitis which was subsequently treated with a laparoscopic cholecystectomy. The mass was barely palpable on digital rectal examination. An MRI revealed a 2-cm cystic lesion originating from the left pelvic sidewall at mid-rectal level below the piriformis muscle, indenting the mesorectal fascia posteriorly and to the left (Figure 2). At an outside institution, after a normal colonoscopy, she underwent a CT guided biopsy of the mass. Pathology revealed fragments of a cyst wall with atypical glandular cells. Immuno-histo-chemistry was non-diagnostic; cytomorphology was suggestive of a metastatic well differentiated neuroendocrine tumor or a malignant degeneration of a tail-gut cyst. PET scan was negative. Secondary to possible malignant degeneration and its involvement with the pelvic sidewall, the patient was offered a resection of the mass via a minimally invasive trans-abdominal approach. A robotic platform was ideally suited for mobilization of the lateral posterior mesorectum and excision of the presacral cyst.
Preoperative preparation
Preoperative preparation included a complete blood count, electrolytes, renal, and liver function tests. Mechanical bowel preparation was administered one day before the operation and the patient was fasting at least 6 hours pre-operatively. Antibiotic prophylaxis was administered within 30 minutes of incision. Appropriate consent has been obtained from the patient per our institutional protocol.
Equipment preference card
- DaVinci Surgical System (Intuitive Surgical Inc., Sunnyvale, CA);
- Laparoscopic setup;
- Exploratory laparotomy tray (on standby);
- 8 mm robotic trocars ×3;
- Cadiere forceps (bipolar attachment);
- Monopolar electrocautery hook;
- Atraumatic bowel grasper;
- 0° 12 mm laparoscopic camera;
- 12 mm trocar.
Procedure
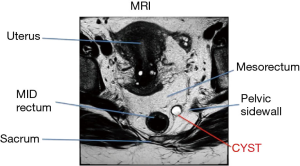
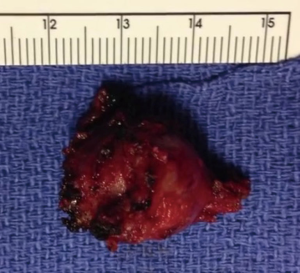
After induction of anesthesia, an oro-gastric tube and Foley catheter were placed. Digital rectal examination revealed a left lateral rectal wall mass approximately 3 cm in size located 7 cm from the anal verge. The patient was placed in a modified lithotomy (Lloyd-Davies) position. The abdomen and perineum were prepped and draped in a sterile fashion. A total of six ports were placed in the following positions. A camera port (12 mm) was placed supra-umbilically. Three 8-mm robotic ports included: (I) arm 1, right iliac fossa above and medial to anterior superior iliac fossa; (II) arm 2, along the left mid-clavicular line, slightly more cephalad than the camera port; (III) arm 3, in the left upper quadrant. Two 5-mm laparoscopic assistant ports were placed in the following manner: (I) right upper quadrant, mid-clavicular line; (II) supra-pubic, right of mid-line. Beginning laparoscopically, the small bowel was cleared out of the pelvis using atraumatic graspers and held in place by the assistant. The uterus was suspended out of the pelvic field. The robotic cart was then docked between the patient’s legs (Figure 3). The sigmoid colon was pulled out of the pelvis and held taut against the pelvic sidewall by one of the robotic arms. The robotic posterior mesorectal dissection began with the incision of the peritoneum overlying the right leaf of the mesocolon above the promontory allowing access to the presacral plane (Figure 4). At this point we identified the hypogastric nerves taking care to avoid injuring them. The mesorectal plane was progressively developed in the standard fashion for rectal dissection. Excessive fat was encountered within the Toldt’s fascia as well as the presacral fascia making the dissection more challenging than usual. Prehypogastric nerve fascia was incised allowing entrance into the areolar holy plane with dissection continuing to the level of the lower sacrum. At this point the dissection was eccentric and directed towards the left hemi-pelvis where an abnormal presacral vessel was identified leading to the mass originating from the left posterior endopelvic fascia. The endopelvic fascia was incised carefully around the mass with meticulous dissection and slowly became more evident in the inferior aspect of the pelvic sidewall fat pad. The ability of retraction, superb optics, and un-paralleled precision of dissection facilitated the dissection, justifying the chosen robotic approach. The lateral location of the lesion to the sacrum along with an anterior extension from the mass resembling a nerve structure initially suggested a neurogenic origin of the tumor. Once the anterior aspect of the lesion was released, it was used for retraction and the mass was dissected off the pelvic sidewall with ease. The mass was retrieved with an endo-catch bag. After ensuring careful hemostasis and lavage, the 12-mm port site was closed with figure of eight stitch of 0-vicryl. The abdomen was de-sufflated and the remaining port sites closed. No drain was left in place. Total operative time was 150 minutes; robotic docking was 5 minutes; robotic dissection 70 minutes. The final pathology revealed a benign Mullerian type cyst, 2.2 cm in greatest dimension (Figure 5).

Postoperative management
The patient was managed with standard protocols for minimally invasive surgery. Clear liquid diet was started on post-operative day 1 along with the removal of the Foley catheter. On post-operative day 2, once general diet was tolerated and pain controlled with oral analgesics, the patient was discharged. She had returned to normal activity within 72 hours.
Results
Tips, tricks and pitfalls
- Diagnosis, investigation, and approach to retrorectal (presacral) tumors are complex.
- Although good concordance of biopsy results and final pathology has been shown for a solid presacral lesion, caution must be exercised with biopsy result with cystic presacral lesions as they are inaccurate.
- Benign presacral lesions should be resected secondary to complications such as infection, local growth and compression, possibility of containing malignancy, and malignant degeneration.
- Definitive diagnosis of primary malignancy of retrorectal tumor warrants an en-bloc resection.
- Anterior abdominal approach is reserved for tumors above mid-level of S3, or if involving the pelvic sidewall. There is also growing evidence that anterior approach using minimally invasive techniques can often be used successfully for most lesions, including those located below S3 level.
- Only when the small bowel, uterus, and sigmoid colon are effectively retracted can robotic dissection commence.
- Access to the retrorectal space begins with incision of the peritoneal leaf at the sacral promontory.
- Care must be taken when moving laterally in the retrorectal space to avoid injury of the ureter, iliac vessels (mainly veins), hypogastric nerves and the pelvic plexus.
- Incision of prehypogastric nerve fascia allows entrance into the areolar holy plane facilitating dissection into the lower level of the sacrum.
Conclusions
Robot-assisted minimally invasive resection of a retrorectal mass is safe and feasible. This method can be particularly useful in the narrow pelvis and with obese patients.
Acknowledgements
The authors would like to acknowledge the James R. & Helen D. Russell Institute for Research and Innovation at Advocate Lutheran General Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent:Written informed consent was obtained from the patient for publication. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Toh JW, Morgan M. Management approach and surgical strategies for retrorectal tumours: a systematic review. Colorectal Dis 2015. [Epub ahead of print]. [Crossref] [PubMed]
- León-Brito H, Fraile González M, Oquiñena Legaz S, et al. Cystic tumors in the retrorectal space. Do these two cases have something in common? An Sist Sanit Navar 2014;37:151-6. [PubMed]
- Jao SW, Beart RW Jr, Spencer RJ, et al. Retrorectal tumors. Mayo Clinic experience, 1960-1979. Dis Colon Rectum 1985;28:644-52. [Crossref] [PubMed]
- Kye BH, Kim HJ, Cho HM, et al. Clinicopathological features of retrorectal tumors in adults: 9 years of experience in a single institution. J Korean Surg Soc 2011;81:122-7. [Crossref] [PubMed]
- Nedelcu M, Andreica A, Skalli M, et al. Laparoscopic approach for retrorectal tumors. Surg Endosc 2013;27:4177-83. [Crossref] [PubMed]
- Fong SS, Codd R, Sagar PM. Laparoscopic excision of retrorectal tumours. Colorectal Dis 2014;16:O400-3. [Crossref] [PubMed]
- Hellan M, Anderson C, Ellenhorn JD, et al. Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol 2007;14:3168-73. [Crossref] [PubMed]
- Baek SJ, Al-Asari S, Jeong DH, et al. Robotic versus laparoscopic coloanal anastomosis with or without intersphincteric resection for rectal cancer. Surg Endosc 2013;27:4157-63. [Crossref] [PubMed]
- Pai A, Marecik SJ, Park JJ, et al. Oncologic and Clinicopathologic Outcomes of Robot-Assisted Total Mesorectal Excision for Rectal Cancer. Dis Colon Rectum 2015;58:659-67. [Crossref] [PubMed]
- Duclos J, Maggiori L, Zappa M, et al. Laparoscopic resection of retrorectal tumors: a feasibility study in 12 consecutive patients. Surg Endosc 2014;28:1223-9. [Crossref] [PubMed]
- Oh JK, Yang MS. Robotic resection of huge presacral tumors: case series and comparison with an open resection. J Spinal Disord Tech 2014;27:E151-4. [Crossref] [PubMed]
- Eftaiha SM, Kochar K, Marecik SJ, et al. The robot assisted technique for the resection of the retrorectal or presacral lesion. Asvide 2016;3:185. Available online: http://www.asvide.com/articles/941
Cite this article as: Eftaiha SM, Kochar K, Pai A, Park JJ, Prasad LM, Marecik SJ. Robot-assisted approach to a retrorectal lesion in an obese female. J Vis Surg 2016;2:59.