Minimally invasive repair of pectus carinatum and how to deal with complications
Introduction
The minimally invasive technique that addresses the correction of the pectus carinatum deformity is described in this document showing the achievements since the first introduction of the innovation reported in 2005 (1) and 2009 (2).
Ravitch [1952, 1960] (3), Robicsek et al. [1963] (4), Welch and Vos [1973] (5) and Lester [1953] (6), introduced the open techniques that still remain without modifications and provide acceptable results although they require large incisions, the creation of large skin and muscle flaps, the resection of costochondral arches and sternal osteotomies. These procedures are laborious and have the disadvantage of leaving sequelae such as keloid scars. We have innovated the surgical field introducing this pectus carinatum technique that avoids these difficulties. The correction is based in aspects like adequate elasticity of the thoracic wall, obtaining very good results compressing the sternochondral region by implanting a metal bar in the pre-sternal region and securing it bilaterally to the posterolateral portion of the costal arches.
The new implant (Steel Rib) consists of a compression strut and stabilizing plates made of 316 L steel that remain implanted until remolding of the chest contour is achieved. Unlike the resection method, the compression procedure achieves corrections avoiding extensive cutaneous incisions, large skin and muscle flaps, resection of variable portions of the costochondral arches, sternal osteotomy and various forms of reconstruction including muscle preimplantation, obtaining comparable results in the chest wall and, similarly than in the Nuss technique treatment of pectus excavatum (7,8), this technique for the correction of pectus carinatum has none of the disadvantages associated with open techniques.
Patient selection and workup
The efficiency of this procedure is connected with the appropriate selection of patients. The degree of the elasticity of the thoracic wall is the key factor. By performing a physical examination we can compress the useful spot of the protruded area and evaluate the potential result that could be achieved. The ideal patient is the one that has not completed his/her growth, one who has symmetric form, one who belongs to a chondro-gladiolar clinical shape, and one who has no lateral depressions or flared ribs.
With lateral radiology we can determine the persistency of cartilage tissue and degree of calcification.
Although leptosomic and marfanoid patients often present malformations of large dimensions, they frequently show a particular flexibility.
Individual interviews with family members and psychological consultations are important. In those cases that require correction of minor deformities, or when they show personality conflicts, we should act with caution before recommending surgical repairs.
The rigid forms are appropriate for pre-operative treatment with compressive massages, kinesiotherapy and orthesis brace during a limited period of time of approximately two months with frequent sessions. These steps help to reach adequate compression during surgery.
We do not recommend surgery in babies. We recommend brace therapy for them.
Patients between 8 and 10 years old are often candidates for orthesis treatment.
Those with chondromanubrial form do not qualify for this procedure.
The asymmetries that have severe contralateral pectus excavatum require complex procedures.
Patients with extreme rigidity, patients who are older, or those with complex anomalies must be corrected with open techniques.
Pre-operative preparation
The analysis of the patient implies a detailed clinical examination, taking into account the background of relatives focusing on genetic diseases.
Malformation traits are documented with photography.
Allergy to metals is investigated through a written questionnaire and chromo and nickel sensitivity tests.
Considerations concerning the need for correction and its magnitude come from the questioning of the patients and parents. The surgeon must take into account the situation he may find when the mother and father disagree about the necessity of the repair.
Lab studies and coagulation tests are routine as well as cardiologic studies such as ECG and echocardiogram.
Cardiologic pathology frequently associated with the malformation must be discarded. The functional respiratory examination and psychological consultation are also part of the routine.
In most cases only the front and lateral thoracic radiology are enough to evaluate the lung, the position of the heart and the persistency of the sternal cartilage. Although we do not request it on a routine basis, the CT SCAN with 3D reconstruction may be useful, particularly before the presence of contralateral pectus excavatum. The presence of scoliosis must be investigated especially in the asymmetric forms.
The different therapeutic alternatives will appear from the physical examination. Symmetry, rigidity of the thoracic cage, anomalies in the floating ribs, contralateral pectus excavatum, etc., must be thoroughly evaluated.
The elasticity of joints is examined as an indicator of the pliability of the thoracic wall.
Manual compression of the protruded region is enough to evaluate the degree of correction that can be achieved through this minimally invasive technique.
Equipment preference card
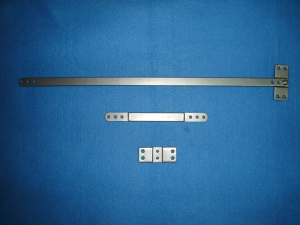
We need regular and special instruments. The special instruments that this technique requires are (Figures 1,2):


- Periosteal rib raspatories of different types for costo-chondral dissection (N: 12);
- Curved instruments for going around the costal arcs without opening the pleural cavity (N: 11);
- Tubes of polyvinylchloride (PVC) of small diameter to be linked to the curved instruments and to be located around the costal arcs;
- Trocars to be inserted in the pre-sternal tunnel (N: 2);
- Tubes of PVC of large diameter to be inserted (guided by the trocars) under the muscular level. These tubes will make the insertion of the compressive bar easier (N: 13);
- Steel wires of different calibers to be implanted in the pericostal location (N: 3);
- Templates for facilitating the appropriate design of the elongated bar (N: 6);
- Implantable elongated compressive bars of different lengths for pre-sternal location. These bars have three holes at both ends (Figure 3);
- Implantable plates with central threaded holes along a groove to be linked to the elongated bars, and four not threaded holes to be linked by the wires to the costal arcs (N: 16);
- Implantable screws of several sizes and shapes designed to link the plate with the compressive bar (N: 15);
- A long scissors to build a pre-sternal tunnel (N: 14);
- A hook to guide the compressive bar during its implantation and removal (N: 5);
- Templates of the same length of the bars for helping the surgeon to give the implant elongated bar the best design (N: 4);
- Instruments for bending the compressive bar like manual benders, table benders and metal bar benders for giving it the adequate design before the implantation, and also for allowing the surgeon to make design corrections “in situ” without removing the implanted strut (N: 6, N: 7);
- Tweezers to adjust the periosteal wires;
- Pliers to cut the wires (N: 9);
- Screw drivers. (N: 8).
Procedure
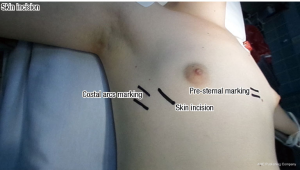
- Marking the skin (Figures 4-7):
- The protruded zone;
- The incisions: sub-mammary incisions in ladies and horizontal incisions on the middle axillary region in males;
- The costal arcs where the wires will be linked;
- Election of the possible length of the compressive bar.
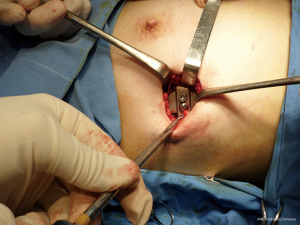
- Anesthetic blockage. Skin incision. Dissection until the costal arcs (Figures 8-10);
- Dissection on both hemi-thoraxes of the costal arcs in a sub-periosteal way (Figures 11,12);
- Introduction of a small size of PVC tube throughout the same way (Figure 13);
- Passage of implantable steel wires throughout these periosteal tubes (Figures 14-18);
- Sub-muscular pocket. Insertion of the fixation plates utilizing the wires and the unthreaded holes of the plate (Figures 19-23);
- Making the pre-sternal passage by means of a long scissors, trocars and a bigger PVC tube. The sub-pectoral location of the bar is ideal. In cases where the protrusion is located in the xiphoid region the bar will remain sub-dermic (Figures 2429);
- Bending the elongated bar helped by the templates (Figures 30-33);
- The bar introduction is helped by the PVC tube (Figures 34,35);
- Manual compression of the bar and linkage between the bar and the fixation plates with screws (Figure 36);
- Slow progression of the pressure of the bar changing the screws on both sides until reaching the desired thoracic contour (Figures 37-42);
- Water check to determine the absence of pleural damage;
- Suture of the muscle and skin layers (Figure 43).





























Role of team members
This technique calls for general anesthesia with endotracheal intubation.
We do not routinely apply epidural anesthesia.
We utilize anesthetic blockade in the intercostal nerve at the start and finish of the operative procedure.
The position of the patient is in dorsal decubitus with both arms abducted.
The surgical nurse is placed at the feet of the patient, allowing two surgeons to work in the hemi-thoraxes.
Given the axillar location of the incisions, the assistant placed in the opposite hemi-thorax limits his/her participation in separating the muscle layers while the other two surgeons proceed to the dissection of the costal arcs and the maneuvers described in the procedure section.
After the costal dissection and placing the fixation plate, as well as passing through the trocar and the PVC tube, the main surgeon moves towards the opposite hemi-thorax and repeats the steps.
Once the PVC tube has been passed, the compressive bar is then inserted through it. Then the surgeon manually compresses the protruded region and the fixation of the bar to the fixation plate begins.
Depending on the degree of the complexity of each case, it may be required that the surgeon moves to both hemi-thoraxes in order to increase the compression and relocates the fixation screws.
Postoperative management
The treatment implemented in the post operatory phase includes analgesic parenteral drugs administration, antibiotic therapy with cefazolin during two days, parenteral hydration and kinetic therapy with rapid ambulation.
Pain is not expected for long periods. The more flexible are the operated thoraxes the less is the pain and easier to be addressed. In those patients with rigid thoraxes the treatment must remain for longer periods.
The expected hospitalization is between three to five days.
During post-operatory period the restrictions of physical efforts and sports activities are less demanding compared to the pectus excavatum surgery by the Nuss procedure. This is because in our procedure there is a steady fixation of the implant in the thoracic wall. However patients are requested to avoid risky activities and refrain from participating in sports that imply contact with others or objects.
In patients with little fatty tissue or those with asymmetric shapes presenting skin compression due to the implanted bar, it is imperative to apply massages in order to avoid dermic adherence. These patients require a more frequent follow-up to detect this potential complication as soon as possible.
A monthly post-operatory control is required during the first three months, and after this period a control is recommended every three months until implant removal.
The expectation is to remove the bar after 2 years, however in patients that have not completed the growth period the bar removal must be evaluated case by case.
A wound or implant trajectory infection is seldom a complication. In an unusually case early removal may be necessary.
With this situation, infectious material must be obtained and cultured. Antibiotic treatment must be initiated according to the germ found. If the infection remains, it must be treated by opening the incision and washing the cavity. The structure implanted should not remain without cover with muscular or dermic layers. The dehiscence of those layers forces the surgeon to re-operate, washing and moving of the layers and recovering the implant.
In these situations we utilize Sulfamethoxazole/Trimethoprim: Bactrim for long periods.
In isolated cases severe trauma cause the release of the fixation plate and the compressive bar. Correction was achieved by re-operating with restoration of the compressive structure.
In a few patients localized growth in the xiphoid region after the implant may cause the cephalic rotation of the implant. This was corrected by re-implanting the strut in a lower area.
Noticeable growth in some patients implanted before puberty may cause the break of the pericostal wires.
Since the organism creates a steady fibrotic structure covering the implant in a few month it is not usually necessary to re-operate on those patients. The compressive element continued performing its function and harmonic growth of the thoracic cage was achieved.
Removal of the implant is a procedure that does not require more than a single day in hospital and does not bring any significant pain.
Tips, tricks and pitfalls
We will address these technical matters bearing in mind the surgical procedure and difficulties or complications that may show up in a post-operative phase.
Marking the skin
The highest protuberance point of the pathology must be chosen to mark the skin. Once a horizontal line is drawn, the two most useful costal arcs must be chosen. We chose the medium axillar region in males; however the sub mammary incision performed on females almost shows an absence of visible scar. The sub mammary incision must be marked with the patient sitting, to determine in them the sub mammary fold with accuracy. This incision does not perfectly match with the region where the fixation plate will be placed, which makes the implant maneuver more complex.
Curettage of the costal arcs
Special attention must be paid to the oblique direction of the costal arcs in the axillar region.
We must then carefully choose the right costal area in order that the pericostal wires put the fixation plates in a perpendicular position to the compressive bar.
The more perfection achieved in this perpendicularity the higher the ease will be in the glide of the compressive bar, and allows the surgeon to achieve the best possible result.
The curettage of the posterior face of the costal arcs must be carefully executed to prevent the pleural breakage and pneumothorax.
Fixation of the plate
The periosteal passage of small caliber PVC tube eases the passing of the wires. The end of the wires to be introduced must be bent and rounded. If they are not rounded during the periosteal journey, they usually perforate the tube and tear the pleura. Afterwards the extremes of the wires must be secured to prevent injuries to the operators.
Pocket for the plate
It is important to allow the fixation plate to remain in a horizontal position so that an adequate lodge will exist to host it.
Placing of the fixation plate
After applying the fixation plate it against the costal layer, the wires are to be adjusted in a loose manner. This allows the glide and union with the screws to be easier. Once the wires and screws are united the adjustment of wires must be tightened. Finally, we proceed to curve and hide them avoiding injury to the skin.
The bar location
The making of the pre-sternal tunnel must be carefully planned. If the sub-pectoral region is chosen the tubes and trocar showed in the videos must be used. The retrosternal zone is the key factor, both in the sub-pectoral as well as the sub-dermic locations where adherence may occur. There is a lack of muscular and fatty tissue in this zone, so the contact with the implant is risky and may provoke adherence and a serum collection. The application of wide skin release and massages prevent those complications.
The bar design
The design of the implant is a key. Considering the lack of body fatty tissue that our patients often have, a fault in the design could cause protuberances and oppression of the bar over the skin. This compression may lead to an adherence process that may include serum, skin blister, the implant exteriorization and infections. The utilization of a template helps the adequate bending of the bar. We must carefully ensure the angle of the thoracic inclination in the anterior axillar region. We must work out the adequate application of the implant after doing the compression of the protrusion. This is different from measuring the angle without thoracic compression. In asymmetries these difficulties may be bigger. The design of the bar for a pectus carinatum correction differs from the pectus excavatum in the Nuss technique. Here the pre-sternal portion of the bar is flat. Minor corrections in both ends of the implant can be done using in situ benders. These instruments avoid the extraction of the implant for these corrections.
Union between the bar and the plate
Utilizing two screws is recommended for the fixation. For the initial coupling screws of a larger size and conical form are used to ease the union. Once achieved, the screws are replaced by others of smaller size.
Post operatory
The massages in the anterior and axillar regions prevent the adherence process. Patients often resist doing massages in a systemic manner. Signs of the adherence process are frequently overlooked. These signs, like changes in the skin color, indicate difficulties in the skin displacement. Thereafter a serum collection appears. This event must be addressed with massages, ice and punctures in case of an inflammatory process. If treated early may provide favorably evolution. If the process is irreversible the bar must be extracted. Between seven and ten months following surgery generally the result does not require a new implant, or the condition can be controlled with an orthesis appliance. In some occasions the compressive bar can be extracted, leaving the fixation plates. After a period between two and three months the bar should be re-installed reinstall the bar. Serum can also appear at the level of the fixation plate. This serum indicates complications of the compression of the periosteal wire. The collection of serum appears when the patients resume physical activities and is well tolerated and successfully treated with ice and anti-inflammatory medication.
Metal allergy
Allergy to metal could appear in between 2% and 4% of the patients. This usually does not call for implant removal. The allergy is characterized by dermatologic alteration in the journey of the bar and responds to corticoid treatments.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Horacio Abramson is owner of an USA patent: “Apparatus for the correction of chest wall deformities such as pectus carinatum and method of using the same”.
References
- Abramson H. A minimally invasive technique to repair pectus carinatum. Preliminary report. Arch Bronconeumol 2005;41:349-51. [PubMed]
- Abramson H, D'Agostino J, Wuscovi S. A 5-year experience with a minimally invasive technique for pectus carinatum repair. J Pediatr Surg 2009;44:118-23. [Crossref] [PubMed]
- Ravitch MM. Operative Correction of Pectus Carinatum (Pigeon Breast). Ann Surg 1960;151:705-14. [Crossref] [PubMed]
- Robicsek F, Sanger PW, Taylor FH, et al. The surgical treatment of chondrosternal prominence (pectus carinatum). J Thorac Cardiovasc Surg 1963;45:691-701. [PubMed]
- Welch KJ, Vos A. Surgical correction of pectus carinatum (pigeon breast). J Pediatr Surg 1973;8:659-67. [Crossref] [PubMed]
- Lester CW. Pigeon breast (pectus carinatum) and other protrusion deformities of the chest of developmental origin. Ann Surg 1953;137:482-9. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Croitoru DP, Kelly RE Jr, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. J Pediatr Surg 2002;37:437-45. [Crossref] [PubMed]
- Abramson H, Aragone X, Blanco JB, et al. Instrumental tools. Asvide 2016;3:116. Available online: http://www.asvide.com/articles/870
- Abramson H, Aragone X, Blanco JB, et al. Skin marking. Asvide 2016;3:117. Available online: http://www.asvide.com/articles/871
- Abramson H, Aragone X, Blanco JB, et al. Costal curettage. Asvide 2016;3:118. Available online: http://www.asvide.com/articles/872
- Abramson H, Aragone X, Blanco JB, et al. Pericostal tube journey. Asvide 2016;3:119. Available online: http://www.asvide.com/articles/873
- Abramson H, Aragone X, Blanco JB, et al. Pericostal wire journey. Asvide 2016;3:120. Available online: http://www.asvide.com/articles/874
- Abramson H, Aragone X, Blanco JB, et al. Second pericostal wire journey. Asvide 2016;3:121. Available online: http://www.asvide.com/articles/875
- Abramson H, Aragone X, Blanco JB, et al. Tip wire protection. Asvide 2016;3:122. Available online: http://www.asvide.com/articles/876
- Abramson H, Aragone X, Blanco JB, et al. Tip wire protection. Asvide 2016;3:123. Available online: http://www.asvide.com/articles/877
- Abramson H, Aragone X, Blanco JB, et al. Water check. Asvide 2016;3:124. Available online: http://www.asvide.com/articles/879
- Abramson H, Aragone X, Blanco JB, et al. Sub-muscular pocket. Asvide 2016;3:125. Available online: http://www.asvide.com/articles/880
- Abramson H, Aragone X, Blanco JB, et al. Sub-muscular pocket. Asvide 2016;3:126. Available online: http://www.asvide.com/articles/881
- Abramson H, Aragone X, Blanco JB, et al. Fixation plate insertion. Asvide 2016;3:127. Available online: http://www.asvide.com/articles/882
- Abramson H, Aragone X, Blanco JB, et al. Fixation plate insertion. Asvide 2016;3:128. Available online: http://www.asvide.com/articles/883
- Abramson H, Aragone X, Blanco JB, et al. Sub-muscular tunnel. Asvide 2016;3:129. Available online: http://www.asvide.com/articles/884
- Abramson H, Aragone X, Blanco JB, et al. Trocar and tube insertion. Asvide 2016;3:130. Available online: http://www.asvide.com/articles/885
- Abramson H, Aragone X, Blanco JB, et al. Trocar removal. Asvide 2016;3:131. Available online: http://www.asvide.com/articles/886
- Abramson H, Aragone X, Blanco JB, et al. Sub-muscular tunnel opposite side. Asvide 2016;3:132. Available online: http://www.asvide.com/articles/887
- Abramson H, Aragone X, Blanco JB, et al. Trocar insertion. Asvide 2016;3:133. Available online: http://www.asvide.com/articles/889
- Abramson H, Aragone X, Blanco JB, et al. A longer tube passage. Asvide 2016;3:134. Available online: http://www.asvide.com/articles/890
- Abramson H, Aragone X, Blanco JB, et al. Template bending. Asvide 2016;3:135. Available online: http://www.asvide.com/articles/891
- Abramson H, Aragone X, Blanco JB, et al. Bar bending 1. Asvide 2016;3:136. Available online: http://www.asvide.com/articles/892
- Abramson H, Aragone X, Blanco JB, et al. Bar bending 2. Asvide 2016;3:137. Available online: http://www.asvide.com/articles/893
- Abramson H, Aragone X, Blanco JB, et al. Bar Bending 3. Asvide 2016;3:138. Available online: http://www.asvide.com/articles/894
- Abramson H, Aragone X, Blanco JB, et al. Bar Insertion. Asvide 2016;3:139. Available online: http://www.asvide.com/articles/895
- Abramson H, Aragone X, Blanco JB, et al. Bar insertion. Asvide 2016;3:140. Available online: http://www.asvide.com/articles/896
- Abramson H, Aragone X, Blanco JB, et al. Bar compression. Asvide 2016;3:141. Available online: http://www.asvide.com/articles/897
- Abramson H, Aragone X, Blanco JB, et al. Final bar bending. Asvide 2016;3:142. Available online: http://www.asvide.com/articles/898
- Abramson H, Aragone X, Blanco JB, et al. First screw insertion. Asvide 2016;3:143. Available online: http://www.asvide.com/articles/899
- Abramson H, Aragone X, Blanco JB, et al. Final wire adjustment. Asvide 2016;3:144. Available online: http://www.asvide.com/articles/900
- Abramson H, Aragone X, Blanco JB, et al. Final wire adjustment. Asvide 2016;3:145. Available online: http://www.asvide.com/articles/901
- Abramson H, Aragone X, Blanco JB, et al. Screw adjusting. Asvide 2016;3:146. Available online: http://www.asvide.com/articles/902
Cite this article as: Abramson H, Aragone X, Blanco JB, Ciano A, Abramson L. Minimally invasive repair of pectus carinatum and how to deal with complications. J Vis Surg 2016;2:64.