Pectus bar removal: surgical technique and strategy to avoid complications
Introduction
Minimally invasive surgical repair of pectus excavatum using pectus bars is a widely accepted technique. Pectus bar removal is the final stage of this procedure (1). The important questions to be answered regarding bar removal include the appropriate duration of bar maintenance, techniques for removal, and strategies to avoid complications. To address these issues, we review our experience of bar removal in one of the largest series of pectus deformity repair, which was performed with our modification of pectus bar implantation technique and devices (2). The aim of this study is to describe the technique of bar removal and to disclose the complications that occurred and countermeasures to avoid them.
Patients and methods
Between September 1999 and August 2015, we operated on 2,553 patients with pectus excavatum and carinatum using pectus bars for a minimally invasive approach. Among them, 1,821 patients (71.3%) underwent pectus bar removal as a final stage of pectus deformity repair, and their data were analyzed retrospectively to identify the outcomes and adverse effects of the pectus bar removal procedure. The mean age of the patients was 9.13 years (range, 16 months to 44 years) and the male to female ratio was 3.55.
Surgical techniques of the procedure
Under general anesthesia with a single-lumen endotracheal intubation, the patient was positioned supine with their arms hanging freely to the overhead strut of the ether screen. Both groins were prepared and draped routinely for emergency cardiopulmonary bypass via femoral artery and vein cannulation in case of bleeding during bar removal.
Previous lateral skin incisions on both sides were reopened after infusion of local anesthetic around the incision sites. The pectus bar(s) and fixation hardware were identified in the extrathoracic subcutaneous area. The fixation devices, such as the stabilizer (Walter Lorenz, Jacksonville, FL, USA) in our initial experience, the pericostal wires including their broken fragments, and the claw fixators (Primemed, Seoul, Korea) that were used more recently, were carefully dissected and pulled out. The pectus bar was mobilized and the tips of the bar were withdrawn through the skin incision bilaterally. With the aid of the bar flipper, both ends of the bar were straightened by manual force, which made the arc of the bar smooth and allowed it to slip out without resistance (Figure 1).

In some cases, especially in adult patients, we found that the bar tips were buried in overgrown osseous tissue from the adjacent ribs. In those instances we had to dig the bars out with the aid of an osteotome or rongeur dissection, or by electric drilling of the bone in tightly sealed cases (Figure 2). When the lateral side of the pectus bar in the subcutaneous plane could be identified, the Hercules device (Primemed, Seoul, Korea) was introduced from the side of the bar without bar tip exposure (Figure 3). Exertion of manual pressure with the Hercules device on the side of the bar forced the tips out from the osseous burial (Figures 4,5). After bar removal, the hinge plates (Primemed, Seoul, Korea) were removed when indicated (Figure 6). The incisions were closed in layers, usually without drainage.





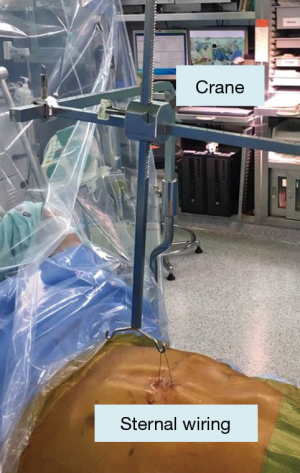
In special situations such as malpositioned pectus bars, crane elevation of the sternum by means of sternal wire suturing was applied without hesitation to avoid possible injury to internal organs (Figure 7). The crane lift assures safety from injury while pulling out the bar by reducing the pressure on the bar and the organs, and by separating the bar from the internal organs.
Upon completion of the bar removal procedure, a portable chest radiograph was taken in the operating theater to confirm that there was no remaining hardware, pneumothorax, or other abnormalities of the intrathoracic organs.
This study was approved by the Institutional Review Board (IRB) of our hospital.
Results
The mean duration of pectus bar maintenance was 2.57 years (range, 4 months to 14 years). By age, the mean duration was 2.02 years (range, 4 months to 7 years) for children under 12 years, 2.99 years (range, 7 months to 9 years) for teenagers aged 12–20 years, and 3.53 years (range, 3 months to 14 years) for adults over 20 years. A total of 48 patients (2.6%) underwent bar removal more than 5 years after bar insertion. Fifty-eight patients (3.2%) underwent bar removal earlier than initially planned. The most common reason for early bar removal was wound infection with chronic seroma. The reasons for early bar removal are shown in Table 1.
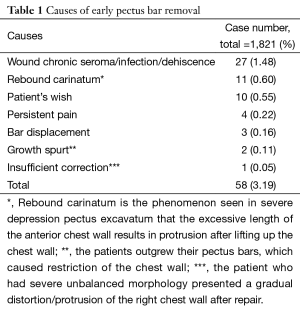
Full table
The most common adverse reaction after bar removal was wound seroma including infection (43 patients, 2.36%). Other complications are listed in Table 2. Recurrence after bar removal occurred in nine patients (0.49%), and seven required redo repair (0.38%).
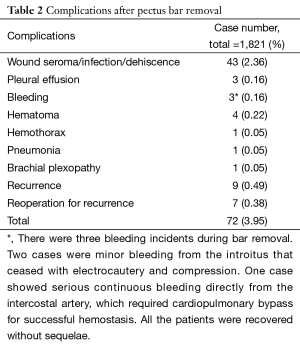
Full table
There has been no mortality related to pectus repair or bar removal in our series.
Discussion
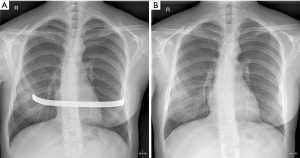
Pectus bar removal as a final stage of minimally invasive repair of pectus excavatum and carinatum is generally an easy procedure (1). Our policy is to maintain the bar for 2 years for pediatric patients up to 12 years old; 2.5 years for teenagers between 12 and 20 years old; and 3 years for adults over 20 years. Initially, we recommended that adults keep their bars for up to 5 years but with accumulating experience this was adjusted to 3 years. The longest duration was 14 years in a 22-year-old patient who was lost to follow-up and ended up delayed bar removal. Bar removal for her was uneventful with a decent result of repair without chest wall constriction (Figure 8).
There are several different techniques to facilitate removal of the bar. An intrathoracic bar that has been in place for more than a month cannot be flipped back, and needs to be pulled out after straightening or with the patient in a different position to allow the curved bar to slip out.
Techniques to remove the bar without straightening include using two operating tables in a T-shaped configuration to clear the lateral chest wall (8), or placing the patient in the prone position (9). We find the two-table technique cumbersome and consider the prone position potentially hazardous in the case of incidents such as bleeding or vital organ instability because access to the inside of the chest is difficult.
Our technique for bar removal involves a maneuver that straightens the bar tips following the internal curvature of the bar to allow it to easily slide out, and then pulling the curvilinear bar out from either side. This technique permits smooth and straightforward removal, as confirmed by others (10).
One unique feature that we see in pectus bar removal is callus formation around the bar, especially at the tips of the bar (11,12). It has been observed that submuscularly placed bars have a greater tendency of callus formation than subcutaneous bars (13). In these instances, dissecting the bar out of the bony overgrowth can be tedious. In most cases the buried bar could be released with an osteotome or rongeur, but occasionally dissection with an electric drill was required. Invariably, callus formation occurs at the end of the bar and the body of the pectus bar was free from bony burial such that the lateral side of the bar could be dissected easily. Based on this observation, we developed an instrument called the Hercules to relieve the hold of the callus on the bar (Figure 3). The Hercules is designed to be introduced from the side of the bar instead of the tip of the bar that is buried in the callus (Figure 9). Once the Hercules is in position, the bar is bent manually and the callus can be broken to deliver the bar out of the wound without the need for total dissection to the tip of the bar (Figure 5).
In our earlier experience, removal of the stabilizer and pericostal wire sutures were difficult. Especially when the wires were broken into pieces, we had to find wire fragments with an aid of C-arm fluoroscopy. After using the claw fixator (15) and bridge devices (16), the procedure was sped up and became simpler.
With current techniques, the bar removal procedure is generally considered safe and straightforward (1), although there have been serious complications, including life threatening internal bleeding (17-19). In cases reported in the literature, such complications arose because of poor bar position (18) or sternal erosion (19). Another cause of bleeding was terminal serration of the bar (20), which was different from our bar design with smooth tips.
In our early experience, we experienced bleeding during bar removal in three patients (Table 2). In two cases, the bleeding evidently came from the introitus of the chest wall entrance and was uneventfully controlled with electrocautery and gauze compression. However, in one patient who bled from the intercostal artery deep in the chest cavity, we had to utilize cardiopulmonary bypass support for successful control of the hemorrhage. All the patients who bled during bar removal recovered well postoperatively.
The only troublesome problem is wound seroma and dehiscence, which seems to be due to residual space occupied by the bar and hardware in the subcutaneous pocket and connection to the pleural space where fluid is normally generated. The postoperative hospital stay is one day and return to normal life is rapid in the majority of cases.
Conclusions
By analyzing the data of pectus bar removal from our large series of pectus repair, we addressed the issues of duration of bar maintenance, technique of bar removal, complications, and the counter-measures to avoid complications. Our results indicated that pectus bar removal is a straightforward and patient recovery is fast.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: The IRB has exempted the informed consent from every patient in this study due to this is a retrospective chart review without revealing any patients’ personal data.
References
- Nyboe C, Knudsen MR, Pilegaard HK. Elective pectus bar removal following Nuss procedure for pectus excavatum: a single-institution experience. Eur J Cardiothorac Surg 2011;39:1040-2. [Crossref] [PubMed]
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Park HJ, Kim KS. Technique for pectus bar removal in an 8-year-old male patient after 2 years of bar implantation: a single bar and claw fixators are removed through the previous incision. Asvide 2016;3:173. Available online: http://www.asvide.com/articles/929
- Park HJ, Kim KS. Technique for removal of callus around the tip of the pectus bar: osteotome and rongeur dissection to release the bar from the osseous burial. Asvide 2016;3:174. Available online: http://www.asvide.com/articles/930
- Park HJ, Kim KS. Pectus bar removal with the Hercules device. Asvide 2016;3:175. Available online: http://www.asvide.com/articles/931
- Park HJ, Kim KS. Technique for freeing the pectus bar from the callus by using the Hercules: exertion of manual pressure with the Hercules device on the side of the bar forced the tips out from the osseous seal. Asvide 2016;3:176. Available online: http://www.asvide.com/articles/932
- Park HJ, Kim KS. Technique for removal of the hinge plate. Asvide 2016;3:177. Available online: http://www.asvide.com/articles/933
- St Peter SD, Sharp RJ, Upadhyaya P, et al. A straightforward technique for removal of the substernal bar after the Nuss operation. J Pediatr Surg 2007;42:1789-91. [Crossref] [PubMed]
- Chon SH, Shinn SH. A simple method of substernal bar removal after the Nuss procedure. Eur J Cardiothorac Surg 2011;40:e130-1. [PubMed]
- Noguchi M, Fujita K. A new technique for removing the pectus bar used in the Nuss procedure. J Pediatr Surg 2005;40:674-7. [Crossref] [PubMed]
- Morimoto K, Imai K, Yamada A, et al. Migration of a pectus bar into the ribs. J Plast Reconstr Aesthet Surg 2008;61:225-7. [Crossref] [PubMed]
- Giacomo TD, Diso D, Francioni F, et al. Minimally invasive pectus excavatum repair: migration of bar and ossification. Asian Cardiovasc Thorac Ann 2013;21:88-9. [Crossref] [PubMed]
- Ostlie DJ, Marosky JK, Spilde TL, et al. Evaluation of pectus bar position and osseous bone formation. J Pediatr Surg 2003;38:953-6. [Crossref] [PubMed]
- Park HJ, Kim KS. Comparison of application of bar flipper and Hercules: the Hercules is designed to be introduced from the side of the bar, whereas the flipper only can be applied at the tip of the bar. Asvide 2016;3:178. Available online: http://www.asvide.com/articles/934
- Park HJ, Kim KS, Lee S, et al. A next-generation pectus excavatum repair technique: new devices make a difference. Ann Thorac Surg 2015;99:455-61. [Crossref] [PubMed]
- Park HJ, Kim KS, Moon YK, et al. The bridge technique for pectus bar fixation: a method to make the bar un-rotatable. J Pediatr Surg 2015;50:1320-2. [Crossref] [PubMed]
- Jemielity M, Pawlak K, Piwkowski C, et al. Life-threatening aortic hemorrhage during pectus bar removal. Ann Thorac Surg 2011;91:593-5. [Crossref] [PubMed]
- Haecker FM, Berberich T, Mayr J, et al. Near-fatal bleeding after transmyocardial ventricle lesion during removal of the pectus bar after the Nuss procedure. J Thorac Cardiovasc Surg 2009;138:1240-1. [Crossref] [PubMed]
- Notrica DM, McMahon LE, Johnson KN, et al. Life-threatening hemorrhage during removal of a Nuss bar associated with sternal erosion. Ann Thorac Surg 2014;98:1104-6. [Crossref] [PubMed]
- de Campos JR, Das-Neves-Pereira JC, Lopes KM, et al. Technical modifications in stabilisers and in bar removal in the Nuss procedure. Eur J Cardiothorac Surg 2009;36:410-2. [Crossref] [PubMed]
Cite this article as: Park HJ, Kim KS. Pectus bar removal: surgical technique and strategy to avoid complications. J Vis Surg 2016;2:60.


